East Asian Arch Psychiatry 2025;35:32-6 | https://doi.org/10.12809/eaap2507
ORIGINAL ARTICLE
Vu Son Tung, Tran Nguyen Ngoc, Le Thi Thanh Huyen, Ngo Tuan Khiem, Nguyen Thi Thu Hang, Nguyen Thi Ai Van, Nguyen Thi Thanh Dat, Nguyen Phuong Linh, Nguyen Thi Ngoc, Kim Thi Linh, Dang Thi Mai
Abstract
Objectives: To identify factors associated with treatment non-adherence among patients with bipolar disorder in Vietnam.
Methods: Outpatients with bipolar disorder receiving treatment at the Bach Mai Hospital, Vietnam between November 2023 and August 2024 were recruited using convenience sampling. Medication adherence was measured using the eight-item Morisky Medication Adherence Scale (MMAS-8). The adherence and non-adherence groups were compared. Generalised multiple linear regression was conducted to assess the effects of relevant factors on the MMAS-8 score. Logistic regression analysis was conducted to identify factors associated with non-adherence.
Results: Of 121 patients with bipolar disorder included in the analysis, 53 (43.8%) were classified as treatment adherence and 68 (56.2%) as non-adherence. In the multivariable analysis, non-adherence status was positively associated with male sex (odds ratio [OR] = 5.837, p = 0.006), lower education level (OR = 3.587, p = 0.023), and receipt of >2 medications (OR = 6.832, p = 0.002), and negatively associated with married status (OR = 0.149, p = 0.002) and family encouragement (OR = 0.214, p = 0.024). In the non-adherence group, MMAS-8 scores were negatively correlated with male sex (β = -0.565, p = 0.001), distance to the clinic (β = -0.002, p = 0.038), and number of medications (β = -1.927, p = 0.030), and positively correlated with family companion during examinations (β = 0.598, p = 0.016), family reminders to take medication (β = 0.585, p = 0.019), and family management of medication (β = 0.636, p = 0.036).
Conclusion: Among patients with bipolar disorder, treatment non-adherence is associated with male sex and number of prescribed medications. Family support is important for treatment adherence; efforts to foster family involvement may improve treatment adherence.
Key words: Bipolar disorder; Family support; Medication adherence; Patient compliance; Vietnam
Vu Son Tung, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Tran Nguyen Ngoc, Department of Psychiatry, Hanoi Medical University, Hanoi, Vietnam
Le Thi Thanh Huyen, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Ngo Tuan Khiem, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Nguyen Thi Thu Hang, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Nguyen Thi Ai Van, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Nguyen Thi Thanh Dat, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Nguyen Phuong Linh, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Nguyen Thi Ngoc, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Kim Thi Linh, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Dang Thi Mai, Department of Mood Disorders, National Institute of Mental Health, Hanoi, Vietnam
Address for correspondence: Dr Tran Nguyen Ngoc, Department of Psychiatry, Hanoi Medical University, Hanoi, Vietnam. Email: trannguyenngoc@hmu.edu.vn
Submitted: 22 January 2025; Accepted: 6 March 2025
Introduction
Bipolar disorder is characterised by recurrent episodes of mania, hypomania, depression, and mixed emotional states.1 The average lifetime prevalence of bipolar disorder is estimated to be 1% but can exceed 5% when the entire bipolar spectrum is included.2 Between 1990 and 2019, bipolar disorder was the sixth most significant cause of disability among people aged 15 to 44 years.3 Bipolar disorder incurs an annual cost of US$202 billion including both direct and indirect treatment expenditures. Direct expenditures amount to approximately US$46 billion and comprise inpatient treatment, emergency room examinations, and outpatient consultation, whereas indirect expenditures represent 72% of total expenses and encompass unemployment, diminished production, and carer stress.3,4
Treatments for mood disorders include pharmaceuticals, electrically induced seizures, magnetic stimulation of the brain, and psychotherapy. Treatment adherence strongly affects the success of pharmacotherapy, but non-adherence is common among people with bipolar disorder. Approximately 20% to 60% of patients with bipolar disorder exhibit inadequate adherence or non-adherence to recommended pharmacotherapy.5 Nearly 30% of hospital admissions are attributable to medication non- adherence.6,7 Non-adherence reduces the ability to work while increasing recurrence, hospitalisation, and suicide rates.8 Non-adherence is associated with sex, age, ethnicity, education level, alcoholism, concomitant mood disorders, manic episodes, and severity of depressive episodes.9 Main reasons for non-adherence include financial constraints (41%), distance from healthcare facilities (35%), and perceived symptom improvement (28%); other factors include adverse medication effects, missed doses, lack of caregiver support, insufficient understanding of bipolar disorder, and work-related demands.10 This study aimed to identify factors associated with treatment non-adherence among patients with bipolar disorder in Vietnam.
