East Asian Arch Psychiatry 2014;24:51-57
ORIGINAL ARTICLE
香港一所地区医院的谘询会诊服务
黄美彰、姚家聪
Dr Mimi Mei-Cheung Wong, MBBS, MRCPsych, FHKAM (Psychiatry), FHKCPsych, Department of Psychiatry, United Christian Hospital, Hong Kong SAR, China.
Dr Michael Gar-Chung Yiu, MBBS, FRCPsych, FHKAM (Psychiatry), FHKCPsych, Department of Psychiatry, United Christian Hospital, Hong Kong SAR, China.
Address for correspondence: Dr Mimi Mei-Cheung Wong, Department of
Psychiatry, United Christian Hospital, Hong Kong SAR, China. Email: wmc009@ha.org.hk
Submitted: 31 July 2013; Accepted: 7 October 2013
Abstract
Objective: To examine consultation-liaison psychiatric services in a general hospital in Hong Kong.
Methods: All records of Tseung Kwan O Hospital psychiatric consultations from 1 July 2012 to 30 June 2013 were extracted from the database. Patients’ demographic data, sources and reasons of referral, psychiatric and suicidal histories, current suicidal attempt, psychiatric diagnoses, psychiatric outcomes, as well as waiting times were analysed accordingly.
Results: A total of 1392 psychiatric consultations were received, of which 82% were attended to within the same working day when the referral was received, and 99% were attended to by the end of the next working day. The commonest reasons of consultation were unstable emotion followed by suicidal / deliberate self-harm and aggression. There were 246 consultations with actual suicidal attempt. Overall, 270 (19%) patients who received consultation-liaison psychiatric services were admitted to the psychiatric wards. Follow-up in the psychiatric outpatient department was arranged for 691 (50%) patients while 57 (4%) required referral to the community psychiatric nursing service in addition to outpatient department arrangement.
Conclusions: Management of suicidal attempters and provision of risk assessment continue to be the major tasks of consultation-liaison psychiatrists and nurses. A readily available on-site consultation- liaison psychiatric service is an essential component of services provided in acute general hospitals.
Key words: Hong Kong; Mental disorders; Referral and consultation
摘要
目的:检视香港一所综合医院的精神科谘询会诊服务。
方法:从数据库提取2012年7月1日至2013年6月30日期间於将军澳医院精神科的所有会诊记录,并分析患者的人口学统计数据、转介来源和原因、精神病和自杀史、自杀未遂途径、精神病诊断、精神病治疗成果以及会诊轮候时间。 结果:在1392例精神科会诊中,82%是於转介当天即时进行,而99%可於下个工作天前进 行。会诊最常见原因是情绪不稳、有自杀/自毁行为以及攻击行为,当中246宗属自杀未遂 个案。总体而言,270例(19%)接受精神科会诊服务的患者均须入住精神病房。691名患者(50%)接受精神科门诊随访,另57名患者(4%)须转介至精神科社康护理服务。 结论:自杀未遂者的治疗和风险评估仍是精神科医生和护士会诊时的重要工作。即场会诊精神 科服务是一所提供急症护理的综合医院必不可少的部份。
关键词:香港、精神障碍、转介和会诊
Introduction
Consultation-liaison (CL) psychiatric services operate at the interface between physical health and mental health, and address the mental needs of people who are being treated primarily for physical health problems or symptoms. The scope includes psychiatric collaboration or integration into mental health care services provided in primary care and specialty care settings.1 Consultation-liaison psychiatrists also need to be equipped with relevant legal knowledge related to health care, informed consent, and privacy. At present, liaison mental health services are mostly provided to patients attending general and acute hospitals. The prevalence of mental illness among people with physical health conditions is 2 to 3 times higher than that in the rest of the population.2 Prevalence is particularly high in the hospital setting, where around half of all inpatients suffer from a mental health condition such as depression, dementia, or delirium.2 Many of these co-morbid mental health problems typically go undiagnosed and untreated. In the absence of effective intervention, they lead to poor health outcomes, including increased rates of mortality and morbidity. Mental health co-morbidities also substantially increase the costs of physical health care.
