East Asian Arch Psychiatry 2012;22:94-9
THEME PAPER
Early Intervention for First-episode Psychosis in India
印度首发思觉失调早期干预发展
Dr Thara Rangaswamy, MD, PhD, Schizophrenia Research Foundation, India. Dr Ramamurthy Mangala, MD, Schizophrenia Research Foundation, India.
Ms Greeshma Mohan, MA, Schizophrenia Research Foundation, India. Ms Jainey Joseph, MSW, Schizophrenia Research Foundation, India. Mr Sujit John, MSc, Schizophrenia Research Foundation, India.
Address for correspondence: Dr Thara Rangaswamy, Schizophrenia Research Foundation (India), R/7A North Main Road, Anna Nagar (West Extension), Chennai 600101, India.
Tel: (91-44) 2615 1073; email: thara@scarfindia.org
Submitted: 16 April 2012; Accepted: 16 July 2012
Abstract
Objective: There have been very few studies of first-episode psychoses or early intervention programmes in India. This paper describes a pilot intervention programme for first-episode psychosis at the Schizophrenia Research Foundation, India.
Methods: A total of 47 patients with the first episode of psychosis were followed up for 2 years. Based on the Positive and Negative Syndrome Scale for schizophrenia and Global Assessment of Functioning Scale scores, the data from 2 groups of patients, those who had remission and those who did not, were identified and compared. Assessments done at 3, 6, 12 and 24 months after recruitment enabled computation of time to achieve remission.
Results: Complete data were available for 38 patients (28 patients in remission group and 10 patients in non-remission group) at 2 years. Baseline scores were not significantly different between the groups. In the remission group, more than 50% attained maximal improvement at 3 months, another 30% at 1 year, and the remaining 20% at 2 years. Maximal reduction in the mean Positive and Negative Syndrome Scale score was seen between 3 and 6 months after recruitment.
Conclusions: With regular treatment, most patients with early psychosis achieve remission within 2 years. Negative symptoms persisting for longer than 6 months could be an indicator of long-term outcome. Early intervention is feasible and effective in developing countries.
Key words: Early intervention (education); Psychotic disorders; Treatment outcome
摘要
目的:很少有研究关注印度首发思觉失调或早期干预计划。本文阐述印度精神分裂症研究基金会的首发思觉失调试点干预计划。
方法:共47名首发思觉失调患者被纳入研究并随访2年。他们分为缓解组和非缓解组,并以其精神分裂症阳性和阴性症状量表和整体功能评估量表得分作比较。研究并以患者接受治疗後第 3、6、12和24个月的数据,评估他们病情缓解所需时间。
结果:在随访2年後共取得38例完整数据(28例缓解组和10例非缓解组)。两组的基线得分无显著分别。缓解组方面,超过50%於3个月达到最大幅度改善,30%需时1年,其馀20%需时2年,而阳性和阴性症状量表评分在研究开始後3至6个月内的下降幅度最大。
结论:在常规治疗下,大部份患者的病情可於2年内缓解。阴性症状持续时间超过6个月可能是远期治疗效果的指标。在发展中国家,早期干预是可行和有效的。
关键词:早期干预(教育)、思觉失调、治疗效果
Introduction
India was among the first countries in the developing world to formulate a National Mental Health Programme (NMHP), as early as 1982.1 The District Mental Health Programme (DMHP) was started under the NMHP and its implementation was integrated into the National Rural Health Mission providing services through Primary Health Centres. However, the absence of a separate budget for mental health until recently is a reflection on its low priority by policy-makers over the years.2 This has been addressed in the past few years with substantial budgetary allocations being made for the implementation of the DMHP. Shortage of trained mental health professionals has been another major impediment in providing mental health services in rural parts of the country.3,4 Apart from lack of access to affordable care, poor or faulty understanding of the concept of mental illness and limited acceptance of modern treatment options have also been responsible for inadequate service utilisation. This, to an extent, can explain the long duration of untreated psychosis (DUP) reported in several Indian studies over the years. When basic mental health needs are still not fully met, early intervention may not be viewed as a priority service and has not been actively sought by stakeholders. However, the effectiveness of early intervention in reducing long-term disability from severe mental illnesses has been noted. Clearly, more compelling evidence is needed before a policy on early intervention can be developed for India.5 A major part of the health care delivery in India is by the private sector. In the field of mental health, a few non-profit non-governmental organisations (NGOs) also play a role in service delivery. Developing an effective model of early intervention will enable scaling up of the service. This paper discusses the experience and feasibility of conducting a first-episode programme by the NGO Schizophrenia Research Foundation (SCARF).
