East Asian Arch Psychiatry 2017;27:91-6
ORIGINAL ARTICLE

Dr Chih-Kang Chen, MD, Department of ?Psychiatry, Tri-Service General Hospital, Taipei, Taiwan.
Dr Hsu-Han Su, MD, Department of Psychiatry, MacKay Memorial Hospital, Hsinchu, Taiwan.
Dr I-Wen Sun, MD, Department of Psychiatry, MacKay Memorial Hospital, Taipei, Taiwan.
Address for correspondence: Dr I-Wen Sun, Department of Psychiatry, MacKay Memorial Hospital, No. 92, Sec. 2, Zhongshan North Road, Taipei City 10449, Taiwan.
Tel: (886) 920933998; Fax (886) 28275622; Email: bz1170@yahoo.com.tw
Submitted: 19 July 2016; Accepted: 20 March 2017
Abstract
Objectives: This survey aimed to understand the attitude of psychiatrists and their use of commonly prescribed second-generation antipsychotics (SGAs) for the treatment of schizophrenia in Taiwan. It also attempted to identify the factors that might influence their preference for selecting SGAs.
Methods: Psychiatrists were interviewed face-to-face using a structured questionnaire. The questionnaire addressed various issues involved in the treatment of patients with schizophrenia, including the reasons for selecting SGAs, psychiatrists??/span> level of satisfaction with commonly prescribed SGAs, and their current use of SGAs in clinical practice.
Results: Gender and age of the psychiatrists, and practice setting were not related to SGA selection. The selection of a SGA might be influenced by characteristics of the psychiatrist, properties of the drugs, and the healthcare insurance system. Most psychiatrists agreed that the performance of brand-name drugs was superior to that of generic drugs. Better symptom control, improvement in cognition, and higher tolerability were among the major factors considered by psychiatrists in Taiwan when prescribing antipsychotics.
Conclusion: Selection of a SGA in Taiwan is potentially influenced by the characteristics of the psychiatrist, properties of the drug, and the healthcare insurance system. Efficacy and tolerability were among the major determining factors when prescribing antipsychotics for the treatment of patients with schizophrenia.
Key words: Antipsychotic agents; Choice behavior; Drugs, generic; Health surveys; Schizophrenia
Introduction
Schizophrenia is a chronic, severe, and disabling mental illness.1 Characteristic symptoms involve a range of cognitive, behavioural, and emotional dysfunctions that are associated with impaired occupational or social functioning.2 The first-generation antipsychotics (FGAs) and second-generation antipsychotics (SGAs) remain the cornerstone of treatment in the acute phase as well as for long-term maintenance therapy.3 The goals of treatment are to promptly reduce symptom severity in the acute phase and improve patient functioning during maintenance therapy, while avoiding the cost as a result of increased adverse effects such as extrapyramidal symptoms or metabolic syndromes. Although the superiority of SGAs over FGAs remains controversial during different stages of treatment, it is important to note that SGAs do not represent a homogeneous class of drugs.2,4
The complex relationship between the patient, his / her illness, the doctor, and the medications greatly influence drug selection, dosage, tolerability, and treatment outcome.5
Psychiatrist-related factors that influence selection of antipsychotics include attitude towards, knowledge of, and experience with the medications.6 Drug selection is also frequently guided by other factors such as cost and local paradigms.7-9
The first popular SGA, risperidone, was introduced in Taiwan in 1997. Paliperidone was the last SGA launched in 2008. Taiwan’s Bureau of National Health Insurance (TBNHI), established in 1995, is the major payer of medical expenditure. It currently covers 99% of the Taiwanese population, and 93% of all healthcare facilities are contracted by the TBNHI, making medical care highly accessible for the general public.10 Among commonly prescribed SGAs, the TBNHI-reimbursed risperidone 2 to 6 mg/day is the cheapest with a daily cost of US$0.7- 2.0, followed by amisulpride 400 to 800 mg (US$2.3-4.5), paliperidone 3 to 12 mg (US$2.9-8.5), olanzapine 10 to 20 mg (US$3.7-7.5), aripiprazole 15 to 30 mg (US$4.6-7.2), and quetiapine 800 to 1200 mg (US$6.1-7.5).