In 2011, the Centre for Mental Health of the UK published an economic evaluation of the award-winning liaison psychiatry service at the UK’s Birmingham City Hospital. As well as improving health, the financial savings generated by the service significantly outweighed the costs of running it; annual savings were estimated to be £3.5 million.3 This was followed in 2012 by the publication of a report recommending that every National Health Service hospital in the UK should have liaison psychiatry as a standard service.2 This highlights the changing status of liaison psychiatry in public health care services. It needs to be recognised as an essential ingredient of modern health care and not an optional extra, which is merely nice to have.2
Most general hospitals in Hong Kong have different levels of CL psychiatric services which are provided by the psychiatric team within the same cluster. Some have round-the-clock coverage, especially to the Accident and Emergency Department (AED), while some have only limited services. Tseung Kwan O Hospital (TKOH) is a general hospital which provides health care services to the growing population in the Sai Kung and Tseung Kwan O districts of the New Territories of Hong Kong since 1999. It clustered with United Christian Hospital (UCH) and Haven of Hope Hospital to form the Hospital Authority Kowloon East Cluster. In 2012, it had about 400 beds. Tseung Kwan O Hospital does not have its own psychiatric unit; instead, visiting psychiatrists and psychiatric consultation-liaison nurses (CLN) from UCH provide CL psychiatric services to the AED as well as all wards of TKOH. A psychiatric nurse is stationed in the AED of TKOH whole day from Monday to Friday and provides psychiatric assessment for patients in AED under supervision of the visiting psychiatrists. One visiting psychiatrist stays in TKOH half day from Monday to Saturday, and is responsible for all inpatient psychiatric consultations as well as AED consultations, if needed. The visiting psychiatrist works under the CL team and is responsible for providing psychiatric consultation to all age-groups. In addition to on-site support, the Department of Psychiatry of UCH also provides 24-hour consultation by phone to all departments of TKOH.
All consultation referrals are initiated by the referring doctors of TKOH. The visiting psychiatrist or his / her delegate provides assistance to CLN for management of cases, whenever necessary. Cases seen by CLN are referred to the visiting psychiatrists for further assessment, if needed. There are CL rounds, once a week, for the discussion of cases seen by CLN. All cases seen by psychiatric trainees are reviewed by the Associate Consultant (AC) of the team. There is an emerging need for the extension of CL psychiatric services provided to both the AED and general wards of TKOH. In order to facilitate improved planning, it is worthwhile to review the current service demand, in particular, the nature of the referrals received. A database of the CL psychiatric service in TKOH was established on 1 July 2012. It served multiple purposes including filing and quality assurance. Establishment of a database in a liaison psychiatry service has been shown to improve clinical performance by leading to the identification of problems and introducing effective interventions.4 It contains information about patients’ demographic data, source and reason of referral, psychiatric and suicidal histories, current suicidal attempt, psychiatric diagnoses, significant medical problem, psychiatric outcome and disposal, as well as waiting time. A data input form (Appendix) is completed by the doctor or nurse. The AC of the team double check the information before entering it into electronic database, and decide the main reason for consultation if there were more than one. All consultations seen within the 1-year period were included in the database.
This study aimed to examine the CL psychiatric services to TKOH from 1 July 2012 to 30 June 2013. The data revealed the demand from the general hospital, and the types of referrals being received. Timeliness of response to referrals was also measured and compared with published standards.
Methods
All records of TKOH psychiatric consultations from 1 July 2012 to 30 June 2013 were extracted from the database and classified into departments of AED, medicine, surgery, paediatrics, orthopaedics, obstetrics and gynaecology, and intensive care unit. The patients’ demographic data, sources and reasons of referral, psychiatric and suicidal histories, current suicidal attempt, psychiatric diagnoses, significant medical problems, psychiatric outcomes and disposal, as well as waiting times were analysed accordingly. The study was approved by the Kowloon Central / Kowloon East Cluster Clinical and Research Ethics Committee.
