Hong Kong J Psychiatry 2006;16:92-100
Original Article
Efficacy of a Brief Intervention for Carers of People with First-episode Psychosis: a Waiting List Controlled Study
介入治療對照顧恩覺失調患者人士的效用:等候名單對照研究
HW So, EYH Chen, RCK Chan, CW Wong, SF Hung, DWS Chung, SM Ng, CLW Chan
蘇可蔚、陳友凱、陳楚僑、黃幟榮、熊思方、鍾維壽、吳少文、陳麗雲
Ms HW So, MA, MSSc, Kwai Chung Hospital, Hong Kong, China.
Dr EYH Chen, MBChB, MA, MD, MRCPsych, FHKAM (Psychiatry), Department of Psychiatry, The University of Hong Kong, Hong Kong, China. Dr RCK Chan, PhD, Institute of Psychology, Chinese Academy of Sciences, Beijing, China.
Dr CW Wong, PsychD, Kwai Chung Hospital, Hong Kong, China.
Dr SF Hung, FRCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong, China.
Dr DWS Chung, MBChB, MSocSc, MRCPsy, Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong, China.
Dr SM Ng, BHSc, MSc, Centre on Behavioral Health, The University of Hong Kong, Hong Kong, China.
Dr CLW Chan, PhD, Centre on Behavioral Health, The University of Hong Kong, Hong Kong, China.
Tel: (852) 2959 8191; Fax: (852) 2371 3197; E-mail: shw661@ha.org.hk
Submitted: 27 December 2006; Accepted: 3 January 2007
Abstract
Objective: While family psycho-education for schizophrenia is well-supported, the efficacy of family intervention for first-episode psychosis is less studied. This waiting list controlled study set out to evaluate the effectiveness of a 6-week intervention for carers of people with first-episode psychosis.
Participants and Methods: Carers were randomised into experimental or waiting list categories. Study 1 compared various outcome measures in the 2 categories. Study 2 evaluated the treatment effects.
Results: After the intervention, carers showed increased knowledge about psychosis and a reduction in negative ways of coping. The improvement in knowledge was maintained at 6-month follow-up, and trends towards improved caregiving burden and coping were also evident.
Conclusion: A brief intervention programme can be effective in improving important variables such as knowledge, coping, and caregiving burden. The implications for selecting ‘core components’ for an effective intervention were discussed.
Key words: Caregivers; Group psychotherapy; Psychological adaptation; Psychotic disorders
摘要
目的:儘管醫學界一直認同以家庭心理教育治療精神分裂,但有關家庭介入治療首發思覺失調的研究則不多。這項等候名單對照研究描述並評估對照顧首發思覺失調患者人員進行6周介入治療的效率。
參與者與方法:照顧者按隨機分為實驗組或等侯名單組。研究包括兩部分: 比較兩組的結果測量,以及評估治療效果。
結果:照顧者接受介入治療後增進對恩覺失調的認識且減低有關適應能力的負面想法。在知識改善方面於6個月隨訪期後仍然持續,也顯示他們照顧負擔及應付方面的正性傾向。
結論:短時間的介入治療計創能有效改善盡重要變數,包括知識、適應力和照顧負擔。研究也對選擇有效治療的核心元素作出討論。
關鍵詞:照顧者、小組精神治療、心理適應力、思覺失總
Introduction
Family psycho-education has become fundamental in the management of patients experiencing mental illness.1-4 The literature to date suggests that meeting the needs of family members dramatically improves patient outcomes and family well-being.5
McFarlane et al5 reviewed research conducted in the last decade, which included family psycho-education as a form of evidence-based practice. Family psycho-education includes many cognitive, behavioural, and supportive therapeutic elements, and often utilises a consultative framework, whilst sharing key characteristics with other types of family interventions.5
Various approaches to family psycho-education have been developed and studied. One of the most-researched is the psycho-educational multiple family group,6 which consists of 3 phases: joining in a collaborative alliance with family members; gradually increasing community functioning of the patient; and establishing an ongoing social network.7 Other evidence-based family intervention models include behavioural family management,8 family psycho-education,9 and resorting to relative groups.10,11
These interventions usually involve intensive sessions over a period of months to years. Solomon et al4,12 compared 2 short-term models involving family intervention, but found that favourable outcomes were only modest for the carers and questionable for the patients.
The small number of randomised studies suggests that brief interventions are ineffective in improving carer distress, burden or poor coping,12-15 while long-term psycho- educational interventions are more successful.16 Other reviews also suggested that long-term interventions (up to 9 months) are more effective than shorter-term treatments (up to 3 months).17,18 However, the number of sessions might not completely explain the differences in outcomes. Length of total time, allowing for refinement of coping skills and strategies by the family and patient, rather than the number of sessions, may be a factor. Also, brief interventions tend to be focused on information presentation, without also providing family members with skills training, ongoing guidance regarding illness management, and emotional support.19 The latter are all core elements for effective psycho-educational interventions.5 Therefore, delivery of the appropriate components of family psycho-education to families appears to be important in determinant of outcomes for both families and patients.
While the efficacy of family intervention in schizophrenia is well-established, the type of family intervention best suited in first-episode psychosis is less apparent. The issues facing first-episode patients are different from those facing the chronically ill and their relatives.18,20 Addington and Gleeson21 identified the following explicit goals in working with first-episode families: (1) to maximise the adaptive functioning of the family; (2) to minimise disruption to family life caused by the first episode; (3) to minimise the risk of long-term grief, stress and burden experienced by the family; and (4) to aid the family in understanding the impact of psychosis on the family system, individual family members and the interaction between them and the course of the psychosis. Linszen et al18 suggested that the intervention needs to be refined and selective, and that comprehensive family interventions may be inappropriate. Rather, they advocated brief educational programmes focusing on problem-solving and relapse prevention as highly suitable for first-episode psychosis afflicted families.
Addington et al22 reported the 3-year outcome of a family intervention that was an integral component of an early psychosis management programme. They found improved psychological well-being and experience of caregiving after 1 to 3 years of family intervention. The Early Psychosis Prevention and Intervention Centre23 adopted a brief programme, which, in 4 sessions, explored the definitions of mental illness, explored possible causes of mental illness through the stress vulnerability model, and described treatment options based on mental illness using biopsychosocial models. Strategies for relapse prevention and early warning identification signs, monitoring and response plans were also included.23-25
The aim of the present study was to evaluate the effectiveness of a 6-session psycho-educational intervention for carers of patients with first-episode psychosis, and involved measuring the changes in the participants’ knowledge of psychosis, caring burden, coping, and expressed emotions.26
Methods
Subjects and Methods
Participants were recruited from the Early Assessment Service for Young People with Psychosis (EASY) in Hong Kong, which was an early intervention project for patients with first- episode psychosis aged 15-25 years.27 Relatives were recruited into the study if: (1) they had a family member suffering from the first episode of a psychotic disorder (schizophrenia, schizoaffective, or schizophreniform disorder) according to the criteria of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems28; (2) they were the major carers of the patient, as identified by both patient and the carer; (3) they were living with the patient at the time of recruitment; and (4) they gave written informed consent to participate in the study. Relatives were not recruited if they were actively receiving psychiatric services or if the patient was receiving inpatient treatment.
