East Asian Arch Psychiatry 2015;25:150-159
ORIGINAL ARTICLE
Dr Lai-Yi Wong, MBBS, Kwai Chung Hospital, Hong Kong SAR, China.
Dr Ramon Yiu Lo, MBBS, MRCS, Department of Orthopaedics and Traumatology, Tseung Kwan O Hospital, Hong Kong SAR, China.
Dr Chi-Kit Chiu, MBBS, FRCSEd (Orth), FHKCOS, FHKAM (Orthopaedic Surgery), Department of Orthopaedics and Traumatology, Tseung Kwan O Hospital, Hong Kong SAR, China.
Dr Wing-King Lee, MBChB, FRCPsych (UK), FHKCPsy, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Dr Yuen-Lun Lee, MBBS, FRCS (Edn), FHKCOS, FHKAM (Orthopaedics and Traumatology), Department of Orthopaedics and Traumatology, Tseung Kwan O Hospital, Hong Kong SAR, China.
Dr Po-Keung Kwong, MBBS, FRCPsych, FHKAM (Psychiatry), FHKCPsy, Kwai Chung Hospital, Hong Kong SAR, China.
Dr William Tak-Lam Lo, MBBS, FRCPsych, FHKCPsy, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Address for correspondence: Dr Lai-Yi Wong, Kwai Chung Hospital, Hong Kong SAR, China.
Tel: (852) 9248 1502; Email: katherine_wly@yahoo.co.uk
Submitted: 19 May 2015; Accepted: 10 August 2015
Abstract
Objectives: To identify the prevalence and associated factors of psychiatric morbidities and to evaluate the effectiveness of the Hospital Anxiety and Depression Scale (HADS) in screening for psychiatric morbidity in patients with knee osteoarthritis in a local orthopaedic clinic.
Methods: A cross-sectional study was conducted from October 2013 to June 2014 to examine patients with knee osteoarthritis at a specialist orthopaedic clinic. They were evaluated for psychiatric diagnoses using the Structured Clinical Interview for the DSM-IV Axis I Disorders (SCID-I). Socio-demographic and clinical characteristics were compared between patients with and without psychiatric morbidity. Patients were also assessed using the HADS with accuracy compared with the psychiatric diagnoses made by the SCID-I.
Results: Of the 115 patients, 39% had current psychiatric disorders. Logistic regression analysis revealed that limitation of physical activity, perceived absence of confidant, a history of psychiatric illness, and follow-up in orthopaedic clinic for ≥ 5 years were independent factors associated with psychiatric disorders.
Conclusions: The prevalence of psychiatric morbidity in patients with knee osteoarthritis was significant. Recognition of independent associated factors can aid in early identification and intervention in patients who are at risk of developing psychiatric morbidity. The HADS is a useful means to screen for psychiatric morbidity in these patients.
Key words: Anxiety; Depression; Disability evaluation; Osteoarthritis, knee; Pain
Introduction
Knee osteoarthritis (knee OA) is a common degenerative joint condition and one of the most common causes of disability and pain in the elderly. According to a US study, the prevalence of radiographic knee OA > 63 years is around 30%, and it increases with age.1 The prevalence of knee OA in Chinese men is similar to that in Caucasian men, but is significantly higher among Chinese women than Caucasian women.2 The Beijing Osteoarthritis Study showed that in a population group aged ≥ 60 years, the prevalence of radiographic knee OA was 42.8% in women and 21.5% in men. Symptomatic knee OA occurred in 15.0% of women and 5.6% of men.2 Hong Kong is now facing an ageing population,3 and knee OA is expected to become an increasingly prevalent condition.
The most frequent symptoms of knee OA are chronic pain and physical limitation. Knee OA has a substantial impact on quality of life.4,5 The prevalence of anxiety and depression is high in affected patients6 and increasing research data reveal that preoperative mood disorders can significantly affect the postoperative outcome following total knee replacement, the most definitive management for knee OA.7 Local studies to specifically examine the prevalence of psychiatric morbidity in patients with knee OA are nonetheless lacking.
