East Asian Arch Psychiatry 2016;26:30-8
ORIGINAL ARTICLE
Prof. Abdel-Hady El-Gilany, MD, Public Health, Faculty of Medicine, Mansoura University, Egypt.
Prof. Mohamed Khater, MD, Psychiatry, Faculty of Medicine, Mansoura University, Egypt.
Prof. Zeinab Gomaa, MD, Psychiatry, Faculty of Medicine, Mansoura University, Egypt.
Prof. Elsayed Hussein, MD, Psychiatry, Faculty of Medicine, Mansoura University, Egypt.
Dr Ibrahem Hamdy, MD, Psychiatry, Faculty of Medicine, Mansoura University, Egypt.
Address for correspondence: Prof. Abdel-Hady El-Gilany, Public Health, Faculty of Medicine, Mansoura University, Mansoura 35516, Egypt.
Email: ahgilany@gmail.com
Submitted: 10 July 2015; Accepted: 28 December 2015
Abstract
Objectives: To estimate the overall prevalence of psychiatric disorders among prisoners and its associated factors, and to estimate the prevalence of different mental and personality disorders.
Methods: This was a cross-sectional descriptive study carried out in 16 randomly selected prisons in Egypt. A stratified proportional random sample of 1350 adult prisoners was included in the study. Data were collected by a psychiatrist by direct interview with prisoners. The study questionnaire obtained information about socio-demographics, prisoner circumstances, medical history, psychological factors, legal history of the prisoner as well as the Arabic version of the Structured Clinical Interview for the DSM-IV Axis I and Axis II disorders. Bivariate and logistic regression analyses were performed to determine the significant factors associated with presence of psychiatric disorder.
Results: The overall point prevalence of psychiatric disorders was 22%, excluding substance abuse and alcohol intake. The independent predictors for psychiatric disorders were work in prison (adjusted odds ratio = 0.6), family visits (0.5), substance abuse outside prison (2.7), history of psychiatric disorders outside prison (2.0), and repeated admission to the prison (2.5). The prevalence of mood disorders and psychosis was 3.3% and 1.3%, respectively. The overall prevalence of personality disorders was 13.6%.
Conclusions: Psychiatric disorders are prevalent among prisoners; the most common being personality and antisocial disorders. There is a need for psychiatric assessment of prisoners when first imprisoned and for subsequent regular monitoring and treatment.
Key words: Egypt; Mental disorders; Personality disorders; Prisoners
Introduction
Prison is defined as a facility in which individuals are forcibly confined and denied a variety of freedoms under the authority of the state as a form of punishment.1 Mental health problems are often more apparent in prisons than in the community.2 Correctional institutions are reservoirs of physical and mental illness that constantly spill back into the community. These conditions are public health problems that demand effective management and close coordination among correctional health, community health, and mental health facilities.3 It is only recently that medical and correctional communities realised that the extent of mental diseases, substance use disorders, as well as chronic and communicable diseases is increasing in the correctional system.4 Prisons are places where living conditions can be both physically and psychologically demanding. Concerns about separation from family and friends and future uncertainties are made worse by poor living conditions.5 One of the major health problems in prisons is the mental health assessment and treatment. Correctional employees are often not trained to identify or assist inmates who experience psychiatric symptoms.6
Fazel and Danesh7 reported that 1 in 7 prisoners had a potentially treatable mental illness and 3.7% of men had psychotic illnesses, 10% major depression, and 65% a personality disorder, including 47% with antisocial personality disorder; in women, 4.0% had psychotic illnesses, 12% major depression, and 42% a personality disorder, including 21% with antisocial personality disorder. A recent study in Brazil found that the lifetime and 12-month prevalence of any mental disorder was 68.9% and 39.2% among women and 56.1% and 22.1% among men, respectively.8 In a study in a single prison in Egypt, Abuzaid9 reported that the overall prevalence of psychiatric disorders was 15.3% and the prevalence of psychotic disorders, depression and anxiety disorders was 0.6%, 5.7% and 5.6%, respectively.