Being a non-profit organisation based in Chennai for > 25 years, the SCARF is a referral centre for rehabilitation of patients with severe mental disorders and an active research centre. The outpatient department is open in the morning for 5 days a week, and is manned by a multi-professional team. An average of 80 patients is seen weekly and there are facilities to admit about 140 patients.
A first-episode psychosis programme was started at the SCARF in collaboration with the Prevention and Early Intervention Programme for Psychosis (PEPP), Montréal, Canada. The programme aims to achieve early remission through effective interventions, re-integrate patients into mainstream life by improving social and work functioning, and improve therapeutic engagement and prevent relapses. This pilot study aimed to evaluate the course and outcomes of persons with untreated first-episode psychosis, examine the time taken for remission from illness, and assess the changes in symptom domains over a 2-year period.
Methods
Inclusion Criteria
Inclusion criteria were age of < 50 years; a first episode of psychotic illness that satisfied the criteria for a current primary diagnosis of non-affective psychotic disorder (schizophreniform, schizophrenia, schizoaffective, psychosis not otherwise specified) according to the DSM-IV; active psychotic symptoms that met the threshold criteria of the Structured Clinical Interview for the DSM-IV Text Revision7 or a minimum global rating of 3 in at least one of the following dimensions — hallucinations, delusions, or thought disorder — of the Scale for Assessment of Positive Symptoms8 at the time of recruitment; had not received antipsychotic medication for longer than 1 month; ability to communicate in Tamil or English and an intelligence quotient of ≥ 70; and did not have other central nervous system disorders such as epilepsy, psychosis secondary to a medical condition, or a primary diagnosis of substance dependence / abuse. A concurrent diagnosis of substance abuse was not an exclusion criterion as long as psychotic disorder was the primary diagnosis.
Patients
The sample was selected from patients attending the SCARF outpatient department from April 2007 to November 2008; 86% of the patients were from Chennai city and its suburbs, with about 14% from the districts and other parts of India. Of 2075 new patients who attended the outpatient department during the study period, 793 had psychotic illness, of whom 284 had first-episode psychosis; 103 met the study inclusion criteria and 181 were excluded.6 Of these eligible patients, 80 were approached for consent; 33 patients did not consent and the remaining 47 patients who consented were recruited. The study team comprised a psychiatrist, a psychologist, and a social worker.
Assessment Tools
Socio-demographic data were collected on a semi- structured questionnaire. Psychopathology was assessed using the Positive and Negative Syndrome Scale (PANSS) for schizophrenia,9 and functioning was measured using the Global Assessment of Functioning (GAF) Scale.10
Both scales were administered every month for the first 3 months, and subsequently at 6, 9, 12, and 24 months. Both PANSS and GAF were administered by a single rater, a psychiatrist who was trained in the scale and had good inter- rater reliability with the PEPP team in Montréal (κ, -0.83). Structured Clinical Interview for the DSM-IV was used to establish the diagnosis at baseline. At 2 years, patients were categorised as being ‘in remission’ if their PANSS scores were ≤ 60 and GAF scores were > 80.11 Patients who did not fulfil the criteria of being in remission at any point in time during the 2-year period were classified as non-remission. Relapse was defined as re-emergence of at least 1 positive psychotic symptom after a remission period of 4 weeks. Time taken to achieve remission was established in the remission group based on PANSS and GAF assessments conducted at months 3, 6, 12, and 24 months after recruitment. This was done for each of the PANSS subscales for both remission and non-remission groups.