Knee OA has great physical and psychological impact on patients as well as imposing a local socio-economic burden.8 In view of the high prevalence of knee OA in this locality and the clinical importance of psychiatric morbidity in this group of patients, a local study was considered necessary to determine the nature and prevalence of psychiatric morbidity among Chinese knee OA patients in Hong Kong. This study also examined factors associated with psychiatric morbidity, and assessed the effectiveness of a convenient screening tool, the Hospital Anxiety and Depression Scale (HADS), in assisting surgeons or physicians in identification of knee OA patients with psychiatric disorders.
Methods
Subjects
All consecutive patients of Chinese ethnicity aged > 18 years with knee OA, who attended the Joint Replacement Clinic (JRC) of Tseung Kwan O Hospital (TKOH) in the Kowloon East Cluster of the Hospital Authority (HA) in Hong Kong from October 2013 to June 2014, were recruited. The criteria for referral of knee OA patients to the JRC of TKOH were failed conservative treatment for ≥ 6 months in a general orthopaedic clinic, and patients for whom arthroplasty was considered a treatment option. The recruited subjects had never undergone knee arthroplasty. Those who were unable to comprehend Chinese or who were cognitively impaired were excluded. Patients aged ≥ 65 years or with a history of cerebrovascular disease were screened using the Mini- Mental State Examination (MMSE). The cutoff score was ≤ 18 for those who had no formal education; ≤ 20 for those with 1 to 2 years of education, and ≤ 22 for those with > 2 years of education.9 This study was approved by the Clinical Research Ethics Committee of the HA and written consent was obtained from all patients.
Assessment
The diagnosis of knee OA was confirmed by an orthopaedic surgeon on the basis of clinical assessment and radiological findings. All psychiatric interviews were conducted by the principal author using the locally validated Chinese version of the Structured Clinical Interview for the DSM-IV Axis I Disorders (SCID-I). The test-retest reliability between SCID-I raters was a kappa of 0.84 for mood disorders and schizophrenia.10 The overall kappa for the clinician-rater reliability in anxiety disorders, adjustment disorders and ‘no diagnosis’ was 0.71.10 The overall percentage agreement for the principal diagnoses in out-patient settings at 4 different sites was 80%.11
The HADS is a widely used self-reported instrument, first designed to detect anxiety and depression in non- psychiatric out-patient clinics by excluding somatic items.12 It reliably detects states of depression and anxiety in a wide variety of clinical populations, where anxiety and depression may co-exist with physical illness. The HADS includes 2 subscales, one for anxiety (HADS-A) and one for depression (HADS-D), with 7 questions in each arranged in alternative order. Each answer has 4 options with a score of 0 to 3. The subscales thus have a maximum score of 21. It has been reported to perform well in assessing symptom severity and incidence of depression and anxiety disorders in a variety of settings.13 The cutoff point for the subscales (HADS-D, HADS-A) or the HADS total (HADS-T) is set at different levels, depending on the study population and the purpose of scoring. The Chinese-Cantonese version of the HADS was found to have good internal consistency and external validity, with favourable sensitivity and specificity when used to screen for psychiatric disorders.14 The usefulness of HADS in detecting anxiety disorders and depression has also been proven in patients with musculoskeletal problems.15 It has been useful in the Chinese elderly population16 as well as other medically ill patients in local studies.17,18
The Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS) measures physical function derived from the activities of daily living (ADL) and sport-recreation subscales of the KOOS.19 The KOOS-PS is a 7-item self-rated questionnaire that takes approximately 2 minutes for patients to complete. It measures the degree of difficulty experienced in everyday tasks over the previous week due to knee OA. All items are scored on a 5-point Likert scale ranged from 0 to 4. The raw score is the sum of the 7 items. The interval score from 0 to 100 is obtained using a conversion chart.19 As items in KOOS-PS are taken directly from KOOS, which has face and content validity, this can also be assumed for the KOOS-PS.20 The reliability and validity of KOOS has been well accepted in the Chinese population.21
A visual analogue scale (VAS) for pain is a simple self-rated means to assess intensity of pain. It is a continuous scale that comprises a horizontal or vertical line, usually 10 cm in length. It is anchored by 2 verbal descriptors, one for each symptom extreme. Using a ruler, the score is determined by measuring in millimetres the distance of a mark on the 10-cm line between the “no pain” anchor and the patient’s mark, providing a range of scores from 0 to 100. A higher score indicates greater pain intensity. For construct validity, in patients with a variety of rheumatic diseases, the pain VAS has been shown to highly correlate with a 5-point verbal descriptive scale (“nil,” “mild,” “moderate”, “severe,” and “very severe”) and a numeric rating scale (with response options from “no pain” to “unbearable pain”), with correlations ranging from 0.71 to 0.78 and 0.62 to 0.91, respectively.22,23 It is shown that VAS for pain has high reliability and sensitivity in knee OA patients.24
Statistical Analyses
All statistical analyses were performed using the Statistical Package for the Social Sciences Windows version 20.0 (SPSS Inc., Chicago [IL], US). To evaluate the performance of HADS against the gold standard diagnoses by SCID-I, the receiver operating characteristic curve was used.
