Hong Kong J Psychiatry 2009;19:65-71
ORIGINAL ARTICLE
激躁性結腸症病人的精神病患病率及生活質素
董富賢、胡志遠、許祖紳、陳秀芬
Dr FY Tung, MBBS, MRCPsych, Department of Psychiatry, Tai Po Hospital, Hong Kong, China.
Dr Justin CY Wu, MBChB, FRCP, MD, FHKCP, FHKAM (Medicine), Department of Medicine and Therapeutics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong, China.
Dr AJ Hui, MBChB, MRCP, FHKCP, FHKAM (Medicine), Department of Medicine, Alice Ho Miu Ling Nethersole Hospital, Hong Kong, China.
Dr Teresa SF Chan, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, Tai Po Hospital, Hong Kong, China.
Address for correspondence: Dr FY Tung, Department of Psychiatry, Tai Po
Hospital, Hong Kong, China.
Tel: (852) 2607 6111; Fax (852) 2662 3568; E-mail: tungrobert@hotmail.com
Submitted: 9 October 2008; Accepted: 30 December 2008
Abstract
Objectives: To examine the prevalence of psychiatric disorders, their clinical correlates, and quality of life of outpatients with irritable bowel syndrome.
Participants and Methods: Patients with irritable bowel syndrome attending 2 gastrointestinal clinics were recruited consecutively. The Chinese-Bilingual Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (4th Edition) was used to identify patients who suffered from different kinds of psychiatric illnesses, and the Hong Kong Chinese version of the World Health Organization Quality of Life Measure (abbreviated version) was used to measure quality of life. The quality of life for subjects with and without psychiatric morbidity was compared.
Results: The lifetime and point prevalences of Axis I psychiatric disorders were 69.7% and 43.4% respectively. Depressive disorders were the most commonly diagnosed psychiatric illnesses. Subjects with psychiatric morbidity had a poorer quality of life. None of the socio-demographic and clinical characteristics correlated strongly with the development of psychiatric morbidity.
Conclusions: This study indicates that psychiatric morbidity was frequent among outpatients with irritable bowel syndrome attending gastroenterology clinics in Hong Kong. Screening for psychiatric disorders in gastroenterology clinics is worthwhile.
Key words: Colonic diseases, functional; Depressive disorder; Dyspepsia; Irritable bowel syndrome; Quality of life
摘要
目的:探討激躁性結腸症門診病人的精神病患病率、臨床相關特徵及生活質素。
參與者與方法:到兩所腸胃科診所應診的激躁性結腸症病人。使用《心理疾病診斷統計手冊(第四版)》中文及雙語定式臨床會診量表確定病人的精神病種類,並用WHO生活質素量表中文版(簡化版)量度病人的生活質素。然後比較有精神病和無精神病的病人的生活質素。
結果:被診斷患有Axis I精神病的終生患病率和時點患病率分別為69.7%及43.4%。最常見的精神病為抑鬱症。有精神病的人生活質素較差。社會人口學及臨床特徵均與精神病情發展無顯著相關。
結論:到腸胃科診所應診的激躁性結腸症病人普遍出現精神病現象。於腸胃科診所作精神病篩選是可取的。
關鍵詞:功能性腸病、抑鬱症、消化不良、激躁性結腸症、生活質素
Introduction
Irritable bowel syndrome (IBS) is the commonest functional disorder of the gastrointestinal tract. It is characterised by changes in bowel habits and the presence of abdominal pain. The prevalence of IBS in the Hong Kong Chinese community ranges from 3.7 to 6.6%.1-3
Psychiatric morbidity is prevalent in outpatients with IBS. The lifetime prevalence of depressive and anxiety disorders is up to 76% and 54% respectively.4,5 The point prevalences of depressive and anxiety disorders range from 9.6 to 54% and from 11.1 to 52.4% respectively.4-14
Though IBS is not usually life-threatening, it has a significant impact on quality of life. Reports indicate that the quality of life for people with IBS is lower than that of the general healthy population, and that of patients with other chronic diseases such as gastro-oesophageal reflux and diabetes.15-17 In a local population-based survey, men with IBS were found to have significantly lower vitality scores in the 36-short form (SF-36) scale than the controls and women with IBS had significantly lower mental health scores than the controls.3 Another study found that a significantly higher proportion of IBS subjects (22% versus 6%, p < 0.001) required days-off work when compared with subjects without IBS.1 Furthermore, more subjects with IBS (25% versus 5%, p < 0.001) reported an adverse effect on their social life when compared with subjects without IBS.