Little is known, however, about preferences of the psychiatrists in Taiwan for individual antipsychotics and the factors affecting their selections. This is the first survey that explored psychiatrists’ attitude towards and use of commonly prescribed SGAs and FGAs in Taiwan for the treatment of schizophrenia. It also attempted to identify the factors that might influence psychiatrists’ preference for certain antipsychotic agents.
Methods
Subjects and Study Procedure
A total of 161 attending psychiatrists, who were selected by the database from their practising hospital, e.g. specialists of psychopharmacology and those experienced in prescribing various antipsychotics were invited to participate in this study from October 2014 to June 2015. Geographical coverage included northern, central, and southern Taiwan. Psychiatrists were interviewed face-to-face using a structured questionnaire. The structured questionnaire addressed various issues involved in the treatment of patients with schizophrenia, including the psychiatrists’ reasons for selecting certain antipsychotics, level of satisfaction with commonly prescribed antipsychotics, and current use of specific antipsychotic agents in their clinical practice. In addition, a series of 6 questions were designed to investigate psychiatrists’ attitude regarding the use of antipsychotics in treating patients with schizophrenia. Their response to each question was rated using a 10-point Likert scale with a score of 1 to 10 where 1 indicated ‘extremely disagree’ or ‘not at all satisfied’ and 10 indicated ‘extremely agree’ or ‘very satisfied’. The proportion of psychiatrists who rated their response as ≥8 was summed to reflect their level of agreement with each statement or satisfaction with each medication.
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki, and all participants gave written informed consents.
Statistical Analysis
For continuous data, the normality of the distribution in each group was examined. If the normality was held, F-test of equal variances was applied to determine either processing pooled or Satterthwaite t test for comparing mean differences between groups. Mann-Whitney test was used to compare continuous variables that were not normally distributed. For categorical variables, the statistical difference between groups was identified using Chi-square test. When >20% of the cells had an expected count of <5, exact test was employed, and unconditional exact test using Z-pooled statistic was chosen for binary data. All tests were 2-sided and the alpha level was set to 0.05 for statistical significance. To identify and classify psychiatrists on the basis of their similar characteristics, cluster analysis was used to minimise within-group variance and maximise between- group variance. A hierarchical clustering approach was first adopted to determine the optimal number of clusters. Once the number of clusters was identified, a k-means clustering algorithm was applied to classify psychiatrists into different clusters.
Results
Psychiatrists’ General Attitude to Antipsychotics
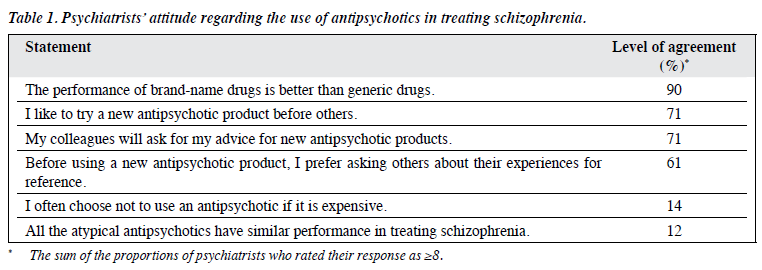
Of 161 attending psychiatrists invited, 69 (43%) consented to be interviewed. The participating psychiatrists agreed that the performance of brand-name drugs was better than generic drugs (level of agreement, 90%) and were likely to try new antipsychotic medications before others (71%). The colleagues of the majority of the psychiatrists were likely to ask for advice about new agents for schizophrenia (71%) [Table 1].