Results
From October 2013 to June 2014, 124 subjects in the JRC at TKOH were approached. A total of 9 patients were excluded of whom 7 were deemed by the MMSE to have cognitive impairment. One patient refused to participate in the study due to concerns about privacy and the other could not speak Cantonese. Overall, 115 patients were enrolled. The response rate was 99%.
Socio-demographic Characteristics
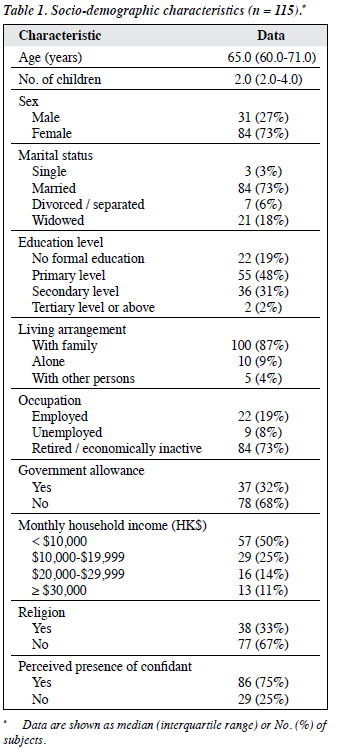
Table 1 describes the socio-demographic characteristics of patients. Among the enrolled 115 patients, the mean (± standard deviation [SD]) age was 65.4 ± 8.2 years. In all, 73% were women and 27% were men. Most were married (73%), educated to a primary or secondary school level (79%), lived with family (87%), and were retired or economically inactive (73%). In addition, 32% were in receipt of government allowance and 25% reported absence of a confidant.
Medical Background
In all, 89.6% of the patients suffered chronic medical illness(es) other than knee OA: 77.4% reported 1 to 3 chronic illnesses. The most common co-morbidities were cardiovascular (mainly hypertension) and endocrine- metabolic disease (mainly diabetes mellitus) affecting 57.4% and 51.3% of patients, respectively.
Psychiatric Background
A history of psychiatric illness was reported by 12.2% of subjects. Psychiatric services were involved in the care of 7.8% and 13.9% of subjects had a family history of psychiatric illness.
Psychiatric Morbidity
The point and lifetime prevalence of psychiatric disorders are shown in Table 2. The point prevalence of any psychiatric disorder was 39%, and that of any depressive disorder was 29% and any anxiety disorder being 24%. Major depressive disorder (MDD) was the most common depressive disorder, with a point prevalence of 27%. Generalised anxiety disorder was the most common anxiety disorder, with a point prevalence of 18%. One patient had an active diagnosis of alcohol abuse and another had organic psychosis. One patient had an active diagnosis of bipolar affective disorder but was in remission at the time of interview. No patient was suffering from schizophrenia at the time of the study.
The lifetime prevalence of any psychiatric disorder was 47%. Depressive disorders had a lifetime prevalence of 31% and anxiety disorders had a lifetime prevalence of 24%. Alcohol abuse had a lifetime prevalence of 4%. In addition, 27 (23%) patients had 1 current psychiatric diagnosis, 17 (15%) had 2, and 1 (0.9%) had 3.