In Hong Kong, the prevalence of psychiatric disorders in outpatients with IBS has not been studied. Previous local studies concerning quality of life mainly targeted on the community samples. The quality of life of IBS outpatients is still to be determined. As understanding of the prevalence of psychiatric morbidity in IBS outpatients can shed light on the integration of medical and psychiatric care, empirical studies on local IBS subjects are clearly warranted. This study focused on the prevalence of psychiatric disorders and quality of life in local IBS outpatients.
Methods
Using a cross-sectional design, data were collected from 1 March 2008 to 31 August 2008. Subjects with IBS were identified by their attending gastroenterologists using the Rome III diagnostic criteria for IBS.18 Each was classified into 1 of 4 subtypes: IBS with constipation, IBS with diarrhoea (IBS-D), mixed IBS, or unsubtyped IBS. Recruitment criteria were: being aged from 18 to 65 years and being able to give written informed consent. People with intellectual disabilities, mental retardation, dementia, or severe deficits in comprehension were excluded.
All the people with IBS were recruited consecutively from 2 gastroenterology clinics at the Prince of Wales Hospital (PWH) and the Alice Ho Miu Ling Nethersole Hospital (AHNH). Clinical notes were reviewed for verification of the socio-demographic and clinical data. Ethical approval was obtained from the Clinical Research Ethics Committee of the Chinese University of Hong Kong and the New Territories East Cluster.
Data Collection
Socio-demographic data, clinical characteristics of the IBS, and medical and psychiatric history were recorded. The socio- demographic data included age, sex, current occupation, monthly family income, number of years of education, and marital status. The clinical characteristic of the IBS included the age of onset, duration of the illness, and any family history of IBS. Clinical notes were reviewed for past and current treatment for IBS. Any history of other significant physical illnesses was recorded. The psychiatric history was explored— including any history of outpatient or inpatient treatment; any consultations with psychiatrists, clinical psychologists or general practitioners; any current use of psychotropic medications; and any family history of mental illness.
Assessment Tools
After reading the appropriate manuals and watching the training video tapes, the first author administered the Chinese- Bilingual Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders – 4th Edition, Axis I, Patient version (CB-SCID-I/P).19-21 The Chinese-Cantonese version of the Hospital Anxiety and Depression Scale (HADS) was used to assess the severity of depression and anxiety.22
Quality of life was assessed using the Hong Kong Chinese version of the World Health Organization Quality of Life Measure (abbreviated version; WHOQOL-BREF).23 At the time of assessing psychiatric morbidity, the first author was blind to the HADS and WHOQOL-BREF results but not the IBS subtypes. Anonymous self-rating HADS and WHOQOL-BREF questionnaires were given to those who refused the interview. A stamped, self-addressed envelope was given to enable the return of the questionnaires.
Statistical Analysis
Data were analysed using the Statistical Package for the Social Sciences (Windows version 11.0; SPSS Inc, Chicago [IL], US). The statistical significance level was set at p < 0.05 unless otherwise specified. All patients with psychiatric morbidity were combined into one group whilst those without psychiatric disorders formed another group. Descriptive statistics were used to characterise the socio-demographic and clinical profiles of the entire sample, then the socio-demographic and clinical variables of subjects with and without psychiatric morbidity were compared. Categorical variables were analysed using the Chi-square test or Fisher’s exact test in cases with cell counts of less than 5. Continuous variables were analysed using the t test or Mann-Whitney U test, depending on the distribution of data. When correlation coefficients were statistically significant (p < 0.05) and their absolute values were greater than 0.5, the variables concerned were entered into a binary logistic regression or multiple regression analysis. The binary logistic and multiple regressions were employed to examine the impact of different variables on the development of psychiatric morbidity and WHOQOL-BREF domain scores respectively.