Results
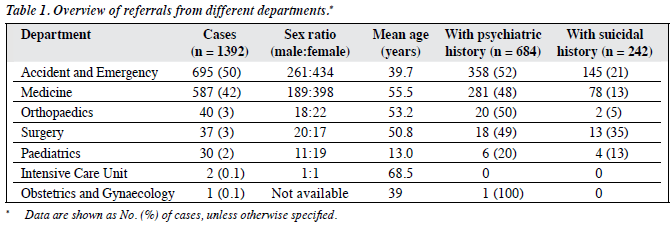
From 1 July 2012 to 30 June 2013, a total of 1392 psychiatric consultations were seen in all departments of TKOH. Overall, 791 (57%) were seen by doctors while 601 (43%) were seen by nurses. Among these consultations, 892 (64%) patients were female and 500 (36%) were male. The mean age of the patients was 47 years (range, 5-99 years). The mean age of the patients seen in the medical ward was higher than that of those seen in AED (56 vs. 40 years). Moreover, 90% of the cases were referred from AED and the medical department. Table 1 provides an overview of the referrals from different departments. Among all the cases referred, only 3 were not seen for various reasons including patient discharged against medical advice, refusal of psychiatric assessment, and patient went missing. Overall, 684 (49%) consultations had a history of mental illness and 242 (17%) reported a suicidal history.
Waiting Time
The mean waiting time for all the consultations was 0.19 working day. The maximum waiting time was 3 working days. Overall, 1144 (82%) consultations were attended to within the same working day when the referral was received, while 1376 (99%) consultations were attended to by the end of the next working day. For those with actual suicidal attempts (n = 246), 204 (83%) were attended to within the same working day while 245 (99.6%) were attended to by the end of the same working day.
Reasons of Referral
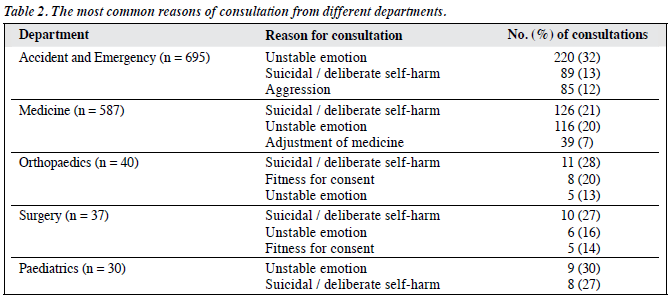
The most common reasons of consultation were unstable emotion, followed by suicidal / deliberate self-harm and aggression. There were individual variations concerning the reasons of consultation for different departments. Table 2 illustrates the few most common reasons of consultation for individual departments.
Suicidal attempts
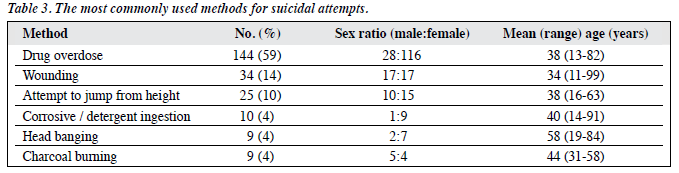
There were 246 consultations with actual suicidal attempt, including 78 males and 168 females. Methods commonly used for attempting suicide are presented in Table 3. Other methods used included attempted hanging, gas poisoning, ingestion of poison, and suffocation. Three patients used more than 1 method at a time, which included a combination of drug overdose (DO) and wrist cutting. The most frequent psychiatric diagnoses in this group of patients included adjustment disorder / reaction (n = 58) and depressive disorder (n = 57). Furthermore, 83 (34%) of those who were referred for being suicidal had a history of suicidal attempt; 196 (80%) patients attempted suicide due to relationship problems.