Independent Factors Associated with Psychiatric Disorders
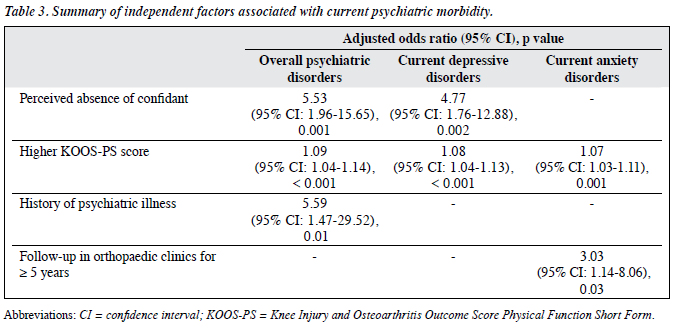
All of the potential predictors associated with p < 0.1 according to bivariate analysis and factors with clinical significance were entered into the logistic regression to determine the presence of a statistically significant association with psychiatric disorders, depressive disorders, and anxiety disorders. The entered factors were checked for multicollinearity. The level of statistical significance was set at 0.05. Table 3 summarises the independent factors associated with psychiatric disorders.
Effectiveness of the Hospital Anxiety and Depression Scale as a Screening Instrument for Psychiatric Disorders
The HADS-T and subscale scores for patients with psychiatric disorders were statistically higher than for those with no current psychiatric disorder. For current overall psychiatric disorders, HAD-T had the largest area under the curve (AUC) and thus had the greatest discriminatory power in screening patients with current overall psychiatric disorders (Fig a). The optimal cutoff score of HADS-T was 13/14, with a sensitivity of 84.4% and specificity of 87.1%. For current depressive disorders, HADS-D had the largest AUC and the optimal cutoff score was 7/8, with a sensitivity of 93.9% and specificity of 89% (Fig b). For current anxiety disorders, HADS-A had the largest AUC and the optimal cutoff score was 7/8, with a sensitivity of 96.4% and specificity of 81.6% (Fig c).
Discussion
Demographic and Clinical Characteristics
Among the 115 subjects enrolled, 73% were female and 27% were male. This is consistent with the existing literature that reveals a higher prevalence of both radiological and symptomatic knee OA in females than in males, in both a Chinese population2 and an overseas population.1 Different hypotheses have been applied to account for this gender difference: women’s lower body is more elastic and thus more mobile, causing the lower limb joints to be more prone to degeneration; the hips of women are wider than men giving rise to a less straight lower limb alignment that could increase the rate of knee injuries predisposing to knee OA. Oestrogen protects cartilage from inflammation. After menopause, there is a drop in oestrogen level and a consequent increased risk of developing knee OA in postmenopausal women.25
Most of the patients were in the retired / economically inactive group (73%). This may be because most of them were female (73%), mostly housewives and most were older adults (median age being 65 years).
In regard to characteristics of knee OA, most patients had been under the care of an orthopaedic specialty clinic for ≥ 5 years (52%), but had yet to be referred for arthroplasty. This confirms the chronicity of the disease and the possibility of a long waiting time for arthroplasty in the locality. The long follow-up duration may also be explained by the nature of a subspecialty clinic in this study. Patients with knee OA may be followed up in a general orthopaedic clinic for a long period of time before being referred to a subspecialty clinic. Since 55% of the patients were not ambulatory (including those who were wheelchair-bound and walked with stick, tripod, or frame), the study population may have had relatively advanced symptomatic stage of knee OA.
Prevalence of Psychiatric Morbidity
The prevalence of current psychiatric disorders was 39%. Depressive disorders (29%) were the most common, followed by anxiety disorders (24%). Consistent with existing literature on the prevalence of psychiatric disorders in arthritis, depressive and anxiety disorders were the most common psychiatric disorders.26-29
A review of the literature revealed that most researchers have investigated depressive symptoms, not anxiety symptoms.30-33 This study revealed that anxiety disorders are also common among knee OA patients and should be given more attention.
Co-morbid current depressive and anxiety disorders were present in 16 (14%) patients. This has been found to have a significant impact on physical functioning and general wellbeing in older adults34 who endure a more chronic course of illness.35
There were no patients with a current or lifetime diagnosis of panic disorder, agoraphobia, social phobia, obsessive-compulsive disorder, or post-traumatic stress disorder but this may be due to the relatively small sample size of the current study.