Results
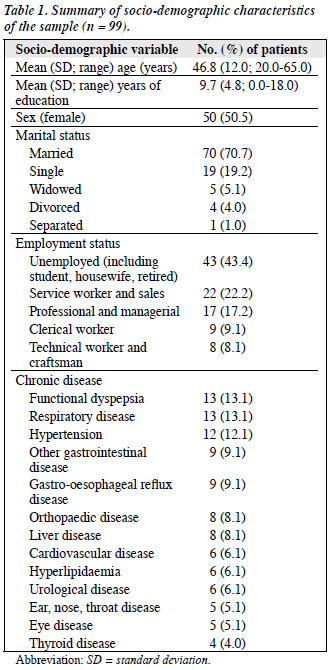
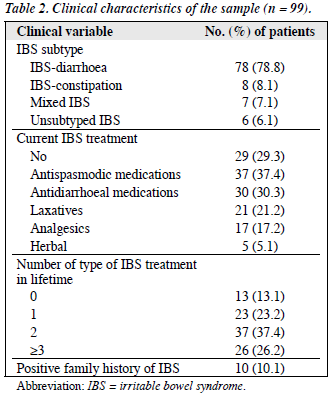
Over the 6-month study period, 104 outpatients with IBS were identified using consecutive sampling. Three refused to participate and two were excluded because they were older than 65 years. The interview was completed in 99 subjects (PWH = 92; AHNH = 7), giving a response rate of 97%. A total of 70 (70.7%) subjects had chronic physical illnesses. Functional dyspepsia (13.1%), respiratory disease (13.1%), and hypertension (12.1%) were the most common chronic physical illnesses in this sample (Table 1). There were no significant differences in age, duration of IBS, and age of onset between respondents and non-respondents. All three non-respondents denied any history of psychiatric illness or use of psychotropic medications. None of them returned the anonymous HADS and WHOQOL-BREF questionnaires. Most (78.8%) subjects were classified as having IBS-D, 29.3% was not receiving any treatment for IBS at the time of interview (Table 2).
Prevalence of Psychiatric Morbidity
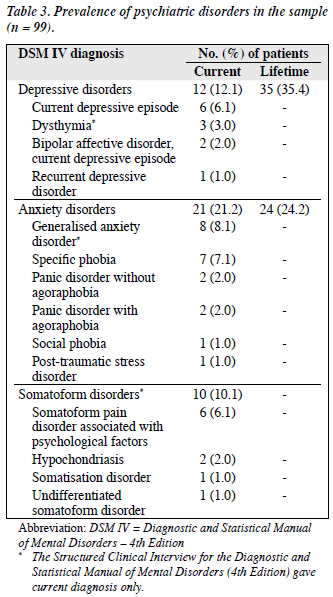
Almost half (49.5%) of the subjects had one or more lifetime psychiatric diagnoses — 32, 14, and 3 patients had 1, 2 and 3 lifetime psychiatric diagnoses, respectively. The corresponding prevalence of lifetime and current psychiatric disorders in this sample were 69.7% and 43.4%. Depressive disorder was the most frequently diagnosed condition with a lifetime and point prevalence of 35.4% and 12.1% respectively. As a group, anxiety disorder was the second most common psychiatric diagnosis with a lifetime and point prevalence of 24.2% and 21.2%. Generalised anxiety disorder was the most common anxiety disorder (8.1%). One-tenth (10.1%) of the sample had somatoform disorder and somatoform pain disorder was diagnosed in 6.1% of those with IBS. No subjects had been diagnosed with alcohol or substance abuse (Table 3).
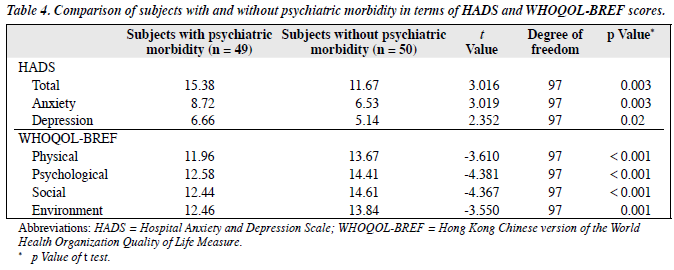
Comparison between Subjects With and Without Psychiatric Morbidity
There were no significant differences in the socio-demographic characteristics of these two groups. The duration of IBS was similar (mean [standard deviation]: 9.4 [6.4] years versus 10.4 [11.0] years; p = 0.59). Patients with IBS with psychiatric morbidity had significantly higher HADS depression and anxiety scores than those without psychiatric morbidity. Subjects with IBS with psychiatric morbidity had significantly lower scores in all 4 WHOQOL-BREF domains (Table 4).
