East Asian Arch Psychiatry 2012;22:146-53
ORIGINAL ARTICLE
首发抑鬱症患者其功能性躯体化病徵的现患率和类型
Dr Sandeep Grover, MD, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Dr Vineet Kumar, MD, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Prof. Subho Chakrabarti, MD, FRCPsych, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India. Dr Prabhakar Hollikatti, MD, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Mr Pritpal Singh, MPhil, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Mr Shikha Tyagi, MPhil, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Prof. Parmanand Kulhara, MD, FRCPsych, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India. Prof. Ajit Avasthi, MD, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Address for correspondence: Dr Sandeep Grover, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh 160012, India.
Tel: (91-172) 2756807; Fax: (91-172) 2744401 / 2745078; email: drsandeepg2002@yahoo.com
Submitted: 28 December 2011; Accepted: 22 February 2012
Abstract
Objective: To study the prevalence and type of functional somatic complaints in patients with first- episode depression.
Methods: A total of 164 patients attending the outpatient department of a general hospital psychiatric unit were evaluated using the Patient Health Questionnaire–15 (PHQ-15) and Hamilton Depression Rating Scale (HDRS).
Results: More than half of the sample were male (n = 85; 52%) and most of the subjects were married (n = 128; 78%). The mean (standard deviation) HDRS score was 19.9 (5.4). All patients had at least 1 functional somatic complaint, and that the mean (range) number of functional somatic complaints per patient on the PHQ-15 was 8 (1-15). The most common functional somatic complaints included feeling tired or having little energy (93%); trouble sleeping (80%); nausea, gas and indigestion (68%); headache (68%); pain in arms, legs, or joints (66%); and feeling the heart racing (65%). Total PHQ-15 scores indicated the presence of moderate-to-severe severity of functional somatic complaints. Back pain, as well as pain in arms, legs, or joints, were found to be more common in females. The number and severity of functional somatic complaints did not differ significantly in relation to other socio-demographics (locality, marital status, age, education, income) and clinical variables (duration, physical co-morbidity, and atypical features).
Conclusion: Functional somatic complaints are quite prevalent in subjects with first-episode depression. Hence, clinicians should routinely evaluate patients with depression for these symptoms.
Key words: Depression; Somatoform disorders
摘要
目的:检视首发抑鬱症患者其功能性躯体化病徵的现患率和类型。
方法:应用患者健康问卷(PHQ-15)和汉氏忧鬱量表(HDRS),对印度一所综合医院精神科门诊部的164名患者进行评估。
结果:在这些患者中,超过一半为男性(n = 85;52%)且大部份已婚(n = 128;78%)。HDRS平均比分为19.9(标準差5.4)。根据PHQ-15的评估,每名患者出现至少1种(介乎1至15种)功能性躯体化病徵,中位数为8种。最常见的功能性躯体化病徵包括感觉疲倦乏力(93%)、失眠(80%)、噁心有胃气和消化不良(68%)、头痛(68%)、胳膊、腿或关 节疼痛(66%),以及心跳加速(65%)。PHQ-15总比分显示中度至严重的功能性躯体化病 徵。背部疼痛,以及胳膊、腿或关节疼痛在女性患者中较常见。功能性躯体化病徵的数目和 严重程度跟社会人口统计学数据(居住环境、婚姻状况、年龄、教育程度和收入)和临床变数(病程、共病和非典型病徵)没有显著相关性。
结论:首发抑鬱症患者其功能性躯体化病徵的现患率颇为普遍。因此,临床医生应对抑鬱症患者的这些病徵作常规评估。
关键词:抑鬱症、心身症
Introduction
Depressive disorder is currently understood the world over by the diagnostic criteria as proposed by the ICD-10 (Mental and Behavioural Disorders)1 and DSM-IV-TR.2 A study from India3 reported that a significant proportion of patients with depression have other physical complaints, which do not find a place in these diagnostic systems. These complaints often dominate the clinical picture and exert a crucial influence on the perception of the illness to an extent that many patients believe their illness to be of physical origin. This belief leads to multiple consultations with medical services resulting in misutilisation of resources,4 wrong diagnoses, and inordinate delay before initiation of appropriate treatment. These physical complaints have been described