Despite the high prevalence of current psychiatric disorders, only 20% of those 45 patients with a current psychiatric disorder were receiving active psychiatric care. This phenomenon is not uncommon wherein psychiatric problems are overlooked in a non-psychiatric setting. It has been reported in other groups of patients with painful OA33 and in local patients with other chronic medical conditions.36,37 This phenomenon may be explained by the avoidance of stigma, overlap of physical and psychiatric symptoms among the elderly age-group, and the lack of awareness of psychiatric disorders by attending doctors.
Factors Associated with Psychiatric Morbidity
Perceived absence of confidant
Social support can have a role in reducing stress, and is particularly important in later adulthood because of the often stressful life transitions that can company ageing (e.g. widowhood, acute or chronic medical illnesses).38,39 Patients with knee OA face various difficulties that range from dealing with the distressing pain and limitation of physical function, to the stress of making treatment decisions (including arthroplasty, a major operation), and subsequent participation in a rehabilitation programme. The presence of a confidant was evaluated as a factor that would reflect the level of perceived social support.
Social support is related to psychological wellbeing and quality of life in OA patients.40,41 Lack of social support or social contact is associated with depression and functional limitation in knee OA patients.30-32 A local study found that having less social support was associated with increased likelihood of depression among older adults.42 In the current study, perceived absence of confidant was an independent factor that predicted current overall psychiatric disorders, depressive disorders, and anxiety disorders. This finding is consistent with the current literature.31,43
Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form
The KOOS-PS measures physical function related to a patient’s ADL. Consistent with existing literature,28,32,33,44,45 our study confirmed that the KOOS-PS score was independently associated with current overall presence of psychiatric disorders, depressive disorders, and anxiety disorders.
Disability is closely linked to psychological distress. The age-adjusted prevalence of serious psychological distress among adults with disability has been reported to be almost 7 times that of adults without disabilities.46 Better mental health is also associated with a better long- term physical outcome in knee OA patients.47 Management of mood problems in arthritis patients improves functional outcome.48 Depression can predict disability49; while disability is a known factor that can worsen pain and can predict depression.50 Knee OA patients with a high anxiety level have a high fear-avoidance belief and may catastrophise their pain leading to a higher disability level.51 Anxiety in knee OA patients also leads to avoidance of pain-related activities, and results in muscle weakness and creates a cycle of reduced mobility and pain. Nonetheless disability is associated with increased anxiety level.52
Duration of Orthopaedic Clinic Follow-up
Duration of follow-up in an orthopaedic clinic for ≥ 5 years was associated with current presence of anxiety disorders. The longer duration of orthopaedic clinic follow- up suggests the chronicity of knee OA, and thus chronicity of pain and disability. These might lead to a stronger fear- avoidance belief and be attributed to the association with anxiety disorders.
Clinical Implications
The present study demonstrated the unmet need for psychiatric treatment in knee OA patients. Due to the limited social health care resources and the ageing population, the waiting time for knee arthroplasty is now even longer in local public hospitals. It is not uncommon for patients to wait several years for surgery, and this does not include the waiting time for referral from primary care through the multiple levels to a subspecialty orthopaedic clinic.53 The emotional distress may be under-recognised and under-addressed by the treating surgeon. Psychiatric disorders in knee OA patients have been shown to have a detrimental effect to knee OA symptom severity, treatment outcome, patient’s quality of life, and the socio-economic burden to society.8 There is a need for orthopaedic surgeons to pay more attention to the psychosocial aspects of patient care, especially for those who are vulnerable to psychiatric morbidities. Staff in orthopaedic clinics should increase their awareness of the early symptoms of psychiatric disorders. Education about mental health should be provided to patients and their family. The inclusion of HADS with a cutoff threshold of 13/14 of a total score offers a practical way to screen for psychiatric morbidity in a busy orthopaedic clinic. Patients who screen positive should be given the option to be referred to mental health services for further evaluation so that appropriate management can be offered. Psychosocial intervention should be an integral part of the management of knee OA patients. It has been reported that a combination of orthopaedic and psychosocial care in patients with OA improves outcome.48,54
Strengths and Limitations
This is the first local study of the prevalence of psychiatric morbidity in patients with knee OA. The diagnosis of knee OA is based on more stringent radiological and clinical findings. The diagnosis of psychiatric morbidity used a validated standardised semi-structured interview as a diagnostic tool to generate an accurate and reliable diagnosis. The effectiveness of the HADS as a screening instrument was evaluated against the gold standard of psychiatric diagnoses, and has not been studied before. In addition, this study focused on knee OA with a more homogeneous sample, instead of a broad inclusion of arthritis or OA patients. The response rate was achieved at a high level of 99% without randomisation to give a representative sample.