Egypt has at least 60,000 prisoners and the number is expected to increase. Despite this, information about prisoners’ health is scarce. In Egypt, apart from a few small-scale studies, the magnitude of psychiatric disorders among prisoners on a national level is unknown. This study aimed to estimate the overall prevalence of psychiatric disorders among prisoners and its associated factors, and to estimate the prevalence of different psychiatric disorders.
Methods
This was a cross-sectional study carried out on a national sample of adult prisoners in Egypt from 1 March 2013 to 28 February 2014. The target population was all prisoners aged 18 to 65 years who spent at least 1 year in prison. Juveniles were excluded as they were incarcerated in correctional facilities rather than prisons. Political prisoners and foreigners were also excluded.
The sample size was calculated using the Epi Info statistical program developed by the Centers for Disease Control and Prevention (www.cdc.gov/epiinfo). The total number of prisoners in Egypt was about 60,000 at the end of 2012. A previous study in one prison in Egypt found that about 15% of prisoners had ≥ 1 psychiatric disorders.9 At 2% precision, 5% confidence level and 80% study power, the estimated sample size was 1200. We added 10% to compensate for defaulters. Thus the final sample size was 1320 prisoners.
The stratified proportional random sampling method was used to select the study population. In Egypt, there are 40 prisons administratively distributed into 3 geographical categories: the Central Region (n = 17), Upper Egypt (n = 5), and Lower Egypt (Delta; n = 18). A list of 16 prisons was selected and provided by the Prisons Sector of the Ministry of Interior to represent different geographical regions and in proportion to the total prisoners in each region (5 from the Central Region, 3 from Upper Egypt and 8 from Delta). Sample size was distributed proportionally according to the total number of prisoners in each prison. Within each prison, the sample prisoners were selected by that prison’s authority. The responsible officer was instructed to choose prisoners by systematic random sampling from the list of prisons in each geographical area. Similarly he was instructed to choose 1 in every 20 prisoners by systematic random sampling from the list of prisoners in each prison. A total of 1357 prisoners were invited to participate in the study, and 1350 of them completed the interview (response rate, 99.5%).
Approval of the Assistant Minister of the Interior for the Prisons Sector, the Public Relation Sector of the Ministry of Interior, and the Directors of the selected prisons was obtained. The study protocol was approved by the Research Ethics Committee of the Faculty of Medicine, Mansoura University, Egypt. Each prisoner gave oral consent before interview. Confidentiality was assured and the prisoner had the right to withdraw from the interview at any time.
Data were collected by the researcher during an interview with each prisoner after agreement with the prison’s director, doctor and / or criminal investigator. The interview was held in the prison hospital, library, or in a private room. For prisoners awaiting execution, the interview was carried out through the window of the door of a highly secured room.
The study questionnaire was in 2 parts. The first part covered the socio-demographic data, prisoner’s circumstances, medical history, psychological factors, and the legal history of the prisoner. The second part was the Structured Clinical Interview for the DSM-IV Axis I and Axis II disorders to diagnose major mental disorders and personality disorders, respectively.10 Each interview lasted about 2 hours. The DSM-IV (Axis I and Axis II) is considered valid for psychiatric diagnosis and is considered the gold standard for psychiatric diagnosis by most psychiatrists in Egypt. The Arabic version has been validated and used by many researchers.11-14
Data were analysed using the Statistical Package for the Social Sciences Windows version 16 (SPSS Inc., Chicago [IL], US). Descriptive statistics were presented as frequencies and percentages. Chi-square test was used to assess the significance between groups. Significant predictors in bivariate analysis were entered into a multivariate logistic regression model using Wald forward method. Odds ratios (ORs) and their 95% confidence intervals were calculated. A p value of ≤ 0.05 was considered statistically significant.
Results
Table 1 shows that the point prevalence rate of ≥ 1 psychiatric disorders in 1350 prisoners was 22%. This was significantly lower among older than younger prisoners (OR = 0.4), working than non-working prisoners (OR = 0.6), and those having family visits than those without (OR = 0.6). On the contrary, the prevalence was significantly higher among prisoners exposed to maltreatment by officers and other prisoners. The prevalence increased significantly among prisoners with substance abuse and psychiatric disorders outside the prison as well as a history of psychiatric disorders inside the prison (Table 2).