by various terms like physical, bodily, functional or somatic complaints and somatisation. Some have attempted to operationalise such manifestations as medically unexplained somatic complaints, hypochondriacal worry, or somatic preoccupation.5 As these somatic complaints are presumed to be a part of the depressive syndrome without any underlying physical cause, possibly a more appropriate term to describe them could be functional somatic complaint (FSC).3 Earlier it was thought that FSC is more common in non-western populations, particularly among Asians because of the cultural disapproval for expressing strong negative emotions.6 Some authors even considered FSC an alternative ‘idiom of distress’, prevalent in cultures where psychiatric disorders carry greater stigma.7 However, a cross-cultural study8 conducted by the World Health Organization (WHO) suggested that worldwide FSC is the most common clinical expression of emotional distress. It also showed that their frequency did not clearly vary according to geography or level of economic development.8 Studies also suggested that FSC in depression is more frequently noted in women, elderly, children, and those having relatively low incomes.9-12
Studies on patients with depression in primary care settings suggested that FSC occurs more as a rule than an exception,13-17 and consistently showed that two- thirds or more of the depressed patients in primary health care have such complaints.14-17 Clinic-based studies also suggested a high prevalence (73-92%) of FSC in patients with depression.18-22 Hamilton18 reported FSC in 80% of the sample of 260 women and 239 men suffering from major depression, and Sugahara et al19 reported a prevalence of 77% in depressed outpatients attending the psychosomatic medicine department in a hospital of Japan. In a multicentric study from Latin America, Muñoz et al20 evaluated 989 depressed patients and reported painful FSC in 73% of those attending the psychiatric outpatient clinic; they also showed that higher severity of painful somatic symptoms was associated with increased severity of depression and poor quality of life. In a study of assessing 150 depressed patients using a self-reported 90-item Symptom Checklist, 92% reported FSC.21
In general, studies from India focused on non-organic somatic complaints in psychiatric outpatient populations, and suggested that about 30% of patients seeking a psychiatric consultation present with FSC.23 Many of these patients have a diagnosis of depression.23-26 However, none of the studies specifically studied patients with depression for the prevalence of FSC. Against this background, the present study aimed to evaluate the prevalence and typology of FSC in patients diagnosed with depression. Additionally, it attempted to study FSC in relation to socio-demographic and clinical correlates.
Methods
Setting
The study was carried out in a tertiary care multispecialty teaching hospital in North India. All study patients were recruited with their written informed consent and were seen during the period of 1 March to 30 June 2010. The study was approved by the research review committee of the department. The present report is part of a larger study which evaluated the pathways to care, attitude towards psychotropic medications, prevalence and typology of FSC, aetiological attribution of depressive symptoms by patients, and treatment compliance. In this paper, data with respect to FSC are presented.
Sample
The sample comprised 164 consecutive patients attending the walk-in clinic of psychiatry outpatient department. To be included in the study, the patients had to be diagnosed with first-episode depression (but excluding severe depression with psychotic symptoms) as per the ICD-10 criteria1 and aged ≥ 18 years. Patients with co-morbid psychiatric disorder or any substance (except nicotine) dependence were excluded.