Psychiatrists’ Satisfaction with Second-generation Antipsychotics
In the treatment of schizophrenia, SGAs like paliperidone, olanzapine, and risperidone scored the highest for level of satisfaction among psychiatrists with mean scores (out of 10) of 7.8, 7.7, and 7.6, respectively. The FGAs were the last to be considered for the treatment of schizophrenia (data not shown). The reasons of using the above SGAs included better symptom control and tolerability. Taking paliperidone as an example, for more than 40% of the psychiatrists, reasons for prescribing it included improvement in positive and negative symptoms as well as cognition, reduction in side-effects, and good tolerability; almost half prescribed paliperidone because of its good tolerability.
Psychiatrists’ Characteristics and Use of Second- generation Antipsychotics
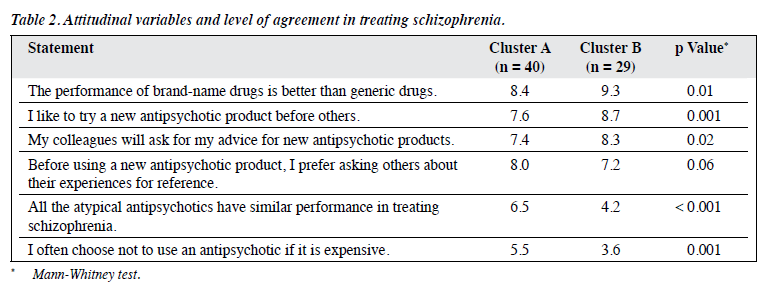
According to responses to the 6 pre-specified questions listed in Table 1, respondents could be classified into 2 clusters (Table 2). Psychiatrists in cluster A were more likely not to prescribe an antipsychotic if it is expensive, and more likely to believe that all SGAs perform similarly. On the other hand, psychiatrists in cluster B preferred brand-name drugs over generic drugs; they were more willing to use new antipsychotics, and were more likely to disagree with the statement “All the atypical antipsychotics have similar performance in treating schizophrenia”. The demographic characteristics of the psychiatrists in the 2 clusters were statistically similar, including age, gender, hospital type, and region of practice.
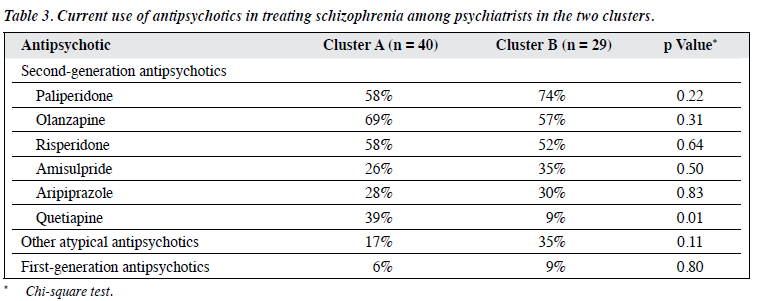
As shown in Table 3, psychiatrists of both clusters were similar in that they were likely to prescribe paliperidone, olanzapine, and risperidone in the treatment of schizophrenia, consistent with their level of satisfaction with these agents. Overall, the use of quetiapine was low, and was rarest among psychiatrists in cluster B which was comparable with the use of FGAs. Although not statistically significant, the use of paliperidone was more frequent among psychiatrists in cluster B than those in cluster A; and use of olanzapine and risperidone was more frequent among psychiatrists in cluster A. Overall satisfaction with paliperidone was significantly higher among psychiatrists in cluster B than that in cluster A (74% vs. 47%; p < 0.05) [data not shown]. In terms of specific measures of its efficacy and safety, there was no difference among psychiatrists of the 2 clusters in their level of satisfaction.