Correlations between Psychiatric Morbidity and Socio-demographic and Clinical Characteristics
None of the socio-demographic characteristics were found to correlate with psychiatric morbidity. There was a significant negative correlation between the presence of gastro-oesophageal reflux disease and psychiatric morbidity (r = –0.25, p = 0.01) but the absolute value of the correlation coefficient was less than 0.5, indicating a small correlation. For this reason, this was not analysed further.
Correlations between WHOQOL-BREF Domain Scores with Socio-demographic and Clinical Characteristics
No socio-demographic characteristics correlated with WHOQOL-BREF domain scores. There were 5 significant correlations between WHOQOL-BREF domain scores and clinical characteristics. The number of chronic physical problems correlated negatively with the WHOQOL-BREF physical (r = –0.22, p = 0.03) and social domain scores (r = –0.20, p = 0.05). There was a significant inverse correlation between the presence of respiratory disease and the WHOQOL-BREF physical domain score (r = –0.22, p = 0.03). Hypertension and gynaecological disease correlated negatively with the WHOQOL-BREF social domain score (r = –0.22, p = 0.03 and r = –0.24, p = 0.02). All the absolute values of these 5 correlation coefficients were less than 0.5, indicating correlations too small to be analysed further.
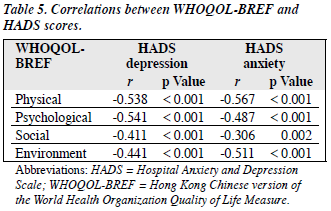
Correlations between WHOQOL-BREF and Hospital Anxiety and Depression Scale Scores
The HADS depression and anxiety scores were found to have significant negative correlations with all 4 WHOQOL- BREF domain scores (Table 5).
Discussion
The mean age of this sample was comparable with that reported in recent studies.11-13 In recent studies, female gender has predominated but overall the female-to-male ratio has been quite variable (range, 1.41-3.03). In our study, the female-to-male ratio was 1.02:1. Most people in the sample were classified as having diarrhoea-predominant IBS. Previous studies have found female gender predominance in constipation-predominant IBS patients.15,24,25 This sample had comparatively low levels of education because they were recruited from gastroenterology clinics in 2 public hospitals which serve citizens with comparatively low monthly family incomes.
The lifetime prevalence of Axis I psychiatric diagnosis (69.7%) in this study was similar to that (66-93%) reported in previous studies.5,12,26 On the other hand, the point prevalence of Axis I psychiatric disorder (43.4%) was not as high as that (47-65.6%) reported in previous studies.11,27
Depressive disorder was the leading psychiatric illness in this sample, affecting 35.4%. This figure is not as high as the lifetime prevalence (46-76%) reported in some previous studies.4,5,8 The lifetime and point prevalences (35.4% and 12.1%) of depressive disorder in our study, however, were very similar to those found by a recent clinic-based study (33.5% and 11.7%).12
Anxiety disorder was the second commonest psychiatric illness in this sample. The point prevalence of anxiety disorders (21.2%) in our group of outpatients was comparable to the finding (22.7%) in another clinic- based study of similar sample size (n = 128) in Japan.13 North American studies have found that anxiety disorders are highly prevalent in IBS outpatients (39.7-52.4%).5,6,12 Only about one-fourth (24.2%) of IBS subjects in this study had a lifetime anxiety diagnosis whereas an earlier study reported that more than half (50.8%) of the patients in their IBS sample had been diagnosed with an anxiety disorder at some point in their lives.12
As in previous studies, our study found that generalised anxiety disorder was the most frequently diagnosed anxiety disorder. Earlier studies have reported a wide variation in generalised anxiety disorder point prevalence, from 2.8 to 58%.4,5,8-10 but it did not exceed one-third (13.6-31.9%) in more recent studies.11,12,14 Our study found a lower point prevalence for generalised anxiety disorder (8.1%).