Instruments
17-Item Hamilton Depression Rating Scale
The 17-item Hamilton Depression Rating Scale (HDRS)27 was used to assess the severity of depression. Items were rated from 0 to 4 or from 0 to 2 according to intensity and frequency of symptoms over the past week. With a total score ranging from 0 to 52, scores of 0-7 indicated no depression; 8-13 mild depression; 14-18 moderate depression; 19-22 severe depression; and ≥ 23 very severe depression. This rating scale is a valid instrument with an intra-class correlation coefficient of 0.86 indicating adequate inter-observer agreement.27
Patient Health Questionnaire–15
The Patient Health Questionnaire–15 (PHQ-15)28,29 was used to assess the prevalence and typology of FSC. It is a self-administered version of the Primary Care Evaluation of Mental Disorders Patient Health Questionnaire (PRIME- MD PHQ), a diagnostic instrument for common mental disorders. The 15 somatic symptoms or symptom clusters included in PHQ-15 accounted for more than 90% of the physical complaints (excluding upper respiratory tract symptoms) reported in the outpatient setting.30,31 Of these PHQ-15 somatic symptoms, 13 were included in the PHQ somatic symptom module, in which patients rated the severity of each symptom as 0 (not bothered at all), 1 (bothered a little), or 2 (bothered a lot). Two additional physical symptoms (‘feeling tired or having little energy’ and ‘trouble sleeping’) were contained in the PHQ depression module. The subjects were asked: “Over the last 2 weeks, how often have you been bothered by any of the following problems?” Response options were coded as 0 (not at all), 1 (several days), or 2 (more than half the days / nearly every day). Thus, the PHQ-15 total score indicated a severity ranging from 0 to 30. Based on the total score, the severity of FSC was graded as mild (0-4), moderate (5-9), and severe (≥ 10).32 The full version of PRIME-MD PHQ was translated into Hindi using WHO methodology and has been shown to have good psychometric properties.33 For the present study, the Hindi version was used and patients themselves rated their symptoms. In case the patients were not able to read Hindi, the scale was administered by the psychiatrist assessing the patient.
Clinical Profile Sheet
A study-specific clinical profile sheet was designed for recording patients’ medication status (drug-naïve or not), alcohol and other drug dependence history (as per ICD- 10), sexual dysfunction prior to onset of depression, presence and type of sexual dysfunction due to depression, presence and type of atypical features of depression (weight gain, increased appetite, leaden paralysis, hypersomnia or interpersonal rejection sensitivity), as well as type of physical morbidity and treatment prescribed.
Procedure
All patients diagnosed with first-episode depression (as per ICD-10) were approached and explained the purpose of the study. Patients who fulfilled inclusion criteria were evaluated further. Socio-demographic data were recorded by psychiatric social workers. Recording of clinical data and rating on HDRS was performed by the psychiatrist evaluating the patient. Thereafter, the patients were requested to complete the Hindi version of the PHQ-15.
Statistical Analysis
Data were analysed using the Statistical Package for the Social Sciences, Windows version 14. Means and standard deviations (SDs) were calculated for continuous variables, and frequencies and percentages were calculated for discrete variables. Comparisons entailed using the Chi-square and Mann-Whitney tests. Correlations between socio- demographics, clinical variables, HDRS, and PHQ-15 were examined using the Spearman rank correlation analysis.
Results
During the study period of 4 months, a total of 426 patients were diagnosed to have first-episode depression by a qualified psychiatrist. Of these, 187 patients were excluded because of Axis 1 psychiatric co-morbidity, 13 others were diagnosed to have severe depression with psychotic symptoms, 40 refused to participate in the study, and in 22 the data available were incomplete. Thus, the final sample entailed 164 patients.
Socio-demographic Profile
The mean (SD) age of the study sample was 41 (15) years. In terms of different age-groups, 91% (n = 149) were aged 18 to 64 years, the rest were ≥ 65 years. Their mean (SD) duration of education was 10 (5) years. The majority of the patients were married and inhabitants of neighbouring states. About half of the sample (52%; n = 85) were not in a paid employment. The mean (SD) monthly income of the study sample was 6148 (12,418) Indian Rupees (Table 1).
Clinical Profile
About one-fourth of these 164 patients had a co-morbid physical illness, hypertension being the most common (n = 27; 17%). Although abstinent at the time of the study, there was a history of alcohol or other drug dependence in a few patients (n = 10; 6%) [Table 1]. The mean (SD) duration of depression was 13 (22) months, being ≤ 6 months in 58% (n = 94), between 6 and 12 months in 21% (n = 35), and > 12 months in the remainder. Notably, 112 had never been treated with any antidepressant, while the remaining 52 had been prescribed an antidepressant by a physician or a psychiatrist. At the index assessment, prescription data were available for 124 (76%) of the patients. Escitalopram was the most commonly prescribed antidepressant (n = 62; 38%) followed by venlafaxine (n = 25; 15%).