Diagnosis after Psychiatric Assessment
The 3 most common psychiatric diagnoses included adjustment disorder (n = 209), depressive disorder (n = 178), and schizophrenia (n = 137). For consultations referred from AED, the findings were similar, with adjustment disorder (n = 119) being the most common diagnosis followed by schizophrenia (n = 71) and depressive disorder (n = 63). The findings of consultations from the medical department were slightly different. The most common diagnosis was dementia (n = 120) followed by depressive disorder (n = 95) and adjustment disorder (n = 76). Among 1392 consultations from different departments, 347 (25%) consultations were diagnosed as organic mental disorders, including 127 cases with dementia and 61 with delirium. Besides, 131 (9%) were suffering from mental disorders due to psychoactive substance use; among these, 54 were related to alcohol use. There were 229 (16%) consultations diagnosed with functional psychosis other than mood disorders, including 137 with schizophrenia and 44 with delusional disorder. Moreover, 244 (18%) consultations were diagnosed to have mood disorders, including 178 with depressive disorder, and 46 with manic or bipolar disorder; 119 (9%) were diagnosed to have neurotic disorders. Besides, 209 (15%) consultations were diagnosed with adjustment disorder, and 117 (8%) with adjustment reaction. In addition, 51 (4%) were diagnosed to have mental retardation, 43 (3%) to have personality disorder, and 22 (2%) to have childhood emotional disorder; 64 (5%) consultations were given no psychiatric diagnosis after examination, and diagnosis was deferred for 25 (2%) cases.
Patients Admitted to General Wards due to Mental Condition
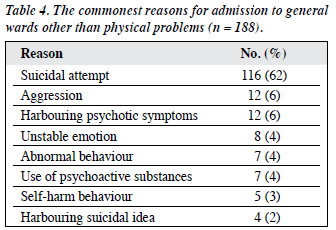
Among the consultations referred from the wards of TKOH, 188 were hospitalised due to the nature of their suspected mental condition. Among these, 116 patients were admitted because of their suicidal attempt; of these, 103 had DO, 6 had carbon monoxide poisoning, 6 had wounded themselves, and 1 had attempted hanging. The other 72 patients did not have any physical problem. Table 4 shows the commonest reasons of admission to general wards other than physical problems. Five of the patients were clinically admitted for psychiatric consultation.
Outcome of Referrals
Overall, 270 (19%) patients were admitted to the psychiatric wards. Among these, 66 (24%) were referred for being suicidal or for engaging in an actual act of self-harm, 62 (23%) were referred for having unstable emotion, while 42 (16%) were referred for being aggressive. Inpatient treatment was offered to 5 patients but both the patients and family members refused the arrangement. They were discharged against medical advice. Follow-up in the psychiatric outpatient department (OPD) was arranged for 691 (50%) patients, while 57 (4%) required referral to community psychiatric nursing service in addition to OPD arrangement. A minority (8%) were referred to private psychiatrists, social services, clinical psychologists, or general practitioners. Overall, 168 (12%) patients did not require follow-up, and 96 (7%) consultations required reassessment. A majority of those who had a suicidal history (n = 230; 95%) and majority of those who were referred for being suicidal (n = 208; 85%) were given psychiatric care either in the inpatient or outpatient setting.
Discussion
Reasons of Referral
The most common reason of referral from all departments of TKOH was risk assessment which included the assessment of suicidal and violent risk. This aligns with data from other studies5,6 which also found that risk assessment was the most important task of CL psychiatrists. Patients were admitted to the ward after a suicidal attempt or noted by the referring team to have unstable emotion with suicidal idea or aggressive behaviour. In TKOH, the majority of the DO cases were admitted to the medical ward. In other general hospitals, these cases were usually managed in the emergency medical ward (EMW) under the AED. Therefore, the reasons of referral from the medical department were different from those from another study on CL psychiatric services in a general hospital, in which the commonest reason for referral was assessment for depressive disorders, confusion, alcohol-related disorders, and anxiety disorders.7 Assessment of somatic complaints was seldom encountered among referrals from the wards. A small proportion of referrals from the surgical teams was for assessment of mental fitness for consent to surgery. Nearly half of the patients who were referred had a psychiatric history; this suggests that referring doctors should involve psychiatrists in the management of their patients who have a positive psychiatric history.8 This group of patients might also have psychiatric presentations or relapse of their mental illness when they had co-morbid physical conditions requiring input from psychiatrists.
Suicidal Attempt and Assessment
Among patients who had attempted suicide, females outnumbered the males by about 2 times. Drug overdose was the commonest method for attempted suicide. More females attempted suicide by DO and ingestion of corrosive agent / detergent than males. Over half of these patients were given a diagnosis of depressive disorder. Although investigating the exact reason for their suicide was not the objective of this study, it was noted that most of the female patients wanted to end their life because of relationship problems, particularly marital problems. Culturally, marriage is highly valued by Chinese women. Despite developing a strong career, many women in Hong Kong devote a significant proportion of their time for taking care of their family members.9 Thus, marital breakdown is a cause for significant distress which can trigger a depressive episode.10-12 In the CL psychiatric setting, in addition to providing a proper risk assessment and formulation of a management plan, the psychiatrist or CLN commonly has to perform the role of a marriage counsellor. Further collaboration with providers of social services would be necessary and helpful in the management of this group of patients.
