East Asian Arch Psychiatry 2013;23:37-44
ORIGINAL ARTICLE
Dr Dorothy Y. Y. Tang, MBBS, MRCPsych, Department of Forensic Psychiatry, Castle Peak Hospital, New Territories, Hong Kong SAR, China.
Dr Amy C. Y. Liu, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Forensic Psychiatry, Castle Peak Hospital, New Territories, Hong Kong SAR, China.
Ms Michelle H. T. Leung, PGDip (Psychology), MA, BBA, Department of Psychiatry, The University of Hong Kong, Hong Kong SAR, China.
Dr Bonnie W. M. Siu, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Forensic Psychiatry, Castle Peak Hospital, New Territories, Hong Kong SAR, China.
Address for correspondence: Dr DYY Tang, Department of Forensic Psychiatry, Castle Peak Hospital, No. 15 Tsing Chung Koon Road, Tuen Mun, New Territories, Hong Kong SAR, China.
Tel: (852) 24567111; Fax: (852) 24559330; Email: tyy551@ha.org.hk
Submitted: 18 February 2013; Accepted: 13 May 2013
Abstract
Objective: Antisocial personality disorder (ASPD) is a risk factor for violence and is associated with poor treatment response when it is a co-morbid condition with substance abuse. It is an under-recognised clinical entity in the local Hong Kong setting, for which there are only a few available Chinese-language diagnostic instruments. None has been tested for its psychometric properties in the Cantonese-speaking population in Hong Kong. This study therefore aimed to assess the reliability and validity of the Chinese version of the ASPD subscale of the Structured Clinical Interview for the DSM-IV Axis II Disorders (SCID-II) in Hong Kong Chinese.
Methods: This assessment tool was modified according to dialectal differences between Mainland China and Hong Kong. Inpatients in Castle Peak Hospital, Hong Kong, who were designated for priority follow- up based on their assessed propensity for violence and who fulfilled the inclusion criteria for the study, were recruited. To assess the level of agreement, best-estimate diagnosis made by a multidisciplinary team was compared with diagnostic status determined by the SCID-II ASPD subscale. The internal consistency, sensitivity, and specificity of the subscale were also calculated.
Results: The internal consistency of the subscale was acceptable at 0.79, whereas the test-retest reliability and inter-rater reliability showed an excellent and good agreement of 0.90 and 0.86, respectively. Best- estimate clinical diagnosis–SCID diagnosis agreement was acceptable at 0.76. The sensitivity, specificity, positive and negative predictive values were 0.91, 0.86, 0.83, and 0.93, respectively.
Conclusion: The Chinese version of the SCID-II ASPD subscale is reliable and valid for diagnosing ASPD in a Cantonese-speaking clinical population.
Key words: Antisocial personality disorder; Hong Kong; Psychiatric status rating scales; Validation studies
摘要
目的:反社会人格障碍是暴力行为的危险因子,其与药物滥用的合併症也可导致治疗效果欠佳。在香港,由於相关的中文诊断工具有限,在日常的临床工作中,反社会人格障碍常被忽视。直至现时,香港仍未有测试粤语人口心理测量学的相关研究。因此,本研究旨在评估DSM-IV结构式诊断晤谈量表反社会型人格障碍子量表(中文版)的信度和效度。
方法:评估工具根据中国内地和香港之间的方言差异作出适度修改,对象为因被评有暴力倾向而纳入优先随访且符合研究标準的香港青山医院住院病人。研究检视跨部门小组的最佳估计诊断跟评估工具诊断的一致性,以及此子量表的内部一致性、敏感性和特异性。
结果:此子量表其内部一致性在0.79的可接受水平,而再测信度和评分者间信度皆优异,分别为0.90和0.86。最佳估计诊断和评估工具诊断的一致度为0.76的可接受水平。敏感性、特异性、阳性和阴性预测值分别为0.91、0.86、0.83和0.93。
结论:DSM-IV结构式诊断晤谈量表反社会型人格障碍子量表(中文版)能可靠和有效地诊断反社会人格障碍。
关键词:反社会人格障碍、香港、精神病状态评定量表、效度研究
Introduction
Violence, according to the Cambridge Advanced Learner’s Dictionary, is defined as “actions or words which are intended to hurt people”. Antisocial personality disorder (ASPD) is described by the DSM-IV-TR as a pervasive pattern of disregard for, and violation of, the rights of others that begins in childhood and persists through adulthood.1 Many studies have found that patients with mental disorders, especially those with a diagnosis of ASPD, are more likely to be engaged in aggressive acts.2-6 A study in Finland indicated that while schizophrenia increased the odds ratio of homicidal violence by approximately 8-fold in men and 6.5-fold in women, ASPD increased the odds ratio by over 10-fold in men and over 50-fold in women.7 The prevalence of any personality disorder in self- reported violent incidents in Britain over a 5-year period was reported to be 29%, while ASPD was reported to be 4 times more likely to result in injury to a victim compared with other personality disorders.8 Moreover, ASPD further triples the risk of violence in an individual intoxicated with alcohol or drugs.8 Individuals with ASPD demonstrated strong association with injury in victims including family, partner, known persons, strangers and police, etc, and their violence was shown to be repetitive in terms of incidents and different victims.9