Phenomenology of Depression
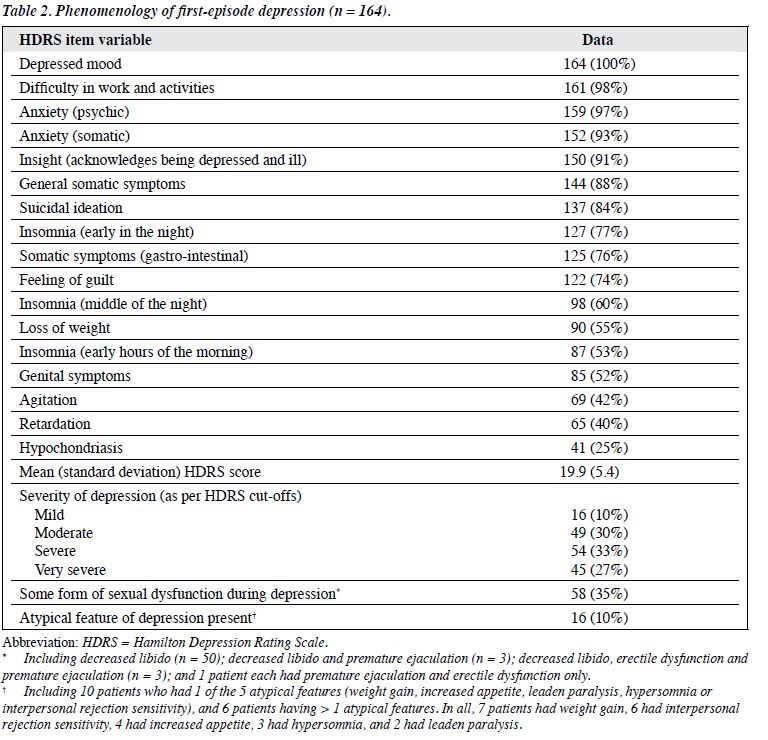
The frequency of other symptoms was shown in Table 2. The mean HDRS score of the study sample was 19.9. The most common symptom was depressed mood (100%) followed by difficulty in work and activities (98%), psychic anxiety (97%), and somatic anxiety (93%). About one-third of the patients (n = 58) had sexual dysfunction that started during the course of the illness. About 10% of the patients had atypical features of depression.
Prevalence and Typology of Functional Somatic Symptoms
All patients reported at least 1 FSC as assessed on PHQ-15. Of these, 96% (n = 158) reported at least 3 FSCs, in whom over 75% (n = 128) had 6 to 15 FSCs. The mean (SD)
number of somatic symptoms per patient was 8 (3) and the median for the same was 8. The mean ± SD total PHQ-15 score was 11 ± 5 (range, 1-25; median = 25). In terms of severity of FSC, 12 (7%) patients had a total PHQ-15 score of 1 to 4, 60 (37%) had scores of 5 to 9, and the remainder had scores of ≥ 10.
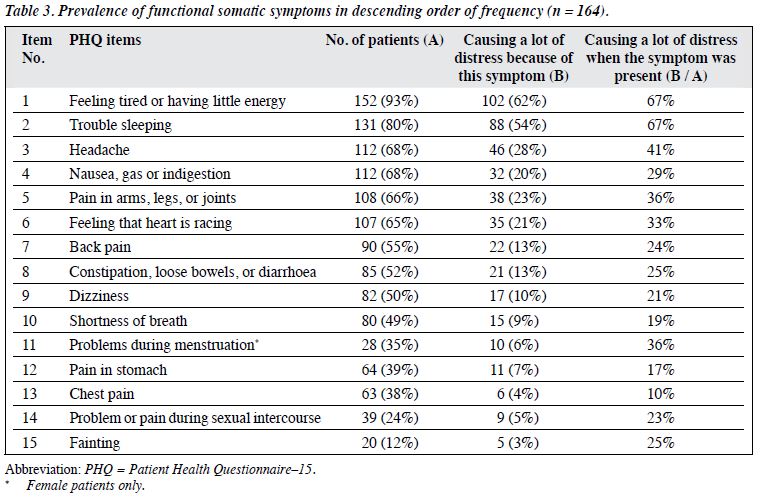
Table 3 shows the prevalence of various FSCs as assessed on the PHQ-15. The most common symptoms (present in two-thirds or more of the patients) included feeling tired or having little energy; trouble sleeping; headache; nausea, gas or indigestion; pain in the arms, legs, or joints; and feeling that heart was racing. Of these, the first 2 led to maximum distress, and that 67% rated them as ‘leading to a lot of distress’.