Role of Consultation-liaison Nurses
In Hong Kong, CLNs have an increasing role in providing CL psychiatric services in general hospitals. This trend is similar to that in other countries.13,14 For example, in the current UK practice, most psychosocial assessments are carried out by mental health nurses and junior psychiatrists.15,16 It was found that the positive predictive value of risk assessments for self-harm repetition was 25% among nurses and 23% among junior psychiatrists.16 This finding supports the use of nurse-led assessment services. Consultation-liaison nurses are arranged to assess cases in AEDs in the Kowloon East Cluster where they encounter a large number of cases with deliberate self-harm. Consultation-liaison nurses are advised to discuss the management of their patients with suicidal attempts with the visiting psychiatrists before disposing the patients; there is weekly supervision of the team by an AC. All these measures ensure provision of high-quality psychiatric services to the patients of TKOH.
Dementia and Delirium
Among all the referrals, only 61 were diagnosed to have delirium, and the finding was similar to that from an earlier study about CL psychiatric services.5 This study only reflected the pattern of referral occurring in the year rather than the genuine number of cases with delirium. Some doctors in the medical department may have already managed patients with delirium themselves, without consulting the CL psychiatric team. Management interventions for delirium by the liaison psychiatry team comprises giving advice to nursing staff on orientation techniques, advice to medical teams on appropriate medical investigations for delirium, and alteration of medications if needed. In some countries, guidelines have been developed which outline a number of management principles for delirium. These guidelines indicate that the most important action for management of delirium is identification and treatment of the underlying cause.7
Timeliness of Response to Referrals
Timeliness of response in this study matches the standards set out by a CL psychiatric service in the UK where 90% of all referrals are seen by the end of the next working day. However, for referrals following self-harm, the standard requires that 90% of all referrals be seen by the end of the same day.7,17 In TKOH, 83% of referrals following self-harm were attended to within the same working day and 99.6% were seen by the end of the next working day. Although it did not match the standard set out by O’Keeffe et al,17 our performance was better than other CL psychiatric teams where about 59% of patients referred following deliberate self-harm were seen within the same day.7,17 It would be meaningful to compare our performance with that of other CL psychiatric teams in local hospitals; however, such data are lacking. An important reason that patients with self- harm could not be assessed on the same day was because the visiting psychiatrist only stayed in TKOH for half day. Sometimes, the psychiatrist only came for the morning session, and referrals received in the afternoon had to be attended to on the next working day.
Admission of Patients with Purely Psychiatric Problems to General Wards
As there was no emergency observation ward under the AED of TKOH, a number of patients with psychiatric problems only were admitted to the general wards of TKOH. In most local hospitals, CL psychiatric services are generally not available for general wards during weekends and public holidays, except for very urgent cases. However, such coverage is available for EMW in most centres. Patients with psychiatric problems or suicidal attempts presenting to AED would be arranged to stay in EMW, if needed, for organic workup. If such patients could be arranged to stay in EMW of TKOH instead of being admitted to the general wards, there could be enhancement of CL psychiatric services with focus in support to EMW along with reduction of the admission rates to medical wards and the length of stay of these patients. Improved CL psychiatric services was found to reduce inappropriately delayed discharge and improve outcomes for patients with psychiatric morbidities.10 Some of the patients who were already admitted to the hospital showed reluctance to get transferred to the psychiatric ward, even if needed, as they were already settled in the general ward and believed their mental condition could be well managed there.