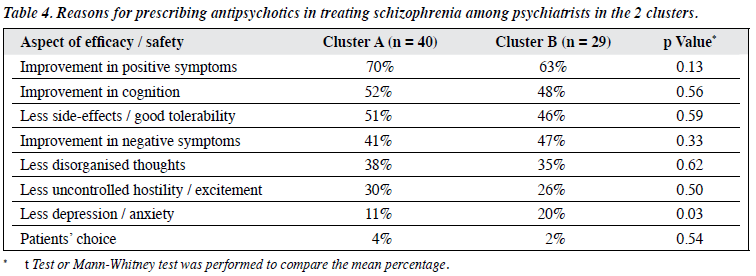
Reasons for prescribing antipsychotics were similar among psychiatrists in both clusters, and mainly included their efficacy in improving positive and negative symptoms, cognition, and their safety / tolerability. There were more psychiatrists in cluster B than in cluster A cited ‘less depression / anxiety’ as the reason for prescribing antipsychotics (20% vs. 11%; p = 0.03) [Table 4].
Discussion
Results of this survey suggest that in the treatment of patients with schizophrenia, paliperidone, olanzapine, and risperidone are the preferred SGAs of psychiatrists. The reasons for antipsychotic prescriptions appeared to be safety and efficacy in improving positive and negative symptoms as well as cognition, reduction in side-effects, and good tolerability. It appears that psychiatrists in Taiwan who determine a treatment strategy are likely to find an optimal balance between efficacy and side-effects, and SGAs do have some advantages. Roh et al11 reported similar findings that the most common prescribed antipsychotics in the treatment of first-episode schizophrenia were (in descending order of prescription frequency) risperidone, quetiapine, paliperidone, and olanzapine, in their patient group in 2010.
In our survey, however, we observed that the use of quetiapine was low overall; it was the rarest prescribed SGA among psychiatrists in cluster B which was comparable with the use of FGAs. Whether this is because of factors such as cost, efficacy, and safety concerns warrants further investigation. In our survey, paliperidone was a commonly prescribed antipsychotic agent in the treatment of schizophrenia, especially among psychiatrists in cluster B. On the other hand, FGAs were least prescribed. Of note, most SGAs currently in use in Taiwan have been replaced by generic drugs since their patents have expired. Among the SGAs included in our study, paliperidone is the only one still on patent. As such, it has a higher level of exposure among psychiatrists in terms of commercial promotional activities. This may result in a higher likelihood of prescription. Another explanation for the more frequent use of newer SGAs might be their better overall efficacy and tolerability. Our results showed that psychiatrists preferred using such agents primarily for their safety and efficacy in improving positive and negative symptoms as well as cognition, reducing side- effects, and good tolerability. It has been reported that while FGAs were mainly used to control aggressive behaviour and positive symptoms, SGAs were targeted at the alleviation of positive and negative psychotic symptoms as well as global cognition in schizophrenia.2,12 In Taiwan, SGAs, especially paliperidone, are officially recommended only to those who are non-responsive to FGAs, older patients, or in the event of prominent adverse effects. These restrictions have been reduced recently because of research and guidelines that confirm the effectiveness of SGAs as first-line treatment for schizophrenia. This might partly explain the frequent use of newer SGAs such as paliperidone, and very low use of FGAs by psychiatrists in both clusters in our study.
Generic drugs are marketed as therapeutically equivalent and less expensive than brand-name ones. Although generic drugs do not undergo the rigorous approval process required of the original drug, their effectiveness and safety are presumed to be equal. In this study, most psychiatrists who preferred brand-name drugs believed that their performance was superior to that of generic drugs, and were more willing to use new antipsychotics. This applied particularly to psychiatrists in cluster B. Similar to our findings in psychiatrists in both clusters, Hamann et al13 reported that psychiatrists were relatively reluctant to use generic drugs. Potential variables that could significantly influence psychiatrist’s choice of a brand-name drug rather than a generic one included imagining choosing the drug for themselves (vs. recommending a drug to a patient), lower share of outpatients, more negative attitudes towards generic drugs, and lower uncertainty for tolerance. Uncertainty about tolerance has previously been shown to be a predictor of prescription behaviour. Psychiatrists who are less certain about tolerance appear to be keen to prescribe brand- name drugs. These uncertainties relate to differences in bioequivalence, negative consequences for patient stability, and interference with patient medication compliance.13-15 Hamann et al13 also showed that a psychiatrist’s decision to select a brand-name or generic drug is largely influenced by ‘non–evidence-based’ factors, and vague attitudes towards properties of generic and brand-name drugs. They reported the ‘non–evidence-based’ belief that brand-name drugs are perceived as somehow ‘better’ than generic drugs with no clear focus on any special advantages (apart from placebo effects that are seen as stronger for brand-name drugs). Nonetheless, several studies and case reports describe clinical deterioration, decreased efficacy / tolerability, and reduced compliance with generic substitutions.14-16 This is due to the recognised need to tailor pharmacological treatment to the individual patient in order to maximise outcome. Psychiatrists might be more anxious about the potential drawbacks of generic drugs (that are less well known to them) and therefore hesitate to prescribe them. We speculated that such factors might have an effect on the prescription behaviour of the psychiatrists in our study, especially those in cluster B.