Cluster B personality disorders, including ASPD, are associated with an increased risk of early institutional care, criminal conviction, and imprisonment. This cluster of personality disorder is positively correlated with functional psychosis, affective / anxiety disorder, and alcohol dependence.4 Antisocial personality disorder itself was significantly associated with poor treatment outcome and persistent alcohol, cannabis, and nicotine use disorders.10
The relationship between ASPD and criminal conviction was reconfirmed in another large-scale review undertaken by Fazel and Danesh in 2002.11 This systematic review of 62 surveys involving 22,790 prisoners suggested that compared with the general American or British population of similar age, prisoners have about a 2- to 4-fold excess of psychotic illness or major depression, and about a 10-fold excess of ASPD.11
It is believed that the rate of ASPD fluctuates significantly across different settings. Epidemiological studies in western countries identified an ASPD prevalence between 0.6 and 3.6% in community samples,12 3.6% among psychiatric outpatients,13 from 3.5 to 18.2% in psychiatric inpatients,14,15 and as high as 78% and 50% among male and female prisoners, respectively in England and Wales.16 This disorder is 4 to 5 times more common in men than in women.2,17
Antisocial personality disorder is a relatively under- researched topic among the Chinese population. From the limited available data, great variability in its prevalence across different settings is observed. While the prevalence was 0.3% in a community sample in Taiwan,18 and 0.2 to 0.8% in a group of psychiatric outpatients in Shanghai,19 another study identified 14% of patients attending a psychological counselling centre in Shanghai as having ASPD.20 In a mass screening for personality disorders in South China, 67% of 2961 prison inmates were identified as having ASPD.21
In Hong Kong, a priority follow-up (PFU) system was established in 1982 aiming to facilitate close monitoring of patients with mental disorders with a propensity to violence or a record of criminal violence. Whereas patients with minimal violent propensity would be allocated into the non-PFU group, attending psychiatrists would categorise patients with a risk of violence into either the target group or sub-target (PFU-ST) group, according to the level of propensity to violence. Patients considered as posing a lower risk of violence or who had committed less serious offences previously were categorised into the target group. Those who were regarded as posing a higher risk or who had committed more serious offences in the past were categorised into the PFU-ST group.22 The status of PFU target patients was reviewed at least annually by the attending psychiatrist, while the PFU-ST group patients were to have their clinical condition discussed and their status reviewed at a multidisciplinary meeting at least once yearly. Experience in western settings suggested that PFU or similar systems could help to reduce relapse or re- hospitalisation rates, minimise the risk of violence, and control psychotic symptoms.23-26
As ASPD is an important risk factor for violence in patients with mental disorders and has a high co-morbidity with Axis I disorders, it is important to identify the diagnosis for better risk assessment and treatment. A structured clinical interview is a useful tool in enhancing validity and reliability in making a diagnosis of ASPD.