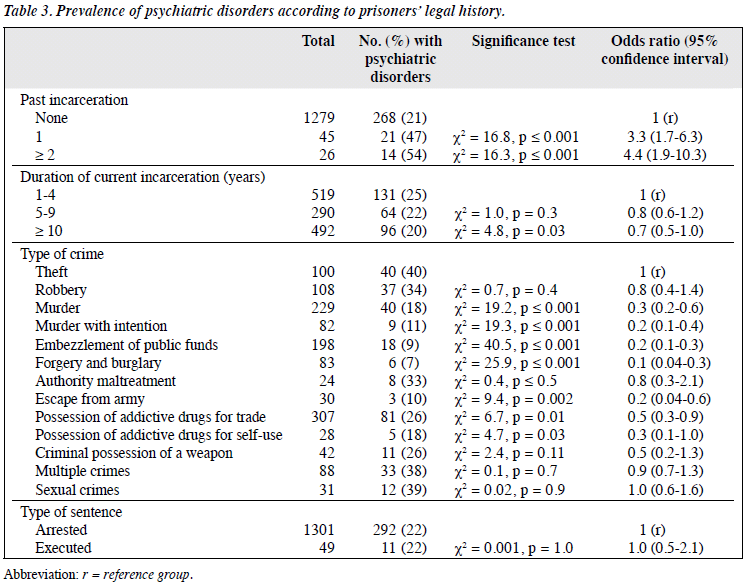
Table 3 reveals that the prevalence of psychiatric disorders increased significantly among prisoners admitted to prison twice and 3 times compared with first admission (OR = 3.3 and 4.4, respectively). The prevalence was significantly lower in prisoners who committed murder (OR = 0.3), murder with intention (OR = 0.2), embezzlement of public funds (OR = 0.2), forgery and burglary (OR = 0.1), and escape from army (OR = 0.2).
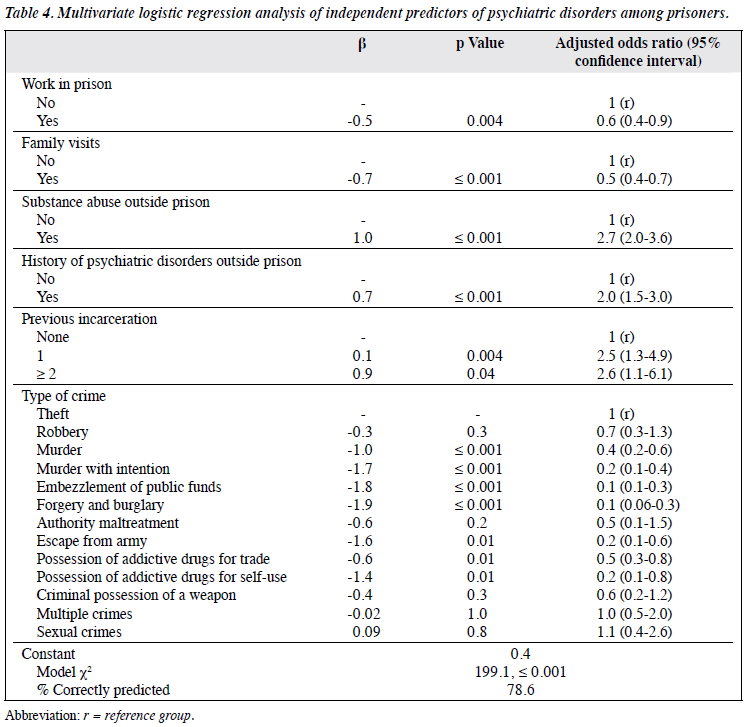
Multivariate logistic regression analysis revealed that the independent predictors of psychiatric disorders were work in prison (adjusted OR [AOR] = 0.6), family visits (AOR = 0.5), substance abuse outside prison (AOR = 2.7), history of psychiatric disorders outside prison (AOR = 2.0), repeated admission to the prison (AOR = 2.5), and some types of crime. p Values for each type of crime is shown in Table 4.