Methods
Outpatients with bipolar disorder receiving treatment at the Bach Mai Hospital, Vietnam between November 2023 and August 2024 were recruited using convenience sampling. Patients were excluded if they had medical conditions affecting cerebral function, brain lesions, a history of substance abuse or addiction or use of psychoactive substances, were unable to comprehend or respond during assessments, or were unable to adhere to the research protocol. The diagnosis of bipolar disorder (F31.0-F31.7) was made in accordance with the ICD-10 guidelines.
Medication adherence was measured using the eight-item Morisky Medication Adherence Scale (MMAS-8).11 The MMAS-8 has been used to evaluate patients with chronic conditions such as hypertension, diabetes, asthma, schizophrenia, and bipolar disorder.12,13 The validated Vietnamese version has a Cronbach’s alpha of 0.60 and reliability of 0.62 (95% confidence interval = 0.22-0.81).14 The cut-off score for non-adherence was defined as <8 points.12 Patient demographics and clinical characteristics were collected using a self-administered questionnaire. Family support was assessed using four yes-or-no questions: (1) Do you often have family members accompany you to see a doctor and get your monthly medication? (2) Does your family manage your daily medication? (3) Do your family members regularly give you medication or remind you to take medication every day? (4) Do you feel that you receive encouragement, sympathy, and psychological support from your family members?
Sample size calculation was based on the reported prevalence of treatment adherence (40.6%) among adult patients in a previous study,8 with a precision rate of 10% and a 95% confidence interval. The required sample size was estimated to be 92. The adherence and non-adherence groups were compared using the Student’s t test or the Mann- Whitney U test for continuous variables and the Chi-squared test for categorical variables. Generalised multiple linear regression was conducted to assess the effects of relevant factors on the MMAS-8 score, which was the dependent variable in the non-adherence group. Logistic regression analysis was conducted to identify factors associated with non-adherence. Statistical analyses were performed using SPSS (Mac version 29.0; IBM Corp, Armonk [NY], United States). All tests were two-sided, and a p value of <0.05 was considered statistically significant.
Results
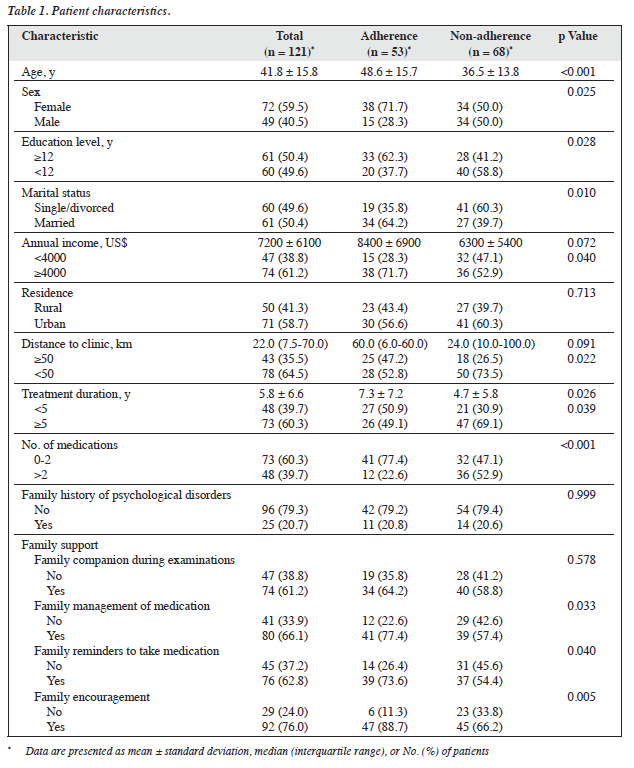
Of 121 patients with bipolar disorder included, 53 (43.8%) were classified as treatment adherence and 68 (56.2%) as non-adherence (Table 1). The non-adherence group tended to include those who were male (p = 0.025), younger (p < 0.001), unmarried (p = 0.010), and had lower education levels (p = 0.028) and lower income levels (p = 0.040), whereas the adherence group had higher a prevalence of family support including family management of medication (p = 0.033), family reminders to take medication (p = 0.040), and family encouragement (p = 0.005).