This was a cross-sectional study and cannot determine a causal relationship between psychiatric morbidity and knee OA. Prospective studies are required to determine the exact causal relationship and the predictive factors in knee OA patients. This study lacked a control group so comparison of the prevalence of psychiatric morbidity and associated factors could not be made between patients with knee OA and controls without knee OA. All patients were recruited in the subspecialty orthopaedic clinic (JRC of TKOH) and thus may have represented a sample with more advanced disease. It is uncertain whether they are representative of local patients with knee OA as management of knee OA can be provided by general practice clinics, general orthopaedic clinics, and the private sector. The elderly Chinese may also seek help from traditional Chinese medicine practitioners for management of their musculoskeletal complaints. Future study should be conducted in a multi-centre setting to give a more representative sample. The recruitment of patients in a clinic setting also excluded patients with knee OA who were severely physically or mentally ill. Knee OA patients with significant cognitive impairment were also excluded.
If time and resources allow, a more comprehensive assessment of social support should be carried out due to its significant association with psychiatric morbidity. More dimensions of knee OA outcome can be assessed using more comprehensive questionnaires such as Western Ontario and McMaster Universities Arthritis Index and KOOS. Nonetheless a lengthy assessment may reduce the willingness of patients, especially the elderly, to participate in the study.
This study relied heavily on the patient’s account of past experiences and feelings, so it might pose potential recall bias. Collateral information from a patient’s significant others may help solve this problem. The SCID also has its limitations. It does not cover lifetime prevalence of generalised anxiety disorder, dysthymic disorder or adjustment disorder and thus it might underestimate the lifetime prevalence of overall psychiatric morbidity.
Conclusions
The findings of the current study suggest that psychiatric morbidity, especially depressive disorders and anxiety disorders, are prevalent in patients with knee OA. The HADS can be considered a screening instrument to facilitate early detection of psychiatric morbidity in the clinical setting in patients with knee OA.
Declaration
The authors declared no conflict of interest in this study.
References
- Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 1987;30:914-8.
- Zhang Y, Xu L, Nevitt MC, Aliabadi P, Yu W, Qin M, et al. Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: The Beijing Osteoarthritis Study. Arthritis Rheum 2001;44:2065-71.
- Hong Kong Population Projections 2012-2041. Hong Kong SAR: Census and Statistics Department; 2012.
- Woo J, Lau E, Lee P, Kwok T, Lau WC, Chan C, et al. Impact of osteoarthritis on quality of life in a Hong Kong Chinese population. J Rheumatol 2004;31:2433-8.
- Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Saika A, et al. Impact of knee and low back pain on health-related quality of life in Japanese women: the Research on Osteoarthritis Against Disability (ROAD). Mod Rheumatol 2010;20:444-51.
- Axford J, Butt A, Heron C, Hammond J, Morgan J, Alavi A, et al. Prevalence of anxiety and depression in osteoarthritis: use of the Hospital Anxiety and Depression Scale as a screening tool. Clin Rheumatol 2010;29:1277-83.
- Vissers MM, Bussmann JB, Verhaar JA, Busschbach JJ, Bierma- Zeinstra SM, Reijman M. Psychological factors affecting the outcome of total hip and knee arthroplasty: a systematic review. Semin Arthritis Rheum 2012;41:576-88.
- Woo J, Lau E, Lau CS, Lee P, Zhang J, Kwok T, et al. Socioeconomic impact of osteoarthritis in Hong Kong: utilization of health and social services, and direct and indirect costs. Arthritis Rheum 2003;49:526- 34.