Relationship of Prevalence of Functional Somatic Complaints with Different Variables
Regarding socio-demographic variables, our study revealed that back pain (χ2 = 5.7; p = 0.02) and pain in the arms, legs, or joints (χ2 = 3.9; p = 0.05) were FSCs that were significantly more prevalent in females. No significant difference in the prevalence of any FSC in patients from urban versus rural background was found. Headache was significantly more prevalent in migrant patients (χ2 = 6.5; p = 0.01). Marital status and religion had no influence on the prevalence of FSC. Similarly, there was no difference in the prevalence of FSC between the patients aged < 65 years and those ≥ 65 years.
Concerning clinical variables, there was no difference in the prevalence of FSC between patients who were drug- naïve or those receiving antidepressant treatment in the past. Patients without any physical co-morbidity had fainting spells more frequently (χ2 = 5.8; p = 0.02). Compared with those with any of the atypical features of depression, those without had significantly higher prevalence of feeling tired or having little energy (χ2 = 5.1; p = 0.02) and trouble sleeping (χ2 = 9.3; p = 0.002).
In terms of the total number and severity of FSCs, females had more FSCs (Mann-Whitney value, 2604; p = 0.02) and higher mean scores (Mann-Whitney value, 2404; p = 0.002). There was no correlation between total number of FSCs or the total PHQ-15 score and patient age, education level, or income. Also, other socio-demographic variables did not appear to influence the total number of FSCs or the total PHQ-15 score.
The total number of FSCs and total PHQ-15 scores yielded no significant association with the presence of physical co-morbidity, atypical features of depression, and medication status (drug-naïve or not). There was also no correlation between the total number of FSCs or the total PHQ-15 score and the duration of illness.
The total HDRS scores yielded a significant positive correlation with the total number of FSCs (Spearman rank correlation coefficient, 0.245; p = 0.002) and total mean PHQ-15 scores (Spearman rank correlation coefficient 0.199; p = 0.01), but this correlation could be spurious as some items were similar in both scales. Further correlation analysis was therefore attempted after removing the somatic items from the HDRS total score. When the somatic symptoms (items 4-6), somatic anxiety (item 11), gastro-intestinal somatic symptoms (item 12), general somatic symptoms (item 13), and genital symptoms (item 14) were removed from the total HDRS score, the correlation between total HDRS scores and total number of FSCs and the total mean PHQ-15 scores was no longer evident. Furthermore, the total number of FSCs and the total mean PHQ-15 scores had no relationship with suicidal behaviour (as assessed by suicidal ideation item of the HDRS).
Discussion
This study attempted to determine the prevalence of FSC in patients with first-episode depression and to study its relationship with various socio-demographic and clinical variables. The study recruited consecutive eligible adult patients (≥ 18 years) attending the outpatient clinic of a tertiary care hospital. An attempt was made to assess other symptoms of depression using standard rating scale like HDRS.
Patient Health Questionnaire–15, an instrument proved to account for more than 90% of FSCs in primary care patients, was used to assess the FSCs in the present study. Our study showed that FSCs were found to be highly prevalent in depressed patients attending the psychiatry outpatient of a tertiary care hospital. All patients had at least 1 FSC, with a mean of 8 (range, 1-15) for each patient. Studies from different parts of the world assessed the prevalence of FSC using various instruments like the Bradford Somatic Inventory (BSI),34 the Somatic Symptom Inventory,35 the Depression and Somatic Symptoms Scale,36 the Symptom Checklist-90-R,37 the PRIME-MD,29 and the Center for Epidemiologic Studies Depression scale.37 These studies reported prevalence rates of ≥ 1 FSC(s) in 66 to 93% patients attending primary care settings,14-17 and 72 to 100% in patients attending psychiatric centres.18-22 Although these studies differed in methodology in terms of the type of study population and assessment instrument, they all suggested that FSCs are highly prevalent in patients with depression.