Intervention: Medication
Intervention included medication (usually olanzapine) and a psychosocial component that was delivered by the study psychologist and social worker. The interventions were targeted at both the patient and their caregiver who played a major role in facilitating treatment. The main goals of the intervention were to build a collaborative relationship to facilitate treatment compliance, and improve functioning and quality of life. This included:
- Case management: It aimed to ensure medication compliance, regularity of follow-up, planning and execution of need-based, tailor-made rehabilitation programmes, crisis intervention, home visits, and liaison with the treatment team, family members, and employers. Families of patients were active partners with guidance and support from the case managers. Supportive counselling for patients and their families was also provided. The initial contact focused on imparting awareness about the nature of the illness and the importance of uninterrupted treatment. Subsequent visits focused on persisting symptoms and finer functional difficulties.
- Psycho-education separately for patients and families: the 2 groups were educated about the nature of the illness, with emphasis on the biopsychosocial model, and the effectiveness and need for uninterrupted treatment for a minimum period of 2 years. Psycho- education also included sessions on managing symptoms, identifying relapse, and coping with the illness, stigma, and side-effects of medication.
- Inpatient care for patients with severe illness.
- Psychosocial rehabilitation was done by means of a day care and rehabilitation centre if required. Individual and group sessions on improving communication, self-esteem, problem-solving, decision- making, and coping skills were also provided to the patients. Employment was facilitated by the study team. Cognitive retraining was given to patients who needed improvement in the areas of attention, memory, and executive functioning. When families had difficulty in bringing a patient to the treatment facility for reasons of stigma or unwillingness by the patient, and when phone calls were not fruitful, home visits were made.
Statistical Analysis
The data were analysed for socio-demographic and clinical variables using the Statistical Package for the Social Sciences, version 11.5 (SPSS Inc., Chicago [IL], US).
Results
Patients’ Characteristics
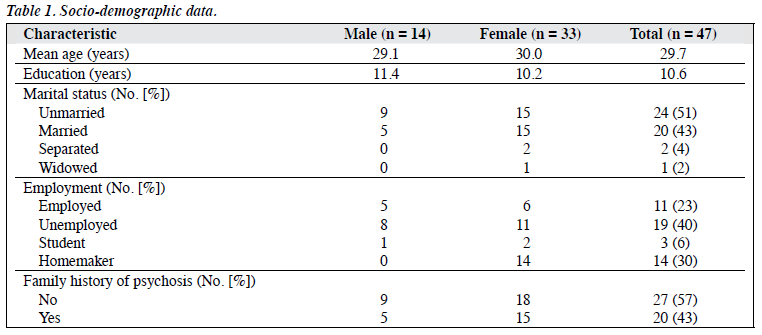
Of the 47 patients who started the study, 38 completed follow-up at 2 years. There were more women (70%) and more than half were single (57%) [Table 1]. The mean age was 29.7 years. Over 40% were unemployed at recruitment. All of the patients lived with their families, and 62% were living with their parents. The patients’ clinical characteristics are shown in Table 2. Of the 9 patients who were not available for assessment, 1 man had died, 2 moved away from Chennai, 1 withdrew consent, 4 who lived outside Chennai expressed inability to continue the study, and 1 moved to a different centre for treatment. The data were analysed for the remaining 38 patients.
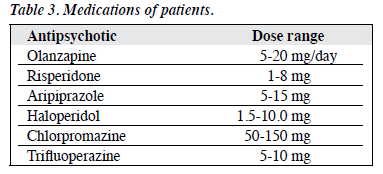
Among the 47 patients at baseline, 22 were taking a single antipsychotic and the others were taking > 1 antipsychotic, at least for 1 to 2 weeks. Olanzapine was the first choice of antipsychotic in most patients (n = 36) [Table 3]. Only a small number of patients (n = 6) needed hospitalisation during the study period and the duration of inpatient stay ranged from 1 to 4 months. Five of the 6 admissions happened in the first 2 months after recruitment. Intensive rehabilitation in day care was generally not required. Home visits were needed in 17 instances and were mostly successful in improving therapeutic engagement, although 1 patient was temporarily lost to follow-up and was re-engaged when she returned after 24 months.