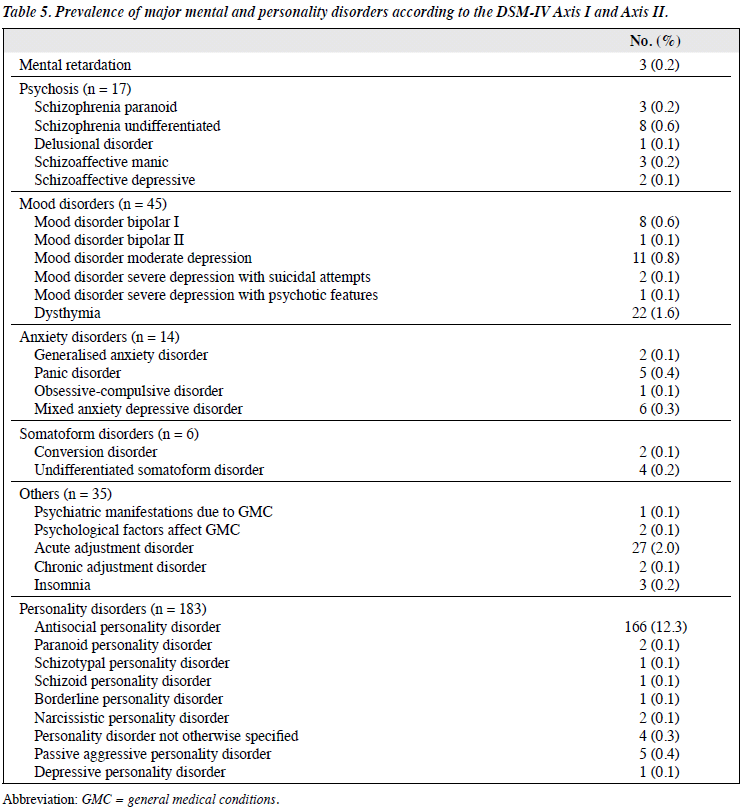
The prevalence of mood disorders and psychosis was 3.3% and 1.3%, respectively. The overall prevalence of personality disorders was 13.6% with antisocial disorder the most prevalent (12.3%) [Table 5].
Discussion
Considerable attention has been given to the increasing prevalence of mental health needs of offenders. Addressing these needs reduces suffering, respects human rights, and provides essential health care services.15 Prevalence estimates of psychiatric disorders in prisoners vary widely depending on methodology, setting, peculiarities of the prison system in each country, and definition of psychiatric disorders used by researchers. This makes comparison difficult. The results based on a standardised diagnostic screening instrument completed by psychiatrists give more accurate results than those based on self-reported symptoms.
We found that 22% of prisoners had ≥ 1 psychiatric disorders, other than substance abuse and alcohol intake at the time of study. Our estimate is higher than the previous report from Egypt. Abuzaid9 found that the overall prevalence of psychiatric disorders was 15.3% in El Kanater prison of Egypt. Previous Egyptian studies examined offenders using a non-structured interview and generated diagnoses according to the Egyptian classification of mental disorders.
In other countries, the prevalence of psychiatric disorders among prisoners varies markedly. Fazel and Danesh7 in their meta-analysis reported that 1 in 7 prisoners has a potentially treatable mental illness. A recent study in Brazil found that the lifetime and 12-month prevalence of any mental disorder was 68.9% and 39.2% among women and 56.1% and 22.1% among men, respectively.8 Higher rates were reported in many countries: 80% in Australia,16 57.2% in Iran,17 55.4% in South Africa,18 51.4% in Turkey,19 43% in Nigeria,20 63.15% in Zambia,21 63% in England and Wales,22 44% to 74% in Australia,23-25 and 64% to 73% in US.26-28 In Nigeria, the prevalence was 57% among male inmates.29 In India, 56.4% of prisoners were suffering from psychiatric illness, excluding substance abuse.30
The reasons why a number of prisoners develop a psychiatric disorder are complex, but there are a number of possible explanations: first, inmates have limited liberty, autonomy, and communication with family and friends. This can be devastating to some inmates and lead to a deterioration in their psychological wellbeing.29 Second, widespread substance abuse over the course of a lifetime renders an individual susceptible to development of a psychiatric disorder and such an individual is more likely to be arrested for drug offences.31 Third, the prison environment, including overcrowding conditions, may have a further detrimental effect on prisoners’ mental health.32 Fourth, the limited resources of community-based care may make individuals with untreated disorders more likely to be arrested. Last but not least, social, demographic, economic, political, environmental, cultural, and religious influences affect the mental health status of people.33
The lower prevalence of psychiatric disorders among prisoners in Egypt could be attributed to a significant degree of sympathy among Egyptian prisoners. Their hard personality traits may make them less susceptible to classic stressors. Those with a long period of incarceration adjust to life inside the prison and consider prison a new home. There is a great amount of coherence in prisons. Many Egyptian biographies have talked about the experience of their authors in prison. Apart from the harsh regimen and difficulties of prisoners’ experience, they also describe coherence and support between inmates that make their time in prison more tolerable. It is possible that prisoners may lack awareness of their own illness and do not think they are sick. The religious programme applied in prisons may influence the onset of and coping with psychiatric disorders. Mandhouj et al34 reported that spirituality and devoutness among detainees is an important means of coping with incarceration and stressful events, and a means of finding inner peace, showing altruism and gaining respect of others. Clear et al35 concluded that religious participation could help an inmate to overcome depression and guilt. It is worth mentioning that the representativeness of the sample is questionable as the list of prisons and prisoners were provided by the prison’s authority.
