East Asian Arch Psychiatry 2014;24:58-67
ORIGINAL ARTICLE
Dr Sandeep Grover, MD, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Dr Naresh Nebhinani, MD, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Dr Subho Chakrabarti, MD, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Dr Ruchita Shah, MD, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Dr Ajit Avasthi, MD, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Address for correspondence: Dr Sandeep Grover, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Tel: (91-172) 2756 807; Fax: (91-172) 2744 401; Email: drsandeepg2002@yahoo.com
Submitted: 25 March 2014; Accepted: 25 April 2014
Abstract
Objective: To explore the relationship between attribution of symptoms to supernatural beliefs and first treatment contact in caregivers of patients with schizophrenia attending a tertiary care hospital located in North India.
Methods: A total of 122 caregivers (aged ≥ 18 years, staying with patient ≥ 1 year and involved in patients’ care) of consecutive patients with diagnosis of schizophrenia (according to the ICD-10) were evaluated for their supernatural beliefs and first treatment contact.
Results: The first treatment contact was a government or private psychiatrist in slightly more than half (53.3%) of the patients, while it was faith healers in 23.8% of the patients. Around three quarters (74.6%) of the caregivers attributed patients’ symptoms to ≥ 1 supernatural belief (like sorcery / witchcraft, ghosts, spirit intrusion, divine wrath, planetary influences, evil spirits, and bad deeds in previous life) and more than half (57.4%) of the caregivers attributed patients’ symptoms to > 1 supernatural belief. It was observed that those who contacted faith healers for their patients’ treatment had significantly higher attribution of the symptoms to supernatural causes.
Conclusions: Supernatural beliefs were common in caregivers of patients with schizophrenia and the majority attributed their patients’ symptoms to these beliefs. It signifies an urgent need for mental health literacy in India.
Key words: Caregivers; Mental health services; Schizophrenia; Spirituality
摘要
目的:检视印度北部一所提供第叁层医疗服务医院内精神分裂症病人照顾者其首个治疗接触点与超自然信念的关係。
方法:研究共纳入连续122名根据ICD-10诊断为精神分裂症病人的照顾者(18岁或以上并直接参与病人护理至少1年),分析其超自然信念和首个治疗接触点。
结果:超过一半(53.3%)的首个治疗接触点为政府或私人精神科医生,而信念疗法则占 23.8%。约四分之叁照顾者(74.6%)认为患者出现症状由至少一种超自然信念造成(如妖术/巫术、魔鬼、灵体入侵、激怒神灵、行星影响、邪灵和前世恶行),而超过一半照顾者(57.4%)相信患者的症状由多於一种超自然信念造成。此外,与信念治疗师联繫的病人照顾者较相信病人患病由超自然原因造成。
结论:超自然信念常见於精神分裂症病人照顾者,且大部分均认为患者病症与这些信念相关。这显示印度精神健康教育的迫切需要。
关键词:照顾者、精神健康服务、精神分裂症、灵性
Introduction
Schizophrenia imposes a significant burden on the individual, family, and community due to its chronic course, associated disability, social dysfunction, along with poor adherence with treatment, and need for frequent hospitalisation.1 Functional recovery in patients with schizophrenia is influenced by several factors such as pre-morbid functioning, symptom profile, and duration of illness (including duration of untreated psychosis).2 Delay in institution of appropriate treatment is closely linked with the community’s awareness about causes and available treatment modalities, which further directs their help- seeking behaviour and pathways.