Course and Outcome
Cross-sectional assessment made after 2 years showed that 28 patients were in remission and 10 remained symptomatic. No significant differences in socio-demographic and clinical profiles at baseline were found between the 2 groups. The DUP of the 2 groups differed significantly, with a mean of 11.4 months for the remission group and 56.5 months for the non-remission group (t = 4.05, p = 0.002). For the entire sample, there was a significant improvement in mean PANSS score from baseline (89.10) to year 1 (54.22), but this difference was not sustained between years 1 and 2. The GAF scores significantly improved from 35.55 at baseline to 63.5 at year 1 (t = 8.005, p < 0.001), but the improvement from year 1 to year 2 (68.6) was not significant (t = 1.06, p= 0.27).
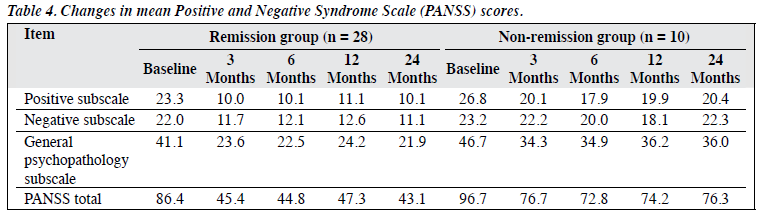
The mean PANSS score of the remission group at baseline was lower than that of the non-remission group (86.4 vs. 96.7), but this difference did not reach statistical significance. Although 8 patients in the remission group experienced a relapse at some point between 3 and 24 months, they reached remission at the end of 24 months when the final assessments were made.
Time Taken for Remission
Among the remission group, just over 50% attained remission at 3 months; by 1 year, another 30% had achieved remission (Fig). In the remission group, all the PANSS subscale scores showed a reduction from baseline over time. The mean positive subscale score was reduced maximally at month 3 (from 23.3 at baseline to 10.0), and subsequent reductions were minimal. The mean negative subscale score reduced by 47% at month 3 and by almost 50% at 2 years. A maximum reduction of mean scores for the general psychopathology subscale was seen at year 2.
In the non-remission group, the mean positive subscale score reduced maximally (33%) at 6 months; at 2 years the symptom reduction was 24% from baseline. Improvement in the negative subscale score was much less, with maximum reductions of 22% at 1 year and 4% at 2 years compared with baseline. A maximum reduction was seen at 3 months for the general psychopathology subscale score, but this had worsened at 2 years. Overall, the non- remission group showed a maximum of 25% improvement at 6 months, then reduced to 21% at 2 years versus 50% improvement seen in the remission group (Table 4).
Of the 28 patients in the remission group, 17 were adherent to the prescribed medication for > 75% of the study period (13 were fully adherent); only 2 patients had < 50% adherence. Nine patients remained well without medication at the end of the second year. Of the 10 patients in the non- remission group, 5 were never taking regular medication and only 3 were > 75% adherent to prescription medication.
Discussion
The first major finding of this study was that 63.8% of patients improved with treatment at the end of 2 years. This was comparable with the improvement rate of 63.1% reported in rural Chandigarh in the Determinants of Outcome of Severe Mental Disorders study,12 as well as that of 69% in the Vellore Centre Study of Factors Affecting the Course and Outcome of Schizophrenia.13 Another study from Vellore reported a 50% remission rate at 1 year.14
Maximal improvement was seen at 3 months from baseline in this study. Studies showed that short-term positive outcomes in treatment-naïve schizophrenia patients were up to 62% in Indian settings.15 More recently, it was demonstrated that good improvement was seen early in treatment and the plateauing of psychopathology after 6 months.14 Although shorter DUP could be a contributing factor, it is not the only reason for early improvement. In the same sample of a previous study,6 patients with longer DUP showed significant improvement in the early stages between 3 and 6 months. The PANSS scores at baseline were not significantly different between the remission (86.4) and non-remission (96.7) groups, therefore PANSS score is not indicative of outcome at 1 and 2 years. This is similar to other Indian studies whereby scores on psychopathology at baseline did not predict outcome.14 It appears that positive symptoms tend to go into remission earlier, while negative symptoms take a longer time to achieve remission. In the present study, 50% or more reduction in symptoms on the positive subscale was seen within 3 months for most patients in the remission group. The reduction was less for the negative subscale, and this was more so in the non- remission group. Negative symptoms persisting for longer than 6 months despite treatment could be an indicator of long-term outcome. This is consistent with the findings in the Madras Longitudinal Study16 in which more of the typical antipsychotics were used, while most of these patients in the present study were taking atypical antipsychotics, which are thought to be efficacious in reducing negative symptoms.