Diagnostic Tools for Personality Disorders
Several standardised diagnostic tools for personality disorders based on the DSM-IV or the ICD-10 have been translated into Chinese and validated in Mainland China among the Mandarin-speaking population (Table 127-30). Of these 4 existing instruments, the Structured Clinical Interview for the DSM-IV Axis II Disorders (SCID- II) is the only tool which allows interviewers to use one of the subscales to study a particular type of personality disorder (e.g. paranoid personality disorder, ASPD, schizoid personality disorder, etc). This helps to shorten the assessment time because the researcher does not need to perform the whole test when they would like to focus on a particular type of personality disorder. To date, only the Borderline Personality Disorder subscale in SCID-II has been validated in a Chinese (Cantonese speaking) population in Hong Kong.31
We believe that validation of the ASPD subscale (SCID-II ASPD) would assist future researchers in accurate identification of ASPD by this structured clinical interview. The original version of SCID-II entails a semi-structured face-to-face interview developed at the US New York State Psychiatric Institute.32 It starts with a brief overview on the subject’s usual behaviours and relationships. The interviewer needs to ensure that the pattern of behaviour fulfils the following criteria: (i) being an enduring pattern of inner experience that is stable, of long duration, and with the onset being traceable back at least to adolescence or early adulthood; (ii) deviating markedly from the expectations of the individual culture; (iii) leading to clinically significant distress or impairment in social, occupational, or other important areas of functioning; and (iv) not better accounted for as a manifestation or consequence of another mental disorder, substance or a general medical condition. Apart from the above general requirements for the diagnosis of a personality disorder, the SCID-II ASPD subscale comprises 23 items corresponding to the DSM-IV diagnostic criteria (Appendix) under the umbrella of 3 criteria. Criterion A consists of 7 items which aim to delineate a pervasive pattern of disregard for, and violation of, the rights of others occurring since the age of 15 years. Criterion B requires the subject to be at least 18 years. Criterion C consists of 15 items on the evidence for conduct disorder with onset before the age of 15 years. In order to assess whether the subject reaches the threshold of a particular item, there is an initial interview question followed by several predetermined follow-up questions for each item. Then, the interviewer codes each item with either 1, 2, or 3 through clinical judgement based on information provided by the subjects (1 = absent, 2 = subthreshold, 3 = threshold or true). A rating of 3 is warranted only if the threshold for the criterion is met, with the subject providing a convincing elaboration or example, or if there was clear evidence from the behaviours encountered during the interview. For instance, regarding item 7 (lack of remorse) in criterion A, as indicated by being indifferent to or rationalising having hurt, mistreated, or stolen from another; a rating of 3 would be warranted in the SCID-II ASPD subscale if a person lacks remorse about the consequences of his / her antisocial act(s), often blaming the victim(s) as being foolish, helpless, or deserving of their fate, or else minimising the harmful consequences. Subjects aged ≥ 18 years (criterion B), together with those meeting ≥ 2 items in criterion C and ≥ 3 items in criterion A, were assessed as having ASPD. In its original design, the subject interviewed is usually the sole source of information. However, ancillary data from other sources, for example, collateral information from a current or previous therapist or family member, are also permitted.
The Chinese version of the SCID-II was developed by the Shanghai Mental Health Center in 2006.27 The original English version was translated into Mandarin and was back-translated into English for testing of its psychometric properties. Cultural factors were also taken into consideration in the translation and revision process. The ASPD subscale demonstrated an internal consistency with a coefficient of 0.66; the kappa values for inter-rater reliability and test-retest reliability were not calculated due to low prevalence.