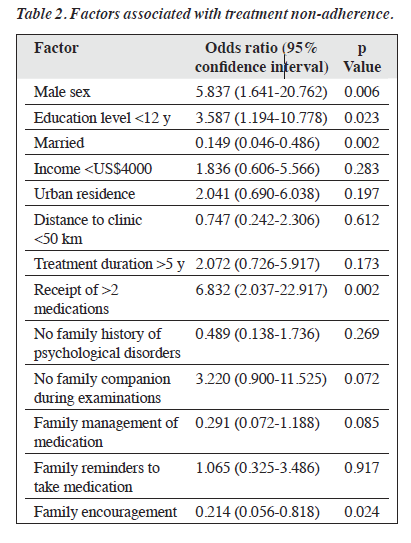
In the multivariable analysis, non-adherence status was positively associated with male sex (odds ratio [OR] = 5.837, p = 0.006), lower education level (OR = 3.587, p = 0.023), and receipt of >2 medications (OR = 6.832, p = 0.002), and negatively associated with married status (OR = 0.149, p = 0.002) and family encouragement (OR = 0.214, p = 0.024) [Table 2].
In the non-adherence group, MMAS-8 scores were negatively correlated with male sex (β = -0.565, p = 0.001), distance to the clinic (β = -0.002, p = 0.038), and number of medications (β = -1.927, p = 0.030), and positively correlated with family companion during examinations (β = 0.598, p = 0.016), family reminders to take medication (β = 0.585, p = 0.019), and family management of medication (β = 0.636, p = 0.036) [Table 3].
Discussion
Female patients demonstrated higher treatment adherence, compared with male patients, consistent with previous findings.15 Healthcare professionals should focus efforts on male patients regarding medication adherence and its health implications. Higher education levels and married status were associated with higher treatment adherence, consistent with a previous studies.8,16 Patient knowledge of the disorder including risk factors, warning signs, and preventive measures correlates with their education levels. Married individuals exhibit higher treatment adherence, compared with single or unmarried counterparts.17,18 Involvement of family members in patient care, follow-up visit, reminders to take medication contributes to treatment adherence.
In the non-adherence group, a higher number of prescribed medications was negatively correlated with MMAS-8 score. Increased numbers and frequencies of medications taken per day result in higher non-adherence rates.19,20 Patients may experience difficulty monitoring their medication intake, which leads to forgetfulness, particularly among older patients. Physicians should consider this when prescribing multiple medications to patients with bipolar disorder.
Family support plays an important role in treatment adherence. Patients who lack family and social support have lower adherence.17,21-23 Families in Vietnam are more closely connected and interactive than those in Western countries. The collectivist nature of Vietnamese culture emphasises familial duty and interdependence, fostering a sense of responsibility among family members to support their loved ones managing their illnesses. This cultural framework can create a structured and supportive environment that reinforces treatment adherence. Family members provide reassurance, reduce feelings of isolation, and offer psychological support, all of which can enhance patient motivation to adhere to prescribed treatment regimens. Families often assume an active role in reminding patients to take medication and attend psychiatric consultations, thereby mitigating the risk of missed doses or therapy sessions. Additionally, mental health stigma often deters individuals from seeking or adhering to treatment. Strong family support can help normalise mental healthcare, encourage open discussions, and reinforce the importance of adherence. Family members can recognise early warning signs of mood episodes and intervene promptly, decreasing the likelihood of relapse or hospitalisation. Families can also provide financial support, ensure transportation to medical appointments, and assist with daily responsibilities, thereby reducing barriers to adherence.
The study had several limitations. First, the generalisability of the findings may be limited due to the small sample size in a single hospital. Second, medication adherence was assessed using a self-administered questionnaire; no objective tests for serum drug levels were performed. Third, other factors that may affect medication adherence were not assessed. Fourth, selection biases may have been present, because individuals who consented to participate were more likely to adhere to treatment. Fifth, patients experiencing various phases of bipolar disorder, including manic, depressive, and remission states, were included. Mental states can affect treatment adherence, but our analysis did not adjust for this confounder. Sixth, causality could not be established due to the cross-sectional nature of the study.
Conclusion
Among patients with bipolar disorder, treatment non- adherence is associated with male sex and number of prescribed medications. Family support is important for treatment adherence; efforts to foster family involvement may improve treatment adherence.
Contributors
All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding / support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
All data generated or analysed during the present study are available from the corresponding author on reasonable request.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki. The patients provided written informed consent for all treatments and procedures and for publication.