Although taking a longer time, improvement was also seen in the non-remission group. However, those patients achieving quicker remission of symptoms on the positive and negative subscales tended to have better final improvement; while persisting or worsening negative symptoms for longer than 6 months were associated with delayed or non-remission. This group may therefore require more intensive and longer intervention, with a focus on negative symptoms.
Adherence to medication appears to be a key factor affecting improvement. Ensuring adherence was an important management issue. Patients and their families believed that medications used in psychiatry are highly sedative, habit- forming, and could impair memory and cognition, affect productivity, and render a person unproductive. This was in addition to fear of developing physical problems as side- effects of long-term use of medicines. Patients also felt ‘labelled’ when taking a prescription drug. All these issues needed to be addressed during the first visit. Restricting the number of medicines to < 3, preferably taken as a single dose at night, ensured better adherence. For most patients, their families closely supervised their intake of medication. Pill counts, ensuring refills at the end of the stock without delay, were documented and adherence achieved. Taking medicines for 75% or more of time since the previous visit was considered good adherence. Ensuring adherence to medication and involving the families are critical to the efforts involved in early intervention.
Sex differences could not be statistically assessed due to the disproportionate distribution. However, the sexes were comparable for age, education level, DUP, and baseline PANSS scores. Both sexes showed similar patterns of improvement from baseline to 1 year, and less improvement from 1 year to 2 years. Women had better GAF scores at baseline, and remained so at the end of 2 years. As in many developing countries, the men were largely unemployed at baseline, while the women, who were primarily homemakers, were more productive. It was easier to engage women in the intervention programme.
Limitations
Since the sexes were not equally represented, this study was not able to make a satisfactory comparison in this aspect. Information on dropouts was not complete because of logistical problems. For the purposes of this paper, PANSS score of ≤ 60 and GAF score of > 80 were used to denote remission instead of the more widely used consensus operational criteria put forward by the Remission of Schizophrenia Working Group.17 It is proposed to use the consensus operational criteria in subsequent analyses.
Challenges
As the SCARF is predominantly a referral centre, it does not attract too many first-episode patients. Most people who attend have been treated before. In Chennai, with several places available to choose for treatment in the state and private sectors, patients and families tend to move from one place to another in search of instant results, especially when the duration of illness is short. This posed difficulties in ensuring that patients stayed engaged in treatment. Distance also played a key role in follow-up. Some patients dropped out for financial reasons despite consultation and psychosocial services provided at no cost. The quality of time and psycho-education given to families during the first contact could to a certain extent ensure sustained therapeutic engagement. Telephone calls made between visits (either to the patient or the caregiver) also went a long way in building rapport and maintaining therapeutic engagement. Reminders about review appointments or rescheduling appointments if needed also helped.
Young unmarried women tend to disengage from treatment due to the stigma of contact with a mental health facility and its impact on marriage prospects. When they are married, continuing contact becomes harder. Death or illness of a primary caregiver sometimes causes setbacks in regularity of treatment. Establishing contact with at least 1 family member other than the primary caregiver has helped to ensure uninterrupted treatment.