Prescribing behaviour may be influenced by financial factors and cost containment strategies.17 Chong et al12 also highlighted that utilisation of SGAs in East Asia is influenced by the healthcare system and the availability and cost of the drugs, although the prescription patterns varied among different countries. We speculated that the health insurance policy of the TBNHI might affect psychiatrists’ selection and clinical decision making regarding SGA prescription. In fact, to contain medical expenditure, cost regulation programmes have been implemented in hospitals by the TBNHI, with consequent changes in physicians’ medical behaviour such as reduced prescription of drugs, limited daily service hours in clinics, and reduced drug expenditure.18 In order to control pharmaceutical expenditure, psychiatrists are persuaded to prescribe cheaper drugs, and are more likely to prescribe older, generic antipsychotics instead of newer, brand-name agents. Chiu et al18 concluded that the use of SGAs was believed to have been reduced by TBNHI’s implementation of the global budget programme. Our study had similar findings that psychiatrists in Taiwan often choose not to prescribe certain SGAs because of their higher cost, especially psychiatrists in cluster A. Nonetheless, psychiatrists in cluster B were more likely to prescribe more expensive brand-name SGAs such as paliperidone and olanzapine to treat their patients instead of cheaper SGAs or FGAs. This finding is similar to a report that an intervention programme to encourage use of older, generic antipsychotics instead of newer, on-patent SGAs did not decrease the rate of prescription of the latter.19 Several reports also acknowledge that generic substitution in schizophrenia may not be cost-saving due to compliance loss, decreased symptom control, and lower quality of life or possible relapse, thus reducing the impetus to proceed with compulsory generic switching.14-16 The demand-side properties of certain diseases such as schizophrenia, and the recognised need to maximise outcome imply that it is difficult to restrict prescriptions of brand-name drugs or encourage the preferential prescribing of multiple- sourced generic drugs as first-line treatment.17 Prescription of antipsychotics is a complex clinical decision based on price, efficacy and side-effects, as well as characteristics and attitudes of psychiatrists.4,6
This is the first report about psychiatrists’ attitude and use of SGAs in the treatment of schizophrenia in Taiwan. The results of this survey must be considered in light of its limitations. First, the survey is of a limited scale with only 69 respondents participating. Second, questions covered in this survey were arbitrarily designed and might not completely reflect the actual opinion of participants. Lastly, the nature of the recruitment process inevitably created a certain degree of selection bias, as only psychiatrists being contacted and were willing to take part in the survey were included. A randomly selected sample would have been more appropriate.
In conclusion, the results of this survey suggest that psychiatrists in Taiwan are more satisfied with certain SGAs in the treatment of patients with schizophrenia. Although drug selection is not influenced by gender, age, or practice setting of the psychiatrists, it is potentially influenced by the psychiatrist’s characteristics, properties of the drugs, and the healthcare insurance system. Better symptom control, improvement in cognition, and higher tolerability appear to be among the major factors considered by psychiatrists in Taiwan when prescribing antipsychotics.