In view of the cultural and dialectal differences between Mandarin-speaking Chinese and Hong Kong Chinese, the present study aimed to evaluate the applicability of this instrument for the Cantonese-speaking Chinese population in Hong Kong, including the assessment of its reliability, validity, and measurement of the internal consistency and the level of agreement between best-estimate clinical diagnosis and the SCID-II ASPD diagnosis using the kappa value. The sensitivity and specificity of the SCID-II ASPD subscale were also calculated.
Methods
Sample Size Estimation
With the assumption of ASPD prevalence of 18% from a previous study in Norway,15 the number of subjects required to detect a statistically significant kappa coefficient would be between 62 and 77.33 It was thus determined that 77 subjects would be recruited into the current study.
Expert Panel Agreement and Pilot Assessment
Although written Chinese (either traditional or simplified characters) is universal among Chinese populations, different dialects are used in Mainland China / Shanghai (Mandarin) and Hong Kong (Cantonese). Therefore, some items in the Mandarin version of the SCID-II ASPD subscale developed in Shanghai were modified for ease of understanding by Hong Kong Chinese in this study. This modified version was reviewed by an expert panel consisting of 5 health care professionals from different disciplines, including a psychiatrist, a nurse, an occupational therapist, a clinical psychologist, and a social worker. The panel members were required to have at least 3-year experience in the psychiatric service in Hong Kong. This was to ensure that the panel members would have adequate experience with local psychiatric patients in order to give accurate comment on their ability to comprehend the meaning of wording used in the subscale. After the panel members agreed on the content validity of the items, the final version was pilot- tested by convenience sampling of 5 inpatients in a forensic psychiatric ward of Castle Peak Hospital (CPH). Practical problems, such as difficulty in understanding the wording of certain items, were subsequently addressed.
Recruitment
All inpatients labelled as PFU-ST cases in CPH as of 19 June 2012 were invited to participate in the study. Patient inclusion criteria were: (a) aged between 18 and 64 years; (b) Chinese ethnicity; and (c) mentally fit to provide written informed consent for participation in the study. Exclusion criteria included: (a) moderate or severe mental retardation; (b) unable to comprehend Cantonese; and (c) physically unsuitable for interview.
Data Collection
Demographic data including age, sex, marital status, as well as the principal diagnosis were retrieved from the inpatient case notes. Each subject was interviewed by a multidisciplinary team formed by experienced psychiatrists, nursing staff, clinical psychologists, occupational therapists, and social workers to evaluate whether he / she fulfilled the diagnostic criteria for ASPD according to the DSM-IV. The assessment result served as the gold standard for the ASPD diagnosis. Assessment using the SCID-II ASPD subscale was then carried out by a trained rater within 1 month of the assessment by the multidisciplinary clinical team. The rater was blind to the assessment result by the multidisciplinary team when the SCID-II ASPD was carried out. The rater was not permitted to obtain other sources of information to ensure that the outcome of the assessment was based solely from the information obtained during the interview.
Test-retest Reliability and Inter-rater Reliability
To evaluate test-retest reliability, a group of patients were randomly selected for the retest of the SCID-II ASPD subscale by the same rater within 2 weeks of the first assessment. To assess inter-rater reliability, another group of randomly selected patients was retested by a second trained rater. The retests were conducted within 2 weeks of the first assessment to minimise the effect of change in mental state.
Data Analysis
Data were analysed using the Statistical Package for the Social Sciences, Windows version 17.0. The ASPD diagnostic status established by the SCID-II ASPD subscale and multidisciplinary clinical assessment was compared, with a p < 0.05 considered statistically significant. The level of agreement, expressed as kappa value, was calculated. The sensitivity, specificity, as well as positive and negative predictive values for ASPD diagnoses established by the assessment tool were calculated. The internal consistency of the ASPD subscale, expressed as Cronbach’s alpha coefficient, was computed. The test-retest reliability and inter-rater reliability were also calculated.
Ethical Considerations
Ethical approval was obtained from the New Territories West Cluster Clinical and Research Ethics Committee. Written consent was obtained from all subjects. Subjects could withdraw from the study at any time.