The lower rate of depressive and anxiety disorders in this study may be explained by the preponderance of males in the sample. Men are confined by many social and cultural bounds that make expression of emotional states difficult.
We found that the prevalence of psychiatric disorders was significantly lower among prisoners who worked inside prisons and those who received visits from their family. Vocational training had a positive significant effect on employment rates after release.36 Prisoners can work in workshops (woodwork, assembly and production). Prison vocational training helps to improve offenders’ efficiency and productivity, and assures a career after release. Furthermore, family support may lessen the burden associated with being in a prison.21
The prevalence of psychiatric disorders was significantly higher among prisoners with substance abuse outside prison, a history of psychiatric disorders, and previous incarceration. The abuse of drugs may have been the reason for imprisonment. It was concluded that most mentally ill individuals in prisons and jails would have been treated before incarceration.37 Many studies agreed that prison inmates with psychiatric disorders are more likely to have had a previous incarceration.17,38-41
We found a different prevalence of psychiatric disorders among offence categories: lower among the offences of forgery and burglary and embezzlement of public funds. The prevalence was highest among prisoners guilty of theft, sexual crimes, and multiple crimes. In Iranian prisoners, psychiatric disorders were less prevalent in the financial offences group.17 Vinkers et al42 concluded that mental disorders are related to type of crime. Pondé et al43 found that psychosis and bipolar disorder were not associated with violent crime.
In this study, gender and age of prisoners were not independent predictors of psychiatric disorders. Previous studies showed contradictory findings. Among Nigerian inmates, psychiatric disorders increased significantly with age.29 A Zambian study found that married prisoners were less likely to have a mental illness than separated / divorced prisoners.21 Effect of gender on occurrence of psychiatric disorders is contradicting. Some studies found more males affected25,44 and others found more females.17,28-45
In this study, the prevalence of mood disorders and psychosis was 3.3% and 1.3%, respectively. The overall prevalence of personality disorders was 13.6% with antisocial disorder the most prevalent (12.3%). Abuzaid9 reported that the prevalence of psychotic disorders was 0.6%. In Kuwait, 25% of prisoners had generalised anxiety disorders.46
In other developing countries such as Nigeria, substance abuse was the most common disorder (48.7%) among male inmates, followed by depression (30.8%), generalised anxiety disorder (11.8%), panic disorder (6.1%), and psychosis (1.2%).29 In South Africa, substance use disorder and depression with anxiety disorder were found in 42.0% and 23.3%, respectively.18 In Zambia, Mayeya et al33 found that the most common mental disorders were acute psychotic episodes, schizophrenia, affective disorders, alcohol-related problems, and organic brain syndromes. In Brazil, the 12-month prevalence of anxious-phobic dis- orders was 27.7% among women and 13.6% among men. The corresponding figures for affective disorders were 21% and 9.9% and for drug-related disorders were 1.6% and 1.3%. For severe mental disorders (psychotic, bipolar disorders, and severe depression) the prevalence was 14.7% among women and 6.3% among men.8 In India, 2.5% of female prisoners had dysthymia and 6.1% had phobia.47
In Australia, 10% of prisoners had attention deficient hyperactivity disorder and behavioural disorders, 6% had substance-related disorders, 5% schizophrenia and other psychotic disorders, 3.5% mood disorders, 15% anxiety disorders, 5% sleep disorders, and 3% personality disorders.25 Other studies reported a rate of 31% for mental disorders including drug and alcohol abuse.45,48 Also a higher rate of 80% for mental disorders was reported from New South Wales.16 In the US, 50% of inmates had anxiety disorders and more than one-third had affective disorders.28 In French prisons for men, 21.4% had mood disorders, 21.2% had anxiety disorders, 14% had substance-related disorders, and 12.1% had psychotic disorders.49