In the present study, the mean number of FSC per patient was 8. A study from India, although not restricted to depressed patients, reported 4 FSCs per patient.26
Another study using BSI for assessment reported 21 FSCs per depressed patient.38 When comparing the findings of the present study with these studies, the prevalence in our study was within the previously reported range. Reported differences between studies can be appreciated on account of different assessment instruments used (e.g. BSI has 50 items to assess FSCs).In the present study, majority of the patients (93%) had a total PHQ-15 score of ≥ 5, indicating moderate- to-severe intensity FSCs. Literature on this aspect from elsewhere is not available for comparison. The most prevalent FSCs were feeling tired or having little energy (93%), trouble sleeping (80%), headache (68%), nausea, gas or indigestion (68%), pain in arms, legs, or joints (66%) and feeling that heart is racing (65%). Existing literature suggested that painful symptoms and ‘feeling fatigued, weak, or tired all over’ were more commonly reported.19,20,39 Studies in primary care patients also suggested a significant association between major depression and painful FSCs, such as joint pains, lumbar pain, and headache.40-42 Other studies from India, which evaluated patients presenting with FSCs, also reported headache to be the most common FSC (present in 81-84% of cases).23,25,26 Other commonly reported somatic complaints in previous studies from India included aches and pains (91%) involving limbs and joints followed by headache; autonomic symptoms (72%) like palpitations, giddiness, numbness; weakness and tiredness (66%); and behavioural symptoms (66%) such as lack of sleep and appetite.43 In a previous study from our centre,38 ‘feeling of lack of energy (weakness) much of the time’ (98%) was the most common FSC, followed by feeling tired when not working (82%), heavy head feeling (74%), feeling of constriction of head (68%), and aches and pains all over the body (64%). These data suggested that painful FSCs are quite common in patients with depression.
Researchers have attempted to study socio- demographic and clinical correlates of FSCs in patients with depression. Studies from the West suggested that FSCs are more common in females.44-46 In the present study, among all FSCs, back pain, as well as pain in arms, legs, or joints were more common in females, but as consistent with a previous study,38 their number and severity did not differ significantly in relation to other variables like locality, marital status, age, education level, and income. It was also noted that the duration of illness, physical co-morbidity, and the presence or absence of atypical features were not significantly associated with the prevalence of FSC. These findings suggested that as such socio-demographic and clinical variables have no impact on the prevalence of FSC in depression, and possibly therefore FSCs are part and parcel of depression. Moreover, our study revealed that significant correlations between the number and severity of FSCs and total HDRS scores disappeared when items dealing with somatic symptoms were removed from the HDRS score. In the existing literature, there is no consensus regarding the relationship between severity of depression and FSC. A few psychiatric outpatient-12,20,39,47,48 and inpatient-based23 studies reported significant positive correlation between FSC and severity of depression. Several others14,34,49,50 conducted in different settings also found that the prevalence of FSC did not correlate with the severity of depression. The present study also suggests that some of the correlations reported in the literature may be spurious due to the use of instruments like HDRS which also includes some of the FSCs.
Regarding the current nosological systems (DSM-IV and ICD-10), though they include FSC like ‘feeling tired or having little energy’ and ‘trouble sleeping’ as part of the diagnostic criteria for depression, many FSCs, in particular painful symptoms like headache and pain in arms, legs or joints, are not included. Similarly, current diagnostic systems do not give any importance to gastro-intestinal symptoms (nausea, gas or indigestion, constipation, loose bowels or diarrhoea) or the autonomic symptoms. Owing to the high prevalence of these symptoms in patients with depression, any revision of nosology should include these FSCs as part of the diagnostic criteria of depression. Our study also suggests that these symptoms should be routinely evaluated when assessing patients with depression. Future clinical trials should also take these complaints into account while evaluating the efficacy of various antidepressants.