Results
Demographic Characteristics
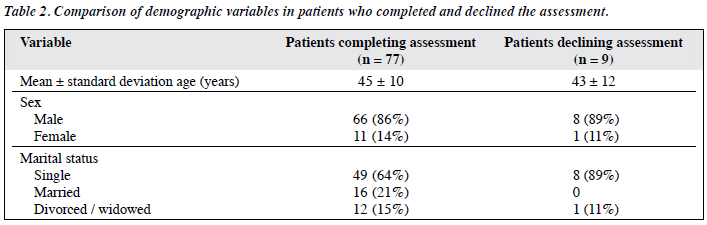
A total of 86 inpatients at CPH were both labelled as PFU-ST and fulfilled the inclusion criteria as of 19 June 2012. Of these, 9 (10%) patients declined to participate in the present study. The remaining 77 patients gave informed consent and completed the study, including 66 males (86%) and 11 females (14%). The mean (± standard deviation) age was 45 ± 10 years. For marital status, 49 (64%) were single, 16 (21%) were married, and the remaining were either divorced (10%) or widowed (5%). As shown in Table 2, the demographic characteristics were similar in those agreed or declined to participate in this study.
Principal Diagnosis
The principal Axis I diagnosis was obtained from the case notes. The majority of subjects (87%) were diagnosed as having schizophrenia or related psychotic disorder. The remaining subjects were diagnosed with epilepsy (4%), mental retardation (4%), substance- or alcohol-related disorder (3%), or mood disorder (2%).
Assessment Results
The internal consistency (expressed as Cronbach’s alpha coefficient) of the SCID-II ASPD subscale was 0.79. Since this value was greater than 0.70, it was considered acceptable.34
A total of 20 subjects were randomly selected to be interviewed for establishing test-retest reliability. Table 3 shows the distribution of the SCID-II ASPD diagnoses. The kappa value was 0.90 indicating excellent agreement.
A total of 14 patients were randomly selected to be assessed by the second rater, and the distribution of the SCID-II ASPD diagnoses is shown in Table 4. The kappa value was 0.86, indicating good agreement between the 2 raters.
Of those 77 subjects, 33 (43%) were diagnosed to have ASPD by the multidisciplinary team, while 36 (47%) were diagnosed with ASPD by the SCID-II ASPD subscale. The kappa value reflecting the level of agreement was 0.76. Table 5 shows the distribution of diagnoses under these 2 methods of assessment. The SCID-II ASPD subscale demonstrated satisfactory sensitivity (0.91), specificity (0.86), as well as positive predictive (0.83) and negative predictive (0.93) values.
Discussion
In this study, subjects were intentionally recruited from a clinical population with a propensity to violence or a history of serious criminal offending. A higher base rate of ASPD was postulated compared with other sources of subject recruitment. This sampling method was deliberately chosen because a sample with a low base rate might lead to unstable kappa values.35 It has been recommended that the kappa value should only be calculated if the frequency of the item tested for agreement is more than 5%.36 The relatively high base rate of ASPD in our sample (33%) was not only sufficient to estimate a kappa value, but also ensured that parameters such as sensitivity, specificity, as well as positive and negative predictive values could be calculated for the assessment tool.
The agreement between the best-estimate clinical diagnosis and the SCID-II ASPD diagnosis was acceptable, indicating that this assessment tool could safely differentiate patients who suffer from ASPD from those who do not, to the level of accuracy of the clinical diagnosis made by a multidisciplinary team. Furthermore, as the administration mainly involves direct reading-out verbatim, this helps to minimise any inconsistency in the diagnostic process. The stability of this assessment tool is also reflected in its excellent test-retest reliability, good inter-rater reliability, and satisfactory internal consistency. The satisfactory sensitivity, specificity, positive and negative predictive values, as measured against the clinician’s best-estimate diagnosis, were comparable to those obtained in other studies.27,37
Given the well-known association of ASPD with violence in psychiatric patients, this assessment tool may also prove reliable and invaluable in providing an accurate diagnosis of ASPD in daily clinical practice to facilitate appropriate patient management and follow-up.