- Chiu HF, Lam LC, Chi I, Leung T, Li SW, Law WT, et al. Prevalence of dementia in Chinese elderly in Hong Kong. Neurology 1998;50:1002- 9.
- So E, Kam I, Leung CM, Chung D, Liu Z, Fong S. The Chinese- bilingual SCID-I/P project: stage 1 — reliability for mood disorders and schizophrenia. Hong Kong J Psychiatry 2003;13:7-18.
- So E, Kam I, Lam L. The Chinese-bilingual SCID-I/P project: stage 3 — multi-site inter-rater reliability. Hong Kong J Psychiatry 2004;14:19-25.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70.
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77.
- Leung CM, Wing YK, Kwong PK, Lo A, Shum K. Validation of the Chinese-Cantonese version of the hospital anxiety and depression scale and comparison with the Hamilton Rating Scale of Depression. Acta Psychiatr Scand 1999;100:456-61.
- Härter M, Reuter K, Gross-Hardt K, Bengel J. Screening for anxiety, depressive and somatoform disorders in rehabilitation — validity of HADS and GHQ-12 in patients with musculoskeletal disease. Disabil Rehabil 2001;23:737-44.
- Lam CL, Pan PC, Chan AW, Chan SY, Munro C. Can the Hospital Anxiety and Depression (HAD) Scale be used on Chinese elderly in general practice? Fam Pract 1995;12:149-54.
- Martin CR, Thompson DR, Chan DS. An examination of the psychometric properties of the Hospital Anxiety and Depression Scale in Chinese patients with acute coronary syndrome. Psychiatry Res 2004;129:279-88.
- Wong VT, Yu DK. Usefulness of the Hospital Anxiety and Depression Scale for screening for psychiatric morbidity in Chinese patients with Graves’ ophthalmopathy. East Asian Arch Psychiatry 2013;23:6-12.
- Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S208-28.
- Perruccio AV, Stefan Lohmander L, Canizares M, Tennant A, Hawker GA, Conaghan PG, et al. The development of a short measure of physical function for knee OA KOOS-Physical Function Shortform (KOOS-PS) — an OARSI/OMERACT initiative. Osteoarthritis Cartilage 2008;16:542-50.
- Xie F, Li SC, Roos EM, Fong KY, Lo NN, Yeo SJ, et al. Cross-cultural adaptation and validation of Singapore English and Chinese versions of the Knee injury and Osteoarthritis Outcome Score (KOOS) in Asians with knee osteoarthritis in Singapore. Osteoarthritis Cartilage 2006;14:1098-103.
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson A. Studies with pain rating scales. Ann Rheum Dis 1978;37:378-81.
- Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S240-52.
- Joyce CR, Zutshi DW, Hrubes V, Mason RM. Comparison of fixed interval and visual analogue scales for rating chronic pain. Eur J Clin Pharmacol 1975;8:415-20.
- Felson DT, Nevitt MC. The effects of estrogen on osteoarthritis. Curr Opin Rheumatol 1998;10:269-72.
- Patten SB, Beck CA, Kassam A, Williams JV, Barbui C, Metz LM. Long-term medical conditions and major depression: strength of association for specific conditions in the general population. Can J Psychiatry 2005;50:195-202.
- van’t Land H, Verdurmen J, Ten Have M, van Dorsselaer S, Beekman A, de Graaf R. The association between arthritis and psychiatric disorders; results from a longitudinal population-based study. J Psychosom Res 2010;68:187-93.
- Fuller-Thomson E, Shaked Y. Factors associated with depression and suicidal ideation among individuals with arthritis or rheumatism: findings from a representative community survey. Arthritis Rheum 2009;61:944-50.
- Teesson M, Mitchell PB, Deady M, Memedovic S, Slade T, Baillie A. Affective and anxiety disorders and their relationship with chronic physical conditions in Australia: findings of the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 2011;45:939- 46.
- Blixen CE, Kippes C. Depression, social support, and quality of life in older adults with osteoarthritis. Image J Nurs Sch 1999;31:221-6.