One limitation of this study was one-time assessment of patients for the FSCs. Also, we did not assess other clinical variables like the level of anxiety, hypochondriasis, somatosensory amplification, and alexithymia (difficulty describing emotions) associated with FSC. Furthermore, the study was limited to a clinic population only, hence the findings could not be generalised to primary care settings. Nor did we study the influence of FSC on the treatment adherence and drug compliance, help-seeking behaviour, and the effectiveness of various treatment measures. Future studies should attempt to overcome these limitations by evaluating a larger sample comprising patients from different treatment settings. Research in this area should also focus on developing effective interventions for FSC in patients with depression.
To conclude, the present study suggests that FSCs are highly prevalent in patients diagnosed with depression. Most patients had more than 3 FSCs. The prevalence and typology of FSCs were not much influenced by socio-demographic or clinical variables and severity of depression. Considering the high prevalence of FSCs in depression, there is a need to include these symptoms in diagnostic guidelines and nomenclature.
References
- The ICD-10 Classification of Mental and Behavioural Disorders— Clinical Descriptions and Diagnostic Guidelines. Geneva, World Health Organization; 1992.
- Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision (DSM-IVTR). Washington, DC, American Psychiatric Association; 2000.
- Chakraborty K, Avasthi A, Grover S, Kumar S. Functional somatic complaints in depression: an overview. Asian J Psychiatr 2010;3:99-107.
- Lloyd G. Medicine without signs. Br Med J (Clin Res Ed) 1983;287:539-42.
- Lipowski ZJ. Somatization: the experience and communication of psychological distress as somatic symptoms. Psychother Psychosom 1987;47:160-7.
- Conrad MM. Pacquiao DF. Manifestation, attribution, and coping with depression among Asian Indians from the perspectives of health care practitioners. J Transcult Nurs 2005;16:32-40.
- Kleinman A, Good BJ. Culture and depression: studies in the anthropology and cross-cultural psychiatry of affect and disorder. Berkeley: University of California Press; 1985.
- Gureje O, Simon GE, Ustun TB, Goldberg DP. Somatization in cross- cultural perspective: a World Health Organisation study in primary care. Am J Psychiatry 1997;154:989-95.
- Wool CA, Barsky AJ. Do women somatize more than men? Gender differences in somatization. Psychosomatics 1994;35:445-52.
- Kroenke K, Spitzer RL. Gender differences in the reporting of physical and somatoform symptoms. Psychosom Med 1998;60:150-5.
- 1 Stewart DE. Physical symptoms of depression: unmet needs in special populations. J Clin Psychiatry 2003;64 Suppl 7:12-6.
- Sayar K, Kirmayer LJ, Taillefer SS. Predictors of somatic symptoms in depressive disorder. Gen Hosp Psychiatry 2003;25:108-14.
- Robbins JM, Kirmayer LJ. Attributions of common somatic symptoms. Psychol Med 1991;21:1029-45.
- Kirmayer LJ, Robbins JM, Dworkind M, Yaffe MJ. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry 1993;150:734-41.
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med 2003;163:2433-45.
- Caballero L, Aragonès E, García-Campayo J, Rodríguez-Artalejo F, Ayuso-Mateos JL, Polavieja P, et al. Prevalence, characteristics, and attribution of somatic symptoms in Spanish patients with major depressive disorder seeking primary health care. Psychosomatics 2008;49:520-9.
- Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med 1999;341:1329-35.
- Hamilton M. Frequency of symptoms in melancholia (depressive illness). Br J Psychiatry 1989;154:201-6.
- Sugahara H, Akamine M, Kondo T, Fujisawa K, Yoshimasu K, Tokunaga S, et al. Somatic symptoms most often associated with depression in an urban hospital medical setting in Japan. Psychiatry Res 2004;126:151-8.
- Muñoz RA, McBride ME, Brnabic AJ, López CJ, Hetem LA, Secin R, et al. Major depressive disorder in Latin America: the relationship between depression severity, painful somatic symptoms, and quality of life. J Affect Disord 2005;86:93-8.
- Corruble E, Guelfi JD. Pain complaints in depressed inpatients. Psychopathology 2000;33:307-9.
- Tamayo JM, Román K, Fumero JJ, Rivas M. The level of recognition of physical symptoms in patients with a major depression episode in the outpatient psychiatric practice in Puerto Rico: an observational study. BMC Psychiatry 2005;5:28.