Explanatory models refer to patients’ and their families’ causal attributions of illness3 and have been shown to affect their coping,4,5 treatment preferences,5 compliance, and outcome.6 Thus, investigating family members’ causal beliefs regarding schizophrenia is an important step in the management of the illness as it further influences the help- seeking pathway of individuals with schizophrenia.7
Pathways of psychiatric care have been defined as the sequence of contacts with individuals and organisations, initiated by the patients or families in their effort to seek appropriate help.8 Such studies provide vital information regarding the individual’s help-seeking and illness behaviour, and possible sources of delay in presenting to appropriate treatment facilities. Knowledge about these parameters, subsequently, helps in organising mental health services, coordinating psychiatric referrals, and enhancing the treatment-seeking attitude.9
Few studies have evaluated the aetiological models (mostly, by using semi-structured interviews) including supernatural beliefs held by patients with schizophrenia and their caregivers from developed3,10-14 and developing countries including India.5,7,15-27 Non-biomedical causal models of schizophrenia including magico-religious causes were more commonly reported from developing countries.5,18,25
Few studies have also evaluated pathways to care in patients with psychiatric disorders, and most of these are from developed countries28-31; few are from developing countries like China32 and Nigeria.33 The Indian literature on help-seeking patterns in psychiatric populations is mainly about common mental disorders,34-40 with only few studies on schizophrenia.26,27
Although studies have evaluated the aetiological models and pathways to care, none of the studies has evaluated the relationship of supernatural beliefs with pathways to care and initial help-seeking behaviour. In India, family provides supports to patients with psychosis, and when a patient is ill, the help-seeking behaviour is more or less determined by the caregivers. In view of this, the present study aimed to evaluate the relationship between the magico-religious beliefs held by the primary caregivers of patients with schizophrenia and first treatment contact pathways to care.
Methods
Study Setting and Sample Selection
The study was carried out at the outpatient clinic of the psychiatry department in a multi-specialty tertiary care hospital in North India. Consecutive newly registered patients diagnosed with schizophrenia by a qualified psychiatrist were approached. To be included in the study, the patients were required to be aged ≥ 15 years and fulfil the diagnosis of schizophrenia as per the ICD-10.41 Those with co-morbid mental retardation and organic brain syndromes were excluded. Informed consent was sought from all patients and their caregivers. In case a patient was incompetent, consent was obtained from the primary caregiver.
Family members accompanying the patients were included in the study if they were living with the patients and were involved in their care for ≥ 1 year. When more than one family member was available, the caregiver staying with the patient for most part of the day and more involved in the care of the patient and decision-making about treatment was selected. To be included in the study, caregivers were required to be aged ≥ 18 years.
The study was approved by the Ethics Review Committee of the Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Instruments
Supernatural Attitude Questionnaire (Caregiver Version)
The questionnaire consists of 28 items worded in simple language with ‘yes’ and ‘no’ responses designed to study the various types of magico-religious beliefs held by an individual, the role of magico-religious beliefs in causation of mental illness / behavioural abnormalities, and the role of treatment based on such beliefs. Various items of the questionnaire are based on commonly prevalent magico- religious beliefs in our society.25 This questionnaire has been used in earlier studies from our centre.25
Assessment on Pathways to Care
Pathways to care were assessed by a self-designed questionnaire. By using a semi-structured interview, patients and their caregivers were asked about their help- seeking behaviour for symptoms of schizophrenia. The sequence of contact with different agencies was prepared. This questionnaire had been used in an earlier study.26
Statistical Analysis
Analysis was done using the Statistical Package for the Social Sciences Windows version 14.0 (SPSS, Chicago [IL], US). Frequencies with percentages were calculated for nominal and ordinal variables, and means and standard deviations (SDs) were calculated for continuous variables. Chi-square test, t test, and one-way analysis of variance were used for comparisons. Correlation analysis was employed to study the association between different variables by using Pearson product-moment correlations and Spearman’s rank correlation.
Results
Socio-demographics and Clinical Profiles
The study included 122 patients with schizophrenia contacting the psychiatric services of our institute for the first time. The mean (± SD) patient age was 30.6 ± 12.6 years and they received education with a mean of 8.9 ± 4.7 years. Nearly half of the patients were males (50.8%), single (54.9%), and from a rural background (54.9%). The majority of patients was Hindu (77.0%).
As stated in Table 1, the most common subtype of schizophrenia was undifferentiated (61.5%) followed by paranoid (34.4%), with a median duration of illness of 36 months. One-fourth (23.8%) of patients had co-morbid substance abuse / dependence and slightly more than a quarter (28.7%) had physical co-morbidities. Nearly two-thirds of the patients were receiving antipsychotic medications. Other details are depicted in Table 1.