References
- Loots E, Goossens E, Vanwesemael T, Morrens M, Van Rompaey B, Dilles T. Interventions to improve medication adherence in patients with schizophrenia or bipolar disorders: a systematic review and meta- analysis. Int J Environ Res Public Health 2021;18:10213. Crossref
- Mousavi N, Norozpour M, Taherifar Z, Naserbakht M, Shabani A. Bipolar I disorder: a qualitative study of the viewpoints of the family members of patients on the nature of the disorder and pharmacological treatment non-adherence. BMC Psychiatry 2021;21:83. Crossref
- Aghababaie-Babaki P, Malekpour MR, Mohammadi E, et al. Global, regional, and national burden and quality of care index (QCI) of bipolar disorder: a systematic analysis of the Global Burden of Disease Study 1990 to 2019. Int J Soc Psychiatry 2023;69:1958-70. Crossref
- Dembek C, Mackie deMauri, Modi K, Zhu Y, Niu X, Grinnell T. The economic and humanistic burden of bipolar disorder in adults in the United States. Ann Gen Psychiatry 2023;22:13. Crossref
- Levin JB, Aebi ME, Howland M, et al. The relationship between medication attitudes and medication adherence behavior in adults with bipolar disorder. J Nerv Ment Dis 2020;208:87-93. Crossref
- McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 2002;36:1331-6. Crossref
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487-97. Crossref
- Selvakumar N, Menon V, Kattimani S. A cross-sectional analysis of patterns and predictors of medication adherence in bipolar disorder: single center experience from South India. Clin Psychopharmacol Neurosci 2018;16:168-75. Crossref
- Bates JA, Whitehead R, Bolge SC, Kim E. Correlates of medication adherence among patients with bipolar disorder: results of the Bipolar Evaluation of Satisfaction and Tolerability (BEST) Study: a nationwide cross-sectional survey. Prim Care Companion J Clin Psychiatry 2010;12:PCC.09m00883. Crossref
- Tesfay K, Girma E, Negash A, Tesfaye M, Dehning S. Medication non- adherence among adult psychiatric outpatients in Jimma University Specialized Hospital, Southwest Ethiopia. Ethiop J Health Sci 2013;23:227-36. Crossref
- 1 Culig J, Leppée M. From Morisky to Hill-bone; self-reports scales for measuring adherence to medication. Coll Antropol 2014;38:55-62.
- De Las Cuevas C, Peñate W. Psychometric properties of the eight- item Morisky Medication Adherence Scale (MMAS-8) in a psychiatric outpatient setting. Int J Clin Health Psychol 2015;15:121-9. Crossref
- Moharamzad Y, Saadat H, Nakhjavan Shahraki B, et al. Validation of the Persian version of the 8-item Morisky Medication Adherence Scale (MMAS-8) in Iranian hypertensive patients. Glob J Health Sci 2015;7:173-83. Crossref
- Nguyen T, Cao HTK, Quach DN, et al. The Vietnamese version of the Brief Illness Perception Questionnaire and the Beliefs about Medicines Questionnaire: translation and cross-cultural adaptation. Trop Med Int Health 2019;24:1465-74. Crossref
- Gutiérrez-Rojas L, Martínez-Ortega JM, Pérez-Costillas L, Jiménez- Fernández S, Carretero MD, Gurpegui M. Illness insight and medication adherence among patients with bipolar disorder. J Nerv Ment Dis 2020;208:481-7. Crossref
- Schoeyen HK, Birkenaes AB, Vaaler AE, et al. Bipolar disorder patients have similar levels of education but lower socio-economic status than the general population. J Affect Disord 2011;129:68-74. Crossref
- Miklowitz DJ. The role of the family in the course and treatment of bipolar disorder. Curr Dir Psychol Sci 2007;16:192-6. Crossref
- Grover S, Nehra R, Thakur A. Bipolar affective disorder and its impact on various aspects of marital relationship. Ind Psychiatry J 2017;26:114-20. Crossref
- Depp CA, Lebowitz BD. Enhancing medication adherence. Psychiatry Edgmont 2007;4:22-32.
- Sajatovic M, Levin J, Fuentes-Casiano E, Cassidy KA, Tatsuoka C, Jenkins JH. Illness experience and reasons for nonadherence among individuals with bipolar disorder who are poorly adherent with medication. Compr Psychiatry 2011;52:280-7. Crossref
- Levin JB, Krivenko A, Howland M, Schlachet R, Sajatovic M. Medication adherence in patients with bipolar disorder: a comprehensive review. CNS Drugs 2016;30:819-35. Crossref
- Wang D, Ma J, Tan L, et al. Characteristics of help-seeking behavior among bipolar disorder patients: a study in Hunan, China. Medicine (Baltimore) 2019;98:e17687. Crossref
- Zhang X, Zhao M, Li J, et al. Associations between family cohesion, adaptability, and functioning of patients with bipolar disorder with clinical syndromes in Hebei, China. J Int Med Res 2019;47:6004-15. Crossref