Use of Clinical Inbox and Electronic Records
This study found a very low rate of discharge of patients before assessment by the CL. It was likely related to the efficiency of the team and the use of electronic referral system. Referrals from AED are received by phone calls while referrals for inpatient psychiatric consultation were received from the clinical inbox of the Clinical Management System (CMS). The clinical inbox has the advantage of keeping an electronic record of all the consultations and being linked directly to the electronic patient record. There are pop-up notifications of unread referrals when the AC in-charge of TKOH CL service logs into the CMS of TKOH. These systems help to ensure that referrals reach the psychiatrists as soon as possible, reduce the waiting time, and minimise the rate of discharge against medical advice before psychiatric assessment.5
Case notes of CLN and visiting psychiatrist are entered into the CMS and this facilitates the exchange of useful clinical information with other psychiatrists or doctors from other departments who provide clinical care to the patients.
Conclusions
Management of suicidal attempters and provision of risk assessment continue to be the major tasks of CL psychiatrists and CLNs. There is a definite need to enhance CL psychiatric services by increasing the number of CLNs with support from CL psychiatrists, especially in view of the increasing number of inpatient beds and prospective opening of EMW in TKOH.
Declaration
There is no financial support and no conflict of interest.
Acknowledgment
We would like to acknowledge the help from consultation- liaison nurses and doctors of Department of Psychiatry, United Christian Hospital who assisted in the data collection process of the study.
References
- Leentjens AF, Rundell JR, Diefenbacher A, Kathol R, Guthrie E. Psychosomatic medicine and consultation-liaison psychiatry: scope of practice, processes, and competencies for psychiatrists working in the field of CL psychiatry or psychosomatics. A consensus statement of the European Association of Consultation-Liaison Psychiatry and Psychosomatics (EACLPP) and the Academy of Psychosomatic Medicine (APM). Psychosomatics 2011;52:19-25.
- Parsonage M, Fossey M, Tutty C. Liaison psychiatry in the modern NHS. London: Centre for Mental Health; 2012.
- Parsonage M, Fossey M. Economic evaluation of a liaison psychiatry service. London: Centre for Mental Health; 2011.
- Holmes AC, Judd FK, Lloyd JH, Dakis J, Crampin EF, Katsenos S. The development of clinical indicators for a consultation-liaison service. Aust N Z J Psychiatry 2000;34:496-503.
- Ku KH, Nguyen GH, Ng YK. Consultation-liaison psychiatry in Kwai Chung Hospital. Hong Kong J Psychiatry 1997;7:3-8.
- Lilley R, Owens D, Horrocks J, House A, Noble R, Bergen H, et al. Hospital care and repetition following self-harm: multicentre comparison of self-poisoning and self-injury. Br J Psychiatry 2008;192:440-5.
- Lyne J, Hill M, Burke P, Ryan M. Audit of an inpatient liaison psychiatry consultation service. Int J Health Care Qual Assur 2009;22:278-88.
- Kapur N, Murphy E, Cooper J, Bergen H, Hawton K, Simkin S, et al. Psychosocial assessment following self-harm: results from the multi- centre monitoring of self-harm project. J Affect Disord 2008;106:285- 93.
- Tao J, Zheng B, Mow SL. Holding up half the sky: Chinese women past, present and future. New York: Feminist Press at the City University of New York; 2004.
- Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, et al. Stressful life events, genetic liability, and onset of an episode of major depression in women. Am J Psychiatry 1995;152:833-42.
- 1 Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. Am J Psychiatry 2002;159:1133-45.
- Herman SJ. Women, divorce, and suicide. J Divorce 1978;1:107-17.
- Griffin G, Bisson JI. Introducing a nurse-led deliberate self-harm assessment service. Psychiatrist 2001;25:212-4.
- Roberts D. Liaison mental health nursing: origins, definition and prospects. J Adv Nurs 1997;25:101-8.
- McAllister M. Assessment following self-harm: nurses provide comparable risk assessment to psychiatrists but are less likely to admit for in-hospital treatment. Evid Based Nurs 2011;14:83-4.
- Murphy E, Kapur N, Webb R, Cooper J. Risk assessment following self-harm: comparison of mental health nurses and psychiatrists. J Adv Nurs 2011;67:127-39.
- O’Keeffe N, Ramaiah U, Normani E, Fitzpatrick M, Ranjith G. Benchmarking a liaison psychiatry service: a prospective 6-month study of quality indicators. Psychiatrist 2007;31:345-7.