Pathways to Care
Prior to contacting our treating agency, the patients had a mean of 2.04 ± 1.07 treatment contacts. As shown in Table 1, over half of the patients (n = 65; 53.3%) were first taken to a psychiatrist for their symptoms. One-sixth (n = 22; 18.0%) of the patients were first taken to a physician (including the registered medical practitioners), whereas nearly one-fourth (n = 29; 23.8%) were first taken to faith healers and other traditional healers for their symptoms.
Agency of First Contact
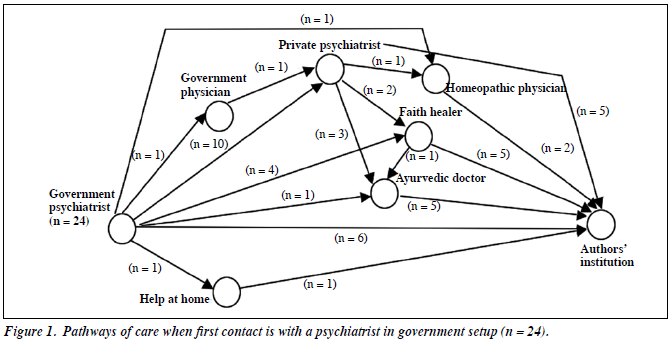
In our study, 24 patients had first contact with psychiatrists in a government hospital. Of these 24 patients, 6 had second contact with our institution. Eleven patients had 1 contact with other helping agencies (4 patients contacted private psychiatrists, 3 patients contacted a faith healer, 1 patient contacted an ayurvedic physician, 1 patient contacted a homeopathic physician, and 1 was helped at home) before reaching our centre. Seven patients had 3 contacts before reaching our centre. The pathways for these patients are shown in Figure 1.
In our study, 31 patients had first contact with a psychiatrist in the private setup. Of them, 9 contacted our institution as the second place of consultation. Fifteen patients had contact with 1 helping agency and 7 patients had contact with 2 helping agencies before reaching our centre. The pathways for these patients are shown in Figure 2.
In our study, 29 patients had first contact with faith healers. Of these, 5 patients contacted our institution as the second contact; 20 had contact with 1 helping agency (5 to private psychiatrist, 1 to a government psychiatrist, 4 to an ayurvedic physician, 3 to a government physician, 3 to a private physician, 1 to a homeopathic physician, 2 to registered medical practitioners [RMP], and 1 was helped at home); the remaining 4 patients contacted with 2 helping agencies before reaching our centre.
Caregivers’ Supernatural Beliefs
Of the 122 caregivers, 46 (37.7%) had supernatural beliefs. In all, 31 (25.4%) believed in sorcery / witchcraft (jaadu tona), 29 (23.8%) believed in ghosts / evil spirits (bhoot pret), and 40 (32.8%) believed in spirit intrusion (opari kasar). Overall, 32 (34.4%) caregivers had > 1 supernatural belief. Further details are provided in Table 2.
On exploring about the patients’ supernatural beliefs, 54 (44.3%) caregivers reported that their patients had ≥ 1 supernatural belief. Of them, 36 (29.5%) had ≥ 2 supernatural beliefs about mental illness and 9 (7.4%) had all the 6 supernatural beliefs.
In all, 64 (52.5%) caregivers of patients with schizophrenia stated that community also held magico- religious beliefs regarding causation and treatment of mental illness. When asked about their belief in supernatural causation of mental illness in general, 91 (74.6%) caregivers stated they had belief in any one supernatural cause. Other details are shown in Table 2. In all, 38 (31.1%) caregivers felt that offering prayers (puja, rituals, jhad-phook) could change patients’ behaviour and 49 (40.2%) agreed that their families had actually arranged such rituals for the betterment of their patients. Also, 56 (45.9%) caregivers had also visited faith healers for their patients’ illness (Table 2).
Association of Socio-demographic and Clinical Variables with Supernatural Beliefs and First Treatment Contact
Based on the first treatment contact, the study group was divided into 3 groups: (1) those who chose to seek treatment from a psychiatrist as first contact (i.e. those who first contacted a psychiatrist in a government hospital, private clinic, or those who came directly to our psychiatry outpatient clinic); (2) those who first sought treatment from a physician (from the government / private sector); and (3) those who first contacted faith healers and other traditional healers.