Somatoform disorder was less prevalent than mood and anxiety disorders in our IBS subjects, with somatoform pain disorder being the commonest somatoform disorder (6.1%). There is a paucity of data, however, on the prevalence of somatoform pain disorder in IBS outpatients. Only 2 previous studies included IBS subjects diagnosed with somatoform pain disorder but their findings on lifetime prevalence differed greatly (0.8% versus 12.9%).12,13 None of the IBS subjects in our study were diagnosed as alcohol abusers. In other recent studies, the lifetime prevalence of alcohol abuse among IBS outpatients ranged from 8 to 9%.12,26
Depressive disorders are commonly associated with comorbid anxiety or somatoform disorders. In this study, among those 14 IBS outpatients with 2 lifetime diagnoses, 10 had a depressive episode comorbid with an anxiety disorder whilst another 2 had a depressive episode comorbid with a somatoform disorder. All the 3 IBS subjects with 3 lifetime diagnoses had a depressive episode comorbid with 2 anxiety disorders.
People with IBS suffer from chronic physical symptoms and are at greater risk of developing psychiatric problems, leading to a high prevalence of lifetime psychiatric diagnoses. It has been hypothesised that higher systems, such as the autonomic nervous system and the brain-gut axis, are involved in the pathophysiological mechanisms underlying the co-existence of IBS and psychiatric symptoms. For example, a brain-gut model of IBS is offered as an explanation of the high prevalence of anxiety disorders in IBS patients.28 It has been proposed that the emotion-motor system, made up of the visceral motor cortex, the amygdala, the hypothalamic nuclei and peri- aqueductal grey matter, plays a central role in mediating IBS and anxiety symptoms.29,30
Patients with psychiatric morbidity had significantly lower scores in all 4 WHOQOL-BREF domains. The association between poorer quality of life and psychiatric morbidity in IBS outpatients was addressed in a recent study which showed that depressive disorder, panic disorder, and neurasthenia were associated with impaired physical role limitation scores in SF-36 at baseline in outpatients with severe IBS.27 The number of psychiatric diagnoses at baseline predicted SF-36 physical role limitation scores at the follow-up.
In this study, the socio-demographic and clinical characteristics did not have strong correlations with both psychiatric morbidity and all the WHOQOL-BREF domain scores. On the other hand, HADS depression and anxiety scores correlated significantly with all the 4 WHOQOL- BREF domain scores. As this was a cross-sectional study, the direction of the causal relationship between psychiatric symptoms and quality of life could not be elucidated. In 2 recent studies, Hamilton depression scores and 2 depressive symptoms (tiring easily and low in energy) were found to be significant independent predictors for SF-36 physical component scores.31,32 Distressing IBS symptoms, co-existing psychiatric disorders, and other somatic comorbidities can lead to reduction of quality of life in IBS patients.
The predominance of IBS-D subjects in our sample was not commonly observed in previous studies using the Rome I or II criteria. This could be due to the difference between the Rome III criteria and previous versions. More local studies are needed to determine whether there is a genuine difference in the proportion of IBS subtypes seen in our sample and clinic-based samples from Europe and North America. The predominance of the IBS-D subtype in our sample may explain some of the differences in the prevalence of psychiatric morbidities between this study and previous ones. For example, the lifetime and point prevalences for anxiety disorders were lower in our sample than those reported in previous studies. This suggests that diarrhoea-predominant IBS and anxiety disorders do not share a common pathophysiological mechanism. Further studies on the aetiology of IBS with comorbid psychiatric disorders are warranted.
This was the first local study to assess the prevalence of psychiatric morbidity in IBS outpatients with a semi- structured diagnostic interview tool. The CB-SCID-I/P, used to establish psychiatric diagnoses, has been shown to be a reliable instrument for diagnosing mood and anxiety disorders in the Hong Kong Chinese population.20-22 Subjects were identified by their attending gastroenterologists, using the Rome III diagnostic criteria, ensuring a sensitive diagnosis of IBS and a homogenous sample. This was a study involving 2 gastrointestinal clinics, increasing the likelihood that a representative sample of IBS outpatients attending gastrointestinal clinics in Hong Kong was collected. The high response rate (97%) minimised the risk of response bias.