In a systematic review of 62 surveys from 12 countries, Fazel and Danesh7 found that 3.7% of men had psychotic illness, 10% had major depression, and 65% had personality disorders. The corresponding figures for women were 4%, 12%, and 42%. In a meta-analysis of 109 studies including 33,588 prisoners in 24 countries, Fazel and Seewald50 found that the pooled prevalence of psychosis and major depression was 3.7% and 11.4%, respectively. Studies from low- and middle-income countries reported a higher prevalence of psychosis.
The prevalence of psychiatric morbidity observed in this study is in its early expanding phase. Urgent attention is required to reduce the burden of psychiatric disorders. Special attention should be given to prisoners at higher risk, e.g. frequent incarceration, psychiatric history, and substance abuse outside prison. More family visits and work in prison could decrease the likelihood of developing a psychiatric condition. A national representative sample of prisoners is needed to give the actual picture of mental illness in this group. There is a need to formulate a policy favourable to prisoners with psychiatric disorders. These prisoners require complex treatment, services, and supervision strategies that jails are not designed or equipped to provide. Treatment of psychiatric disorders before discharge may decrease the probability of re-offending and returning to prison.
Strengths and Limitations
This is the first large-scale national study of psychiatric disorders among prisoners in Egypt carried out by psychiatrists using a standardised diagnostic tool. It gives an overview of these problems and their associated factors. Despite this, the study has a few limitations. The first is the validity of giving consent and answers to the questionnaire under prison conditions. Written consent will be more ethical than verbal consent in prison conditions. Nonetheless, it is common in Egypt to obtain written consent only for invasive procedures. The second limitation is the uncertainty of external validity of the results. The prevalence of psychiatric disorders may be underestimated. The sample of prisons and prisoners within each prison was provided by the Ministry of Interior. The representativeness of these samples cannot be assured despite detailed instructions given to the officers responsible for sample selection. The third limitation is that the study did not assess the severity or duration of psychiatric disorders, nor the pattern of mental health care. The fourth limitation is that substance and alcohol abuse as well as sexual disorders were not assessed because these are prohibited and will be denied by prisoners. Lastly, as a cross-sectional study, we were unable to make causal inference on whether being in prison causes psychiatric disorders since there was no psychiatric screening prior to imprisonment.
Declaration
The authors declared no conflicts of interest in this study.
References
- Welch M. A social history of punishment and corrections. In: Corrections: a critical approach. New York: McGraw-Hill; 2004: 26-7.
- Australian Institute of Health and Welfare (AIHW). The health of Australia’s prisoners 2009. Canberra: AIHW; 2010.
- Beck AJ, Maruschak LM. Bureau of Justice Statistics special report: mental health treatment in State Prisons, 2000. Available from: http://www.bjs.gov/content/pub/pdf/mhtsp00.pdf. Accessed 22 Nov 2014.
- Wolff N, Plemmons D, Veysey B, Brandli A. Release planning for inmates with mental illness compared with those who have other chronic illnesses. Psychiatr Serv 2002;53:1469-71.
- International Committee of the Red Cross. Health in prisons. Available from: https://www.icrc.org/eng/what-we-do/health/health-prisons/overview-health-in-prisons.htm. Accessed 22 Nov 2014.
- World Health Organization Regional Office for Europe. Health in prisons. A WHO guide to the essentials in prison health. Copenhagen, Denmark: WHO Regional Office; 2007.
- Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet 2002;359:545-50.
- Andreoli SB, Dos Santos MM, Quintana MI, Ribeiro WS, Blay SL, Taborda JG, et al. Prevalence of mental disorders among prisoners in the state of Sao Paulo, Brazil. PLoS One 2014;9:e88836.
- Abuzaid M. Psychiatric disorders in prisoners [thesis]. Faculty of Medicine, Ain Shams University, Egypt; 1995.
- Dreessen L, Hildebrand M, Arntz A. Patient-informant concordance on the Structured Clinical Interview for DSM-III-R personality disorders (SCID-II). J Pers Disord 1998;12:149-61.
- Okasha T, Hatata H, Asaad T, Hamed A, Yousef M. Dual diagnosis in substance abuse [thesis]. Department of Psychiatry, Faculty of Medicine, Ain Shams University, Egypt; 2003.
- El-Missiry A. Homicide in psychiatric illness [thesis]. Department of Psychiatry, Faculty of Medicine, Ain Shams University, Egypt; 2004.
- El-Serafi D. Psychiatric morbidity and coping strategies in a sample of Egyptian cancer female patients [thesis]. Department of Psychiatry, Faculty of Medicine, Ain Shams University, Egypt; 2008.
- El-Hadidy MA. Schizophrenia with and without homicide: a clinical comparative study. J Forensic Psychiatry Psychol 2012;23:95-107.
- Ogloff JR. Identifying and accommodating the needs of mentally ill people in jails and prisons. Psychiatry Psychol Law 2002;9:1-33.
- Butler T, Andrews G, Allnutt S, Sakashita C, Smith NE, Basson J. Mental disorders in Australian prisoners: a comparison with a community sample. Aust N Z J Psychiatry 2006;40:272-6.
- Assadi SM, Noroozian M, Pakravannejad M, Yahyazadeh O, Aghayan S, Shariat SV, et al. Psychiatric morbidity among sentenced prisoners: prevalence study in Iran. Br J Psychiatry 2006;188:159-64.
- Naidoo S, Mkize DL. Prevalence of mental disorders in a prison population in Durban, South Africa. Afr J Psychiatry (Johannesbg) 2012;15:30-5.
- Kugu N, Akyuz G, Dogan O. Psychiatric morbidity in murder and attempted murder crime convicts: A Turkey study. Forensic Sci Int 2008;175:107-12.
- Mafullul YM. A psychosocial study of convicted homicide offenders in a Northern Nigerian prison [unpublished thesis]. West African College of Physician, Nigeria; 1997.
- Nseluke MT, Siziya S. Prevalence and socio-demographic correlates for mental illness among inmates at Lusaka Central Prison, Zambia. Med J Zambia 2011;38:3-7.
- Brooke D, Taylor C, Gunn J, Maden A. Point prevalence of mental disorder in unconvicted male prisoners in England and Wales. BMJ 1996;313:1524-7.
- Butler T, Allnutt S. Mental illness among New South Wales prisoners. Sydney: NSW Corrections Health Service; 2003.
- Ogloff JR, Davis MR, Rivers G, Ross S. The identification of mental disorders in the criminal justice system. Australia: Melbourne University Press; 2006.
- Forsythe L, Gaffney A. Mental disorder prevalence at the gateway of the criminal justice system. Trends and issues in crime and criminal justice no. 438. Canberra: Australian Institute of Criminology; 2012.
- Abt Associates, Inc. Conditions of confinement: juvenile detention and corrections facilities. Washington, D.C.: Office of Juvenile Justice and Delinquency Prevention; 1994.
- James DJ, Glaze LE. Mental health problems of prison and jail inmates. Washington: Bureau of Justice Statistics, U.S. Department of Justice; 2006.
- Trestman RL, Ford J, Zhang W, Wiesbrock V. Current and lifetime psychiatric illness among inmates not identified as acutely mentally ill at intake in Connecticut’s jails. J Am Acad Psychiatry Law 2007;35:490-500.
- Armiya’u AY, Obembe A, Audu MD, Afolaranmi TO. Prevalence of psychiatric morbidity among inmates in Jos maximum security prison. Open J Psychiatry 2013;3:12-7.