The socio-demographic and clinical variables did not differ significantly between the 3 groups. However, those seeking treatment from faith healers were more commonly from the urban locality compared with those contacting physicians as the first treatment contact (51.7% vs. 22.7%, χ2 = 4.41, p = 0.03). Details are depicted in Table 3.
When compared with the groups of seeking psychiatrists and physicians as first treatment contact, a higher proportion of caregivers who first took their patients to faith healers believed in spirit intrusion (p = 0.04) and ghosts (p = 0.02), had ≥ 1 supernatural belief (p = 0.05), had > 1 supernatural belief (p = 0.01), attributed mental illnesses of their patients to sorcery / witchcraft (p = 0.02) , ghosts (p = 0.01), spirit intrusion (p = 0.002), evil spirits (p = 0.002), and considered mental illnesses to be caused by bad deeds in previous life (p = 0.04).
Relationship between First Treatment Contact and Total Number of Contacts before Contacting the Tertiary Care Centre
Those who had first contact with a psychiatrist had a mean of 1.83 ± 1.15 treatment contacts before contacting us; respective value for a physician was 2.27 ± 0.98 treatment contacts and for a faith healer it was 2.41 ± 0.9 treatment contacts. The difference between the 3 groups was statistically significant (F = –3.53, p = 0.03).
Discussion
Family is the key resource in the care of mentally ill in India.42 The causal attribution by families of patients of schizophrenia is strongly influenced by multiple sociocultural factors, which also modulate their health perceptions, illness presentations, and interaction between the patients and health providers.18,43 It also directs the pathways of care, sometimes delays professional medical treatment, and also alters the outcome of this illness.44
Although public health implications of chronic physical disorders are widely accepted, knowledge about mental disorders (mental health literacy) remains broadly neglected.44 Thorough understanding of the layman’s understanding about psychiatric disorders and help-seeking pathways is of great importance for planning locally relevant and sustainable mental health services.31 Therefore, this study aimed to evaluate caregivers’ magico-religious beliefs, role of magico-religious beliefs in causation of symptoms from the carers’ perspectives, and help-seeking behaviour of patients with schizophrenia.
Slightly more than half (53.3%) of the patients had psychiatrists (government setup / private setup) and 23.8% of the patients had faith healers as their first treatment contact. Few patients (18.0%) first contacted a physician for their psychotic symptoms. Similar to earlier studies34,36 which have evaluated patients with other psychiatric disorders from India, psychiatrists were most commonly contacted at first level in our study. However, our findings are in contrast with a study from India27 which evaluated caregivers of schizophrenia and reported faith healers as the commonest first contact. When we compare our findings with studies from other countries, certain important differences emerge. A recently published population-based survey of patients with first-episode psychosis from United Kingdom45 showed that the primary care physicians were the most common first contacts in about one-third (35.2%) of the cases, followed by criminal justice agencies (25.4%) and emergency rooms of general hospitals (21.3%), whereas a recent study from Nigeria46 showed that more than two-thirds (69%) of the subjects with psychosis seek their first help from traditional and religious healers. These differences reflect the sociocultural differences in the conceptualisation of illness and organisation of health care services in different countries.
The study from Nigeria46 also noted that patients who first contacted non-orthodox healers, ultimately, had higher number of treatment contacts during the course of the help-seeking compared with those who had first contact with mental health services. This finding is also validated by our study which showed that those who first contacted a faith healer had significantly more treatment contacts prior to reaching our treatment agency when compared with psychiatrists as first contact. This finding suggests that there is a need to improve collaboration between mental health care facilities and traditional faith healers. Efforts should be made to educate faith healers about the symptoms of mental illnesses, so that these patients can be referred to appropriate treating agencies at the earliest to reduce the duration of untreated psychosis.
In our study, around three-quarters (74.6%) of the caregivers attributed their patients’ symptoms to ≥ 1 supernatural belief (sorcery / witchcraft, ghosts, spirit intrusion, divine wrath, planetary influences, evil spirits, and bad deeds in previous life) and more than half (57.4%) of the caregivers attributed patients’ symptoms to > 1 supernatural belief. Our findings in the caregiver population are more or less similar to those in earlier reports on caregivers25 and patients with schizophrenia,26 pointing towards a stable pattern of predominance of supernatural beliefs in caregivers and patients with schizophrenia in the Indian setting. This suggests that there is a need for awareness campaigns at the community level to address this issue.