There were several limitations to this study. Firstly, the information provided by subjects might be fraught with recall bias. Secondly, being cross-sectional, this study cannot be used to determine a causal relationship between psychiatric disorders and quality of life. Further prospective studies are needed to examine the direction of any causal link. Thirdly, the lack of a control group was another shortcoming, rendering this study unable to ascertain whether the quality of life of IBS outpatients in gastroenterology clinics was poorer than that of healthy individuals in the community. Finally, a sampling bias was inevitable due to the inclusion of more severe IBS cases in the tertiary referral centres used for recruiting the sample. Samples recruited in clinical settings are also unlikely to be representative of the general population.
This study found that the prevalence of psychiatric morbidity among outpatients with IBS was high and those who had psychiatric disorders had an associated poorer quality of life. Therefore, physicians managing IBS outpatients should screen them for psychiatric morbidity. The establishment of integrated clinics attended by medical and psychiatric specialists is another possible means of developing holistic care for IBS outpatients in Hong Kong.
Declaration
No conflicts of interest were declared by authors.
References
- Hu WH, Wong WM, Lam CL, Lam KF, Hui WM, Lai KC, et al. Anxiety but not depression determines health care-seeking behaviour in Chinese patients with dyspepsia and irritable bowel syndrome: a population-based study. Aliment Pharmacol Ther 2002;16:2081-8.
- Kwan AC, Hu WH, Chan YK, Yeung YW, Lai TS, Yuen H. Prevalence of irritable bowel syndrome in Hong Kong. J Gastroenterol Hepatol 2002;17:1180-6.
- Lau EM, Chan FK, Ziea ET, Chan CS, Wu JC, Sung JJ. Epidemiology of irritable bowel syndrome in Chinese. Dig Dis Sci 2002;47:2621-4.
- Walker EA, Gelfand AN, Gelfand MD, Katon WJ. Psychiatric diagnoses, sexual and physical victimization, and disability in patients with irritable bowel syndrome or inflammatory bowel disease. Psychol Med 1995;25:1259-67.
- Walker EA, Roy-Byrne PP, Katon WJ, Li L, Amos D, Jiranek G. Psychiatric illness and irritable bowel syndrome: a comparison with inflammatory bowel disease. Am J Psychiatry 1990;147:1656-61.
- Blanchard EB, Scharff L, Schwarz SP, Suls JM, Barlow DH. The role of anxiety and depression in the irritable bowel syndrome. Behav Res Ther 1990;28:401-5.
- Blanchard EB, Scharff L, Payne A, Schwarz SP, Suls JM, Malamood H. Prediction of outcome from cognitive-behavioral treatment of irritable bowel syndrome. Behav Res Ther 1992;30:647-50.
- Lydiard RB, Fossey MD, Marsh W, Ballenger JC. Prevalence of psychiatric disorders in patients with irritable bowel syndrome. Psychosomatics 1993;34:229-34.
- Blewett A, Allison M, Calcraft B, Moore R, Jenkins P, Sullivan G. Psychiatric disorder and outcome in irritable bowel syndrome. Psychosomatics 1996;37:155-60.
- Trikas P, Vlachonikolis I, Fragkiadakis N, Vasilakis S, Manousos O, Paritsis N. Core mental state in irritable bowel syndrome. Psychosom Med 1999;61:781-8.
- Blanchard EB, Keefer L, Galovski TE, Taylor AE, Turner SM. Gender differences in psychological distress among patients with irritable bowel syndrome. J Psychosom Res 2001;50:271-5.
- Sykes MA, Blanchard EB, Lackner J, Keefer L, Krasner S. Psychopathology in irritable bowel syndrome: support for a psychophysiological model. J Behav Med 2003;26:361-72.
- Handa M, Nukina H, Ando K, Kubo C. What does pain or discomfort in irritable bowel syndrome mean? Dig Dis Sci 2004;49:575-8.