- Sherman AM. Social relations and depressive symptoms in older adults with knee osteoarthritis. Soc Sci Med 2003;56:247-57.
- Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G. Predictors of depression in a sample of 1,021 primary care patients with osteoarthritis. Arthritis Rheum 2007;57:415-22.
- Gleicher Y, Croxford R, Hochman J, Hawker G. A prospective study of mental health care for comorbid depressed mood in older adults with painful osteoarthritis. BMC Psychiatry 2011;11:147.
- Cairney J, Corna LM, Veldhuizen S, Herrmann N, Streiner DL. Comorbid depression and anxiety in later life: patterns of association, subjective well-being, and impairment. Am J Geriatr Psychiatry 2008;16:201-8.
- Almeida OP, Draper B, Pirkis J, Snowdon J, Lautenschlager NT, Byrne G, et al. Anxiety, depression, and comorbid anxiety and depression: risk factors and outcome over two years. Int Psychogeriatr 2012;24:1622- 32.
- Chan H, Yu CS, Li SY. Psychiatric morbidity in Chinese patients with chronic hepatitis B infection in a local infectious disease clinic. East Asian Arch Psychiatry 2012;22:160-8.
- Ho HY. Psychiatric morbidity in Chinese renal transplant recipients. The Hong Kong College of Psychiatrists; 2011.
- Berkman LF. The role of social relations in health promotion. Psychosom Med 1995;57:245-54.
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med 2000;51:843- 57.
- Ethgen O, Vanparijs P, Delhalle S, Rosant S, Bruyère O, Reginster JY. Social support and health-related quality of life in hip and knee osteoarthritis. Qual Life Res 2004;13:321-30.
- Weinberger M, Tierney WM, Booher P, Hiner SL. Social support, stress and functional status in patients with osteoarthritis. Soc Sci Med 1990;30:503-8.
- Chi I, Yip PS, Chiu HF, Chou KL, Chan KS, Kwan CW, et al. Prevalence of depression and its correlates in Hong Kong’s Chinese older adults. Am J Geriatr Psychiatry 2005;13:409-16.
- Riddle DL, Wade JB, Jiranek WA. Major depression, generalized anxiety disorder, and panic disorder in patients scheduled for knee arthroplasty. J Arthroplasty 2010;25:581-8.
- Dunlop DD, Lyons JS, Manheim LM, Song J, Chang RW. Arthritis and heart disease as risk factors for major depression: the role of functional limitation. Med Care 2004;42:502-11.
- Stang PE, Brandenburg NA, Lane MC, Merikangas KR, Von Korff MR, Kessler RC. Mental and physical comorbid conditions and days in role among persons with arthritis. Psychosom Med 2006;68:152-8.
- Okoro CA, Strine TW, Balluz LS, Crews JE, Dhingra S, Berry JT, et al. Serious psychological distress among adults with and without disabilities. Int J Public Health 2009;54 Suppl 1:52-60.
- Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum 2003;48:3359-70.
- Lin EH, Katon W, Von Korff M, Tang L, Williams JW Jr, Kroenke K, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA 2003;290:2428-9.
- Ericsson M, Poston WS, Linder J, Taylor JE, Haddock CK, Foreyt JP. Depression predicts disability in long-term chronic pain patients. Disabil Rehabil 2002;24:334-40.
- Hawker GA, Gignac MA, Badley E, Davis AM, French MR, Li Y, et al. A longitudinal study to explain the pain-depression link in older adults with osteoarthritis. Arthritis Care Res (Hoboken) 2011;63:1382-90.
- Scopaz KA, Piva SR, Wisniewski S, Fitzgerald GK. Relationships of fear, anxiety, and depression with physical function in patients with knee osteoarthritis. Arch Phys Med Rehabil 2009;90:1866-73.
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry 2001;9:113-35.
- Yuen WH. Osteoarthritis of knees: the disease burden in Hong Kong and means to alleviate it. Hong Kong Med J 2014;20:5-6.
- Unützer J, Hantke M, Powers D, Higa L, Lin E, D Vannoy S, et al. Care management for depression and osteoarthritis pain in older primary care patients: a pilot study. Int J Geriatr Psychiatry 2008;23:1166-71.