Similar to earlier studies from India5,25,27 and other countries,17,18,20-22,32,47,48 we also found high prevalence (74.6%) of belief in supernatural aetiology of mental illness. Few studies7,14,23 have reported higher prevalence of belief in psychosocial and biological aetiologies than supernatural aetiology of mental illness.
Aetiological beliefs also influence the societal response towards the mentally ill and, sometimes, generate stigmatising attitudes.49 It further contributes to delay in treatment50 which results in greater functional disability and poorer outcome.51 An earlier study32 found an association between first psychiatric contact and chronic onset of illness, a mixed syndrome of positive and negative symptoms, and better economic status. Another study18 reported that patients who believe in supernatural causation of schizophrenia were more likely to have family members with schizophrenia who had never received psychiatric medical treatment. We could not find any such associations in our study.
Our findings suggest that first treatment contact is influenced by poor knowledge and awareness about psychiatric illness causation as well as treatment modalities, and high prevalence of supernatural beliefs in causation of mental illness. It signifies the urgent need for mental health literacy in India. Fostering effective mental health care requires a thorough understanding of patients’ and caregivers’ perspectives as well as improved literacy about psychosis in the community and other treatment agencies. Therefore, there is a need for sensitisation programmes for physicians, complementary alternative therapists, and faith healers about the need of early identification, timely referral, and proper management of common mental disorders. These measures might reduce the delays in treatment and cost of treatment.36
The study has several limitations. It was a hospital- based sample from an outpatient clinic, and the help- seeking processes and beliefs may be different in patients attending other psychiatric services and in community populations. Recall bias might have affected the help- seeking information provided by caregivers. A self-rated instrument was used to evaluate the supernatural beliefs and aetiological models. Hence, findings should be interpreted with caution. We included a heterogeneous group of patients with schizophrenia in various stages of illness. This could have affected the attribution of illness, and the results must be interpreted against this background. We also did not evaluate the duration of untreated psychosis and its relationship with first treatment contact and supernatural beliefs.
To conclude, the present study demonstrates that supernatural beliefs are quite common in the north Indian community, and the majority of caregivers attribute their patients’ symptoms to ≥ 1 supernatural cause. A significant proportion of patients had belief in magico- religious causation of mental illness and also sought such treatment in different settings. To improve patients’ and caregivers’ understanding about causation and treatment of psychiatric disorder, integrated efforts for raising public awareness and gatekeeper education are required. Future large-scale studies across various regions of India may help in determining societal aetiological models, beliefs in supernatural causation, and pathways of care.
Declaration
The authors declared no conflict of interest in this study.
References
- Salloum IM, Moss HB, Daley DC. Substance abuse and schizophrenia: impediments to optimal care. Am J Drug Alcohol Abuse 1991;17:321- 36.
- Siegel SJ, Irani F, Brensinger CM, Kohler CG, Bilker WB, Ragland JD, et al. Prognostic variables at intake and long-term level of function in schizophrenia. Am J Psychiatry 2006;163:433-41.
- Ghane S, Kolk AM, Emmelkamp PM. Assessment of explanatory models of mental illness: effects of patient and interviewer characteristics. Soc Psychiat Epidemiol 2010;45:175-82.
- Rose LE. Understanding mental illness: the experience of families of psychiatric patients. J Adv Nurs 1983;8:507-11.
- Saravanan B, Jacob KS, Jhonson S, Prince M, Bhugra D, David AS. Belief models in first episode schizophrenia in South India. Soc Psychiatry Psychiatr Epidemiol 2007;42:446-51.
- Foulks EF, Persons JB, Merkel RL. The effect of patients’ beliefs about their illnesses on compliance in psychotherapy. Am J Psychiatry 1986;143:340-4.
- Phillips MR, Li Y, Stroup TS, Xin L. Causes of schizophrenia reported by patients’ family members in China. Br J Psychiatry 2000;177:20-5.