Conclusions
Early intervention helps in improving outcome for all patients irrespective of duration of psychosis. Shorter periods of illness have better results, emphasising the usefulness of early intervention. Persisting or worsening negative symptoms at 6 months can be an indicator of long- term outcome and needs more attention during intervention. Providing adequate medical and psychosocial treatment in the community with active participation of the family will be the most efficient and cost-effective mode of service in India. Educating and involving the families from the beginning of treatment will help to improve outcomes. Families and patients in developing countries place a premium on functional improvement in the absence of welfare benefits for mentally disabled people.18,19 Promoting awareness about the advantages of seeking help early will be of benefit. A large section of the Indian population is still unaware of basic mental health issues or the medical basis of mental illnesses.20 Promoting mental health awareness through campaigns for various sections of society should therefore be the primary focus. Also, awareness of early intervention should be promoted to specific groups such as general practitioners, family physicians, faith healers, and teachers of schools and colleges who are likely to be the first contact in the early stages of psychosis. Mass education through media and social networks will have a lasting impact and also be cost-effective.
Acknowledgements
We thank Ms Sushma Ramesh Kumar and Ms Anitha Jeyagurunathan who assisted with the data collection and the implementation of the intervention programme. We also thank all our patients and families for continuing in the programme despite some difficulties.
Declaration
The project was supported by a grant from the Douglas Hospital Research Centre, Montréal, Canada.
References
- Murthy RS. Mental health initiatives in India (1947-2010). Natl Med J India 2011;24:98-107.
- Kumar A. History of mental health services in India. J Pers Clin Stud 2004;20:1-2.
- Tirupati NS, Rangaswamy T, Raman P. Duration of untreated psychosis and treatment outcome in schizophrenia patients untreated for many years. Aust N Z J Psychiatry 2004;38:339-43.
- Thirthalli J, Channaveerachari NK, Subbakrishna DK, Cottler LB, Varghese M, Gangadhar BN. Prospective study of duration of untreated psychosis and outcome of never-treated patients with schizophrenia in India. Indian J Psychiatry 2011;53:319-23.
- Keshavan MS, Shrivastava A, Gangadhar BN. Early intervention in psychotic disorders: challenges and relevance in the Indian context. Indian J Psychiatry 2010;52(Suppl 1):S153-8.
- Rangaswamy T, Mangala R, Mohan G, Joseph J, John S. Intervention for first episode psychosis in India — The SCARF experience. Asian J Psychiatr 2012;5:58-62.
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition with psychotic screen (SCID-I/P W/ PSY SCREEN). New York: Biometrics Research, New York State Psychiatric Institute; 2002.
- Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS). Iowa City: Department of Psychiatry, University of Iowa College of Medicine; 1984.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76.
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976;33:766-71.
- 1 Opler MG, Yang LH, Caleo S, Alberti P. Statistical validation of the criteria for symptom remission in schizophrenia: preliminary findings. BMC Psychiatry 2007;7:35.
- Sartorius N, Jablensky A, Korten A, Ernberg G, Anker M, Cooper JE, et al. Early manifestations and first-contact incidence of schizophrenia in different cultures. A preliminary report on the initial evaluation phase of the WHO Collaborative Study on determinants of outcome of severe mental disorders. Psychol Med 1986;16:909-28.
- Verghese A, John JK, Rajkumar S, Richard J, Sethi BB, Trivedi JK. Factors associated with the course and outcome of schizophrenia: results of a two year follow up study. Br J Psychiatry 1989;154:499-503.
- Saravanan B, Jacob KS, Johnson S, Prince M, Bhugra D, David AS. Outcome of first-episode schizophrenia in India: longitudinal study of effect of insight and psychopathology. Br J Psychiatry 2010;196:454-9.
- Philip M, Gangadhar BN, Jagadisha, Velayudhan L, Subbakrishna DK. Influence of duration of untreated psychosis on the short-term outcome of drug-free schizophrenia patients. Indian J Psychiatry 2003;45:158-60.
- Thara R. Twenty-year course of schizophrenia: the Madras Longitudinal Study. Can J Psychiatry 2004;49:564-9.
- Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 2005;162:441-9.
- Isaac M, Chand P, Murthy P. Schizophrenia outcome measures in the wider international community. Br J Psychiatry Suppl 2007;50:s71-7.
- Thara R, Rajkumar S. Nature and course of disability in schizophrenia. Indian J Psychiatry 1993;35:33-5.
- Gupta PR, Chakrabarti S, Kulhara P. Lack of association between duration of untreated psychosis and outcome in an Indian cohort. World Psychiatry 2010;9:124-5.