- Goyal SK, Singh P, Gargi PD, Goyal S, Garg A. Psychiatric morbidity in prisoners. Indian J Psychiatry 2011;53:253-7.
- Abram KM, Teplin LA. Co-occurring disorders among mentally ill jail detainees. Implications for public policy. Am Psychol 1991;46:1036- 45.
- Steering Committee for the Review of Government Service Provision. Report on Government Services 2012. Canberra: productivity Commission; 2012.
- Mayeya J, Chazulwa R, Mayeya PN, Mbewe E, Magolo LM, Kasisi F, et al. Zambia mental health country profile. Int Rev Psychiatry 2004;16:63-72.
- Mandhouj O, Aubin HJ, Amirouche A, Perroud NA, Huguelet P. Spirituality and religion among French prisoners: an effective coping resource? Int J Offender Ther Comp Criminol 2013;58:821-34.
- Clear TR, Stout BD, Dammer HR, Kelly L, Hardyman PL, Shapiro C. Does involvement in religion help prisoners adjust to prison? The National Council on Crime and Delinquency NCCD Focus; November 1992.
- Skinner BA. To what extent does prisoners’ mental illness undermine programming effectiveness [thesis]? The University of Iowa; Dec 2010. Available from: http://ir.uiowa.edu/etd/887. Accessed 8 Dec 2014.
- Torrey EF, Kennard SA, Eslinger SD, Lamb R, Pavle J. More mentally ill persons are in jails and prisons than hospitals: a survey of the States. National Sheriffs’ Associations / Treatment Advocacy Center; 2010.
- Mallik-Kane K, Visher CA. Health and prisoner reentry: how physical, mental, and substance abuse conditions shape the process of reintegration: research report, Feb 2008. Washington D.C.: Urban Institute Justice Policy Center; 2008.
- Baillargeon J, Binswanger IA, Penn JV, Williams BA, Murray OJ. Psychiatric disorders and repeat incarcerations: the revolving prison door. Am J Psychiatry 2009;166:103-9.
- Willging CE, Malcoe LH, St Cyr S, Zywiak WH, Lapham SC. Behavioral health and social correlates of reincarceration among Hispanic, Native American, and white rural women. Psychiatr Serv 2013;64:590-3.
- Blank Wilson A, Draine J, Barrenger S, Hadley T, Evans A Jr. Examining the impact of mental illness and substance use on time till re-incarceration in a county jail. Adm Policy Ment Health 2014;41:293- 301.
- Vinkers DJ, de Beurs E, Barendregt M, Rinne T, Hoek HW. The relationship between mental disorders and different types of crime. Crim Behav Ment Health 2011;21:307-20.
- Pondé MP, Caron J, Mendonça MS, Freire AC, Moreau N. The relationship between mental disorders and types of crime in inmates in a Brazilian prison. J Forensic Sci 2014;59:1307-14.
- Steadman HJ, Osher FC, Robbins PC, Case B, Samuels S. Prevalence of serious mental illness among jail inmates. Psychiatr Serv 2009;60:761- 5.
- Australian Bureau of Statistics. National Health Survey: summary of results, 2007-2008 (reissue). Available from: http://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0. Accessed 8 Dec 2014.
- Fido A, al-Jabally M. Presence of psychiatric morbidity in prison population in Kuwait. Ann Clin Psychiatry 1993;5:107-10.
- Math SB, Murthy P, Parthasarathy R, Naveen Kumar C, Madhusudhan S. Mental health and substance use problems in prisons: local lessons for national action. Bangalore, India: National Institute of Mental Health Neuro Sciences; 2011.
- Australian Institute of Health and Welfare (AIHW). The mental health of prison entrants in Australia: 2010. AIHW Bulletin no. 104; June 2012.
- Falissard B, Loze JY, Gasquet I, Duburc A, de Beaurepaire C, Fagnani F, et al. Prevalence of mental disorders in French prisons for men. BMC Psychiatry 2006;6:33.
- Fazel S, Seewald K. Severe mental illness in 33,588 prisoners worldwide: systematic review and meta-regression analysis. Br J Psychiatry 2012;200:364-73.