- Gautam SK, Kapur RL. Psychiatric patients with somatic complaints. Indian J Psychiatry 1977;19:75-80.
- Chaturvedi SK, Michael A, Sarmukaddam S. Somatizers in psychiatric care. Indian J Psychiatry 1987;29:337-42.
- Banerjee G, Sinha S, Mukerjee DG, Sen G. A study of psychiatric disorders other than psychosis in the referred cases with somatic complaints. Indian J Psychiatry 1987;29:363-6.
- Srinivasan K, Srinivasa Murthy R, Janakiramaiah N. A nosological study of patients presenting with somatic complaints. Acta Psychiatr Scand 1986;73:1-5.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62.
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self- report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999;282:1737-44.
- Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994;272:1749- 56.
- Schappert SM. National Ambulatory Medical Care Survey: 1989 summary. Vital Health Stat 13 1992;(110):1-80.
- Kroenke K, Arrington ME, Mangelsdorff AD. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch Intern Med 1990;150:1685-9.
- Kroenke K, Spitzer RL, William JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 2002;64:258-66.
- Avasthi A, Varma SC, Kulhara P, Nehra R, Grover S, Sharma S. Diagnosis of common mental disorders by using PRIME-MD Patient Health Questionnaire. Indian J Med Res 2008;127:159-64.
- Mumford DB, Devereux TA, Maddy PJ, Johnston JV. Factors leading to the reporting of ‘functional’ somatic symptoms by general practice attenders. Br J Gen Pract 1991;41:454-8.
- Barsky AJ, Wyshak G, Klerman GL. Hypochondriasis. An evaluation of the DSM-III criteria in medical outpatients. Arch Gen Psychiatry 1986;43:493-500.
- Derogatis LR. SCL-90R: Administration, scoring and procedure manual. Baltimore: John Hopkins University Press; 1983.
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385- 401.
- Chakraborty K, Avasthi A, Kumar S, Grover S. Psychological and clinical correlates of functional somatic complaints in depression. Int J Soc Psychiatry 2012;58:87-95.
- Vaccarino AL, Sills TL, Evans KR, Kalali AH. Prevalence and association of somatic symptoms in patients with major depressive disorder. J Affect Disord 2008;110:270-6.
- Mathew NT, Reuveni U, Perez F. Transformed or evolutive migraine. Headache 1987;27:102-6.
- Gerber PD, Barrett JE, Barrett JA, Oxman TE, Manheimer E, Smith R, et al. The relationship of presenting physical complaints to depressive symptoms in primary care patients. J Gen Intern Med 1992;7:170-3.
- Juang KD, Wang SJ, Fuh JL, Lu SR, Su TP. Comorbidity of depressive and anxiety disorders in chronic daily headache and its subtypes. Headache 2000;40:818-23.
- Pereira B, Andrew G, Pedneker S, Pai R, Pelto P, Patel V. The explanatory models of depression in low income countries: listening to women in India. J Affect Disord 2007;102:209-18.
- Lee P, Zhang M, Hong JP, Chua HC, Chen KP, Tang SW, et al. Frequency of painful physical symptoms with major depressive disorder in Asia: relationship with disease severity and quality of life. J Clin Psychiatry 2009;70:83-91.
- Betrus PA, Elmore SK, Hamilton PA. Women and somatization: unrecognized depression. Health Care Women Int 1995;16:287-97.
- Silverstein B. Gender difference in the prevalence of clinical depression: the role played by depression associated with somatic symptoms. Am J Psychiatry 1999;156:480-2.
- Fifer SK, Buesching DP, Henke CJ, Potter LP, Mathias SD, Schonfeld WH, et al. Functional status and somatization as predictors of medical offset in anxious and depressed patients. Value Health 2003;6:40-50.
- García Campayo J. Effectiveness of mirtazapine in the treatment of depression with associated somatic symptoms. Actas Esp Psiquiatr 2008;36:25-32.
- Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res 1985;29:563-9.
- Spinhoven P, van der Does AJ. Somatization and somatosensory amplification in psychiatric outpatients: an explorative study. Compr Psychiatry 1997;38:93-7.