Acknowledgements
We would like to thank Dr Chau-Shoun Lee (MacKay Medical College and MacKay Memorial Hospital) for providing additional scientific review of the manuscript.
Declaration
All authors have disclosed no conflicts of interest.
References
- Chaudhury PK, Deka K, Chetia D. Disability associated with mental disorders. Indian J Psychiatry 2006;48:95-101.
- Zhang JP, Gallego JA, Robinson DG, Malhotra AK, Kane JM, Correll CU. Efficacy and safety of individual second-generation vs first- generation antipsychotics in first-episode psychosis: a systematic review and meta-analysis. Int J Neuropsychopharmacol 2013;16:1205-18.
- Thibaut F. Acute treatment of schizophrenia: introduction to the World Federation of Societies of Biological Psychiatry Guidelines. Psychiatr Danub 2014;26:2-11.
- Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 2009;373:31-41.
- Vlastlica M. Psychodynamic approach as a creative factor in psychopharmacotherapy. Psychiatr Danub 2013;25:316-9.
- Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry 2004;161(2 Suppl):1- 56.
- Thakkar KB, Jain MM, Billa G, Joshi A, Khobragade AA. A drug utilization study of psychotropic drugs prescribed in the psychiatry outpatient department of a tertiary care hospital. J Clin Diagn Res 2013;7:2759-64.
- Nielsen J, Dahm M, Lublin H, Taylor D. Psychiatrists’ attitude towards and knowledge of clozapine treatment. J Psychopharmacol 2010;24:965-71.
- Barbui C, Biancosino B, Esposito E, Marmai L, Donà S, Grassi L. Factors associated with antipsychotic dosing in psychiatric inpatients: a prospective study. Int Clin Psychopharmacol 2007;22:221-5.
- National Health Insurance in Taiwan: 2013-2014 Annual Report. Taipei, Taiwan, Bureau of National Health Insurance, Department of Health, Executive Yuan; 2013.
- Roh D, Chang JG, Yoon S, Kim CH. Antipsychotic prescribing patterns in first-episode schizophrenia: a five-year comparison. Clin Psychopharmacol Neurosci 2015;13:275-82.
- Chong MY, Tan CH, Fujii S, Yang SY, Ungvari GS, Si T, et al. Antipsychotic drug prescription for schizophrenia in East Asia: rationale for change. Psychiatry Clin Neurosci 2004;58:61-7.
- Hamann J, Mendel R, Kissling W, Leucht S. Psychiatrists’ decision making between branded and generic drugs. Eur Neuropsychopharmacol 2013;23:686-90.
- Margolese HC, Wolf Y, Desmarais JE, Beauclair L. Loss of response after switching from brand name to generic formulations: three cases and a discussion of key clinical considerations when switching. Int Clin Psychopharmacol 2010;25:180-2.
- Treur M, Heeg B, Möller HJ, Schmeding A, van Hout B. A pharmaco- economic analysis of patients with schizophrenia switching to generic risperidone involving a possible compliance loss. BMC Health Serv Res 2009;9:32.
- Desmarais JE, Beauclair L, Margolese HC. Switching from brand- name to generic psychotropic medications: a literature review. CNS Neurosci Ther 2011;17:750-60.
- Godman B, Petzold M, Bennett K, Bennie M, Bucsics A, Finlayson AE, et al. Can authorities appreciably enhance the prescribing of oral generic risperidone to conserve resources? Findings from across Europe and their implications. BMC Med 2014;12:98.
- Chiu HJ, Chou PH, Loh el-W, Lan TY, Wu BJ, Chang YY, et al. Changes in the prescription pattern of antipsychotics for schizophrenic outpatients after the implementation of a global budgeting program. J Chin Med Assoc 2014;77:325-32.
- Hermes ED, Sernyak M, Rosenheck R. Impact of a program encouraging the use of generic antipsychotics. Am J Manag Care 2012;18:e307-14.