Limitations
There are several limitations in this study. Firstly, a representative prevalence of ASPD among the inpatients of CPH could not be generated due to the method of subject selection. Secondly, as the Mandarin version was directly adopted and back-translation was not performed, its consistency with the English version could not be guaranteed. Thirdly, notwithstanding that the subjects were recruited from psychiatric inpatients labelled PFU-ST to ensure a high base rate of ASPD, i.e. a stable kappa value, this may affect generalisability to a community sample. Furthermore, given the high prevalence of psychosis in the inpatient sample and the age range set in the inclusion criteria, the results cannot be generalised to a non-psychotic population or those aged > 65 years or < 18 years. Fourthly, because of the small sample size, factor analysis could not be performed to test for the factor structure of the SCID-II ASPD subscale.
Conclusion
In this study, the Chinese version of the SCID-II ASPD subscale demonstrated good face validity and content validity in a Cantonese-speaking Chinese population in Hong Kong. It appears a reliable instrument for diagnosing ASPD in Cantonese speakers in both clinical and research settings. It could also be used to determine the prevalence of ASPD in a Cantonese-speaking clinical population or in community epidemiological studies.
References
- Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision. Washington, DC: American Psychiatric Association; 1994.
- Coid J. Epidemiology, public health and the problem of personality disorder. Br J Psychiatry Suppl 2003;44:S3-10.
- Coid J, Yang M, Roberts A, Ullrich S, Moran P, Bebbington P, et al. Violence and psychiatric morbidity in a national household population — a report from the British Household Survey. Am J Epidemiol 2006;164:1199-208.
- Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder in Great Britain. Br J Psychiatry 2006;188:423-31.
- Moran P, Walsh E, Tyrer P, Burns T, Creed F, Fahy T. Impact of comorbid personality disorder on violence in psychosis: report from the UK700 trial. Br J Psychiatry 2003;182:129-34.
- Samuels J, Eaton WW, Bienvenu OJ 3rd, Brown CH, Costa PT Jr, Nestadt G. Prevalence and correlates of personality disorders in a community sample. Br J Psychiatry 2002;180:536-42.
- Eronen M, Hakola P, Tiihonen J. Mental disorders and homicidal behavior in Finland. Arch Gen Psychiatry 1996;53:497-501.
- Coid J, Yang M, Roberts A, Ullrich S, Moran P, Bebbington P, et al. Violence and psychiatric morbidity in the national household population of Britain: public health implications. Br J Psychiatry 2006;189:12-9.
- Samuels J. Personality disorders: epidemiology and public health issues. Int Rev Psychiatry 2011;23:223-33.
- Hasin D, Fenton MC, Skodol A, Krueger R, Keyes K, Geier T, et al. Personality disorders and the 3-year course of alcohol, drug, and nicotine use disorders. Arch Gen Psychiatry 2011;68:1158-67.
- Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet 2002;359:545-50.
- Barry KL, Fleming MF, Manwell LB, Copeland LA. Conduct disorder and antisocial personality in adult primary care patients. J Fam Pract 1997;45:151-8.
- Zimmerman M, Rothschild L, Chelminski I. The prevalence of DSM-IV personality disorders in psychiatric outpatients. Am J Psychiatry 2005;162:1911-8.
- Oldham JM, Skodol AE, Kellman HD, Hyler SE, Rosnick L, Davies M. Diagnosis of DSM-III-R personality disorders by two structured interviews: patterns of comorbidity. Am J Psychiatry 1992;149:213-20.
- Dahl AA. Some aspects of the DSM-III personality disorders illustrated by a consecutive sample of hospitalized patients. Acta Psychiatr Scand Suppl 1986;328:61-7.
- Singleton N, Meltzer H, Gatward R. Psychiatric morbidity among prisoners in England and Wales. London: Office for National Statistics; 1998.