- Creed F, Tomenson B, Guthrie E, Ratcliffe J, Fernandes L, Read N, et al. The relationship between somatisation and outcome in patients with severe irritable bowel syndrome. J Psychosom Res 2008;64:613-20.
- Chang L. Review article: epidemiology and quality of life in functional gastrointestinal disorders. Aliment Pharmacol Ther 2004;20 Suppl 7: S31-9.
- Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related qualify of life. Gastroenterology 2000;119:654-60.
- Halder SL, Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Impact of functional gastrointestinal disorders on health- related quality of life: a population-based case-control study. Aliment Pharmacol Ther 2004;19:233-42.
- Pae CU, Masand PS, Ajwani N, Lee C, Patkar AA. Irritable bowel syndrome in psychiatric perspectives: a comprehensive review. Int J Clin Pract 2007;61:1708-18.
- So E, Kam I, Liu Z, Fong S, Chung D, Leung CM. The Chinese bilingual SCID-I/P project: stage 1 — reliability for mood disorders and schizophrenia. Hong Kong J Psychiatry 2003;13:7-18.
- So E, Kam I, Leung CM, Pang A, Lam L. The Chinese bilingual SCID- I/P project: stage 2 — reliability for anxiety disorders, adjustment disorders and ‘no diagnosis’. Hong Kong J Psychiatry 2003;13:19-25.
- So E, Kam I, Lam L. The Chinese bilingual SCID-I/P project: stage 3 — multi-site inter-rater reliability. Hong Kong J Psychiatry 2005;14:19-25.
- Leung CM, Wing YK, Kwong PK, Lo A, Shum K. Validation of the Chinese-Cantonese version of the hospital anxiety and depression scale and comparison of the Hamilton Rating Scale of Depression. Acta Psychiatr Scand 1999;100:456-61.
- Leung KF, Tay M, Cheng SSW, Lin F. Hong Kong Chinese version World Health Organization quality of life measure – abbreviated version (WHOQOL-BREF). Proceedings of Hong Kong Project Team on the Development of the Development of the Hong Kong Chinese version WHOQOL. Hong Kong: Hong Kong Hospital Authority 1997:1-64.
- Si JM, Wang LJ, Chen SJ, Sun LM, Dai N. Irritable bowel syndrome consulters in Zhejiang province: the symptoms pattern, predominant bowel habit subgroups and quality of life. World J Gastroenterol 2004;10:1059-64.
- Talley NJ, Zinsmeister AR, Melton LJ 3rd. Irritable bowel syndrome in a community: symptom subgroups, risk factors, and health care utilization. Am J Epidemiol 1995;142:76-83.
- Jarrett M, Heitkemper M, Cain KC, Tuftin M, Walker EA, Bond EF, et al. The relationship between psychological distress and gastrointestinal symptoms in women with irritable bowel syndrome. Nurs Res 1998;47:154-61.
- Creed F, Ratcliffe J, Fernandes L, Palmer S, Rigby C, Tomenson B, et al. Outcome in severe irritable bowel syndrome with and without accompanying depressive, panic and neurasthenic disorders. Br J Psychiatry 2005;186:507-15.
- Lydiard RB. Irritable bowel syndrome, anxiety and depression: what are the links? J Clin Psychiatry 2001;62 Suppl 8:S38-47.
- Mayer EA. The neurobiology of stress and gastrointestinal disease. Gut 2000;47:861-9.
- Mayer EA, Fanselow MS. Dissecting the components of the central response to stress. Nat Neurosci 2003;6:1011-2.
- Creed F, Ratcliffe J, Fernandez L, Tomenson B, Palmer S, Rigby C, et al. Health-related quality of life and health care costs in severe, refractory irritable bowel syndrome. Ann Intern Med 2001;134:860-8.
- Spiegel BM, Gralnek IM, Bolus R, Chang L, Dulai GS, Mayer EA, et al. Clinical determinants of health-related quality of life in patients with irritable bowel syndrome. Ann Intern Med 2004;164:1773-80.
Corrigendum
On page 1 of the March issue (Volume 19), the Honorary Advisors list was not updated. The new updated list is included in this issue. We regret the error.