- Rogler LH, Cortes DE. Help-seeking pathways: a unifying concept in mental health care. Am J Psychiatry 1993;150:554-61.
- Trivedi JK, Jilani AQ. Pathway of psychiatric care. Indian J Psychiatry 2011;53:97-8.
- Esterberg ML, Compton MT. Causes of schizophrenia reported by family members of urban African American hospitalized patients with schizophrenia. Compr Psychiatry 2006;47:221-6.
- 1 Angermeyer MC, Matschinger H. Lay beliefs about schizophrenic disorder: the results of a population survey in Germany. Acta Psychiatr Scand Suppl 1994;382:39-45.
- Magliano L, De Rosa C, Fiorillo A, Malangone C, Maj M, National Mental Health Project Working Group. Perception of patients’ unpredictability and beliefs on the causes and consequences of schizophrenia — a community survey. Soc Psychiatry Psychiatr Epidemiol 2004;39:410-6.
- McCabe R, Priebe S. Explanatory models of illness in schizophrenia: comparison of four ethnic groups. Br J Psychiatry 2004;185:25-30.
- Holzinger A, Kilian R, Lindenbach I, Petscheleit A, Angermeyer MC. Patients’ and their relatives’ causal explanations of schizophrenia. Soc Psychiatry Psychiatr Epidemiol 2003;38:155-62.
- Bouhlel S, Ben Haouala S, Klibi A, Ghaouar M, Chennoufi L, Melki W, et al. Assessing beliefs and attitudes of relatives of patients with schizophrenia: a study in a Tunisian sample [in French]. Encephale 2013;39:165-73.
- Shibre T, Negash A, Kullgren G, Kebede D, Alem A, Fekadu A, et al. Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Soc Psychiatry Psychiatr Epidemiol 2001;36:299-303.
- Zafar SN, Syed R, Tehseen S, Gowani SA, Waqar S, Zubair A, et al. Perceptions about the cause of schizophrenia and the subsequent help seeking behavior in a Pakistani population — results of a cross- sectional survey. BMC Psychiatry 2008;8:56.
- Kurihara T, Kato M, Reverger R, Tirta IG. Beliefs about causes of schizophrenia among family members: a community-based survey in Bali. Psychiatric Serv 2006;57:1795-9.
- Sorsdahl KR, Flisher AJ, Wilson Z, Stein DJ. Explanatory models of mental disorders and treatment practices among traditional healers in Mpumulanga, South Africa. Afr J Psychiatry (Johannesbg) 2010;13:284-90.
- Adewuya AO, Makanjuola RO. Lay beliefs regarding causes of mental illness in Nigeria: pattern and correlates. Soc Psychiatry Psychiatr Epidemiol 2008;43:336-41.
- Razali SM, Khan U, Hasanah CI. Belief in supernatural causes of mental illness male patients: impact on treatment. Acta Psychiatr Scand 1996;94:229-33.
- Kua EH, Chew PH, Ko SM. Spirit possession and healing among Chinese psychiatric patients. Acta Psychiatr Scand 1993;88:447-50.
- Srinivasan TN, Thara R. Beliefs about causation of schizophrenia: do Indian families believe in supernatural causes? Soc Psychiatry Psychiatr Epidemiol 2001;36:134-40.
- Saravanan B, Jacob KS, Deepak MG, Prince M, David AS, Bhugra D. Perceptions about psychosis and psychiatric services: a qualitative study from Vellore, India. Soc Psychiatry Psychiatr Epidemiol 2008;43:231-8.
- Kulhara P, Avasthi A, Sharma A. Magico-religious beliefs in schizophrenia: a study from North India. Psychopathology 2000;33:62- 8.
- Kate N, Grover S, Kulhara P, Nehra R. Supernatural beliefs, aetiological models and help seeking behaviour in patients with schizophrenia. Ind Psychiatry J 2012;21:49-54.
- Naik SK, Pattanayak S, Gupta CS, Pattanayak RD. Help-seeking behaviors among caregivers of schizophrenia and other psychotic patients: a hospital-based study in two geographically and culturally distinct Indian cities. Indian J Psych Med 2012;4:338-45.
- Skeate A, Jackson C, Birchwood M, Jones C. Duration of untreated psychosis and pathways to care in first-episode psychosis. Investigation of help-seeking behaviour in primary care. Br J Psychiatry Suppl 2002;43:s73-7.
- Wrigley S, Jackson H, Judd F, Komiti A. Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Aust N Z J Psychiatry 2005;39:514-21.
- Köhn D, Pukrop R, Niedersteberg A, Schultze-Lutter F, Ruhrmann S, Bechdolf A, et al. Pathways to care: help-seeking behavior in first-episode psychosis [in German]. Fortschr Neurol Psychiatr 2004;72:635-42.
- Fujisawa D, Hashimoto N, Masamune-Koizumi Y, Otsuka K, Tateno M, Okugawa G, et al. Pathway to psychiatric care in Japan: a multicenter observational study. Int J Ment Health Syst 2008;2:14.
- Tang YL, Sevigny R, Mao PX, Jiang F, Cai Z. Help-seeking behaviors of Chinese patients with schizophrenia admitted to a psychiatric hospital. Adm Policy Ment Health 2007;34:101-7.
- Gureje O, Acha RA, Odejide OA. Pathways to psychiatric care in Ibadan, Nigeria. Trop Geogr Med 1995;47:125-9.
- Chadda RK, Agarwal V, Singh MC, Raheja D. Help seeking behaviour of psychiatric patients before seeking care at a mental hospital. Int J Soc Psychiatry 2001;47:71-8.
- Pradhan SC, Singh MM, Singh RA, Das J, Ram D, Patil B, et al. First care givers of mentally ill patients: a multicenter study. Indian J Med Sci 2001;55:203-8.
- Mishra N, Nagpal SS, Chadda RK, Sood M. Help-seeking behavior of patients with mental health problems visiting a tertiary care center in north India. Indian J Psychiatry 2011;53:234-8.
- Lahariya C, Singhal S, Gupta S, Mishra A. Pathway of care among psychiatric patients attending a mental health institution in central India. Indian J Psychiatry 2010;52:333-8.
- Kishore J, Gupta A, Jiloha RC, Bantman P. Myths, beliefs and perceptions about mental disorders and health-seeking behavior in Delhi, India. Indian J Psychiatry 2011;53:324-9.
- Jain N, Gautam S, Jain S, Gupta ID, Batra L, Sharma R, et al. Pathway to psychiatric care in a tertiary mental health facility in Jaipur, India. Asian J Psychiatr 2012;5:303-8.
- Faizan S, Raveesh BN, Ravindra LS, Sharath K. Pathways to psychiatric care in South India and their socio-demographic and attitudinal correlates. BMC Proc 2012;6(Suppl 4):P13.
- WHO. The ICD-10 classification of mental and behavioural disorders — clinical descriptions and diagnostic guidelines. Geneva: WHO; 1992.
- Avasthi A. Preserve and strengthen family to promote mental health. Indian J Psychiatry 2012;52:113-26.
- Patel V, Musara T, Butau T, Maramba P, Fuyane S. Concepts of mental illness and medical pluralism in Harare. Psychol Med 1995;25:485-93.
- Jorm AF. Mental health literacy. Public knowledge and beliefs about mental disorders. Br J Psychiatry 2000;177:396-401.
- Bhui K, Ullrich S, Coid JW. Which pathways to psychiatric care lead to earlier treatment and a shorter duration of first-episode psychosis? BMC Psychiatry 2014;14:72.
- Adeosun II, Adegbohun AA, Adewumi TA, Jeje OO. The pathways to the first contact with mental health services among patients with schizophrenia in Lagos, Nigeria. Schizophr Res Treatment 2013;2013:769161.
- Aghukwa CN. Care seeking and beliefs about the cause of mental illness among Nigerian psychiatric patients and their families. Psychiatr Serv 2012;63:616-8.
- Teferra S, Shibre T. Perceived causes of severe mental disturbance and preferred interventions by the Borana semi-nomadic population in southern Ethiopia: a qualitative study. BMC Psychiatry 2012;12:79.
- Corrigan P, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav 2003;44:162-79.
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, et al. The prevalence and correlates of untreated serious mental illness. Health Serv Res 2001;36:987-1007.
- Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry 2005;162:1785-804.