- Moran P. The epidemiology of antisocial personality disorder. Soc Psychiatry Psychiatr Epidemiol 1999;34:231-42.
- Zoccolillo M, Price RK, Ji TH, Hwu HG. Antisocial personality disorder: comparisons of prevalence, symptoms, and correlates in four countries. In: Cohen P, Slomkowski C, Robins LN. Historical and geographical influences on psychopathology. Routledge; 1999: 249-77.
- Zhang TH, Xiao ZP, Wang LL, Dai YF, Zhang HY, Qiu JY, et al. A cross-sectional survey on personality disorder in mental disorder outpatients in Shanghai [in Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi 2010;31:933-7.
- Zhang TH, Xiao ZP, Wang LL, Dai YF, Zhang HY, Qiu JY. Distribution of personality disorder tendency of outpatients in psychological counseling [in Chinese]. Chin Ment Health J 2009;23:767-71.
- Cai J, Gu Y, Yao S. Screening for personality disorders among Chinese prison inmates. Psychiatr Serv 2010;61:947.
- Psychiatric services of Hospital Authority. Press release. November 3, Available from: http://www.info.gov.hk/gia/general/201011/03/P201011030255.htm. Accessed 25 April 2013.
- Chiu SN, Poon TN, Fong SY, Tsoh MY. A review of 354 outreach patients of the Kwai Chung Hospital community psychiatric team. Hong Kong J Psychiatry 2000;10:6-13.
- Dvoskin JA, Steadman HJ. Using intensive case management to reduce violence by mentally ill persons in the community. Hosp Community Psychiatry 1994;45:679-84.
- McRae J, Higgins M, Lycan C, Sherman W. What happens to patients after five years of intensive case management stops? Hosp Community Psychiatry 1990;41:175-9.
- Stein LI, Test MA. Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Arch Gen Psychiatry 1980;37:392-7.
- Dai Y, Xiao Z, Wang Z. The reliability and validity of a Chinese version of the Structured Clinical Interview for DSM-IV personality disorders. Shanghai Archives of Psychiatry 2006;18:1-4.
- Han J, Xu Y, Cui Y. Evaluation on reliability and validity of the Chinese version of International Personality Disorder Examination. Chinese Journal of Psychiatry 1998;31:172-4.
- Yang J, McCrae RR, Costa PT Jr, Yao S, Dai X, Cai T, et al. The cross- cultural generalizability of Axis-II constructs: an evaluation of two personality disorder assessment instruments in the People’s Republic of China. J Pers Disord 2000;14:249-63.
- Yang Y, Shen D, Wang J. The reliability and validity of PDQ-4+ in China. Chinese Journal of Clinical Psychology 2002;10:165-8.
- Wong HM, Chow LY. Borderline personality disorder subscale (Chinese version) of the structured clinical interview for DSM-IV axis II personality disorders: a validation study in Cantonese-speaking Hong Kong Chinese. East Asian Arch Psychiatry 2011;21:52-7.
- First MB, Gibbon MG, Spitzer RL, Williams JB, Benjaman LS. Structured Clinical Interview For DSM-IV Axis II Personality Disorder (SCID-II). Washington D.C.: American Psychiatric Press; 1997.
- Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther 2005;85:257- 68.
- Nunnally JC. Psychometric theory. 2nd ed. New York: McGraw-Hill; 1978.
- Shrout PE, Spitzer RL, Fleiss JL. Quantification of agreement in psychiatric diagnosis revisited. Arch Gen Psychiatry 1987;44:172-7.
- Fleiss JL. Statistical methods for rates and proportions. 2nd ed. Wiley series in probability and mathematical statistics. New York: Wiley; 1981.
- Skodol AE, Rosnick L, Kellman D, Oldham JM, Hyler SE. Validating structured DSM-III-R personality disorder assessments with longitudinal data. Am J Psychiatry 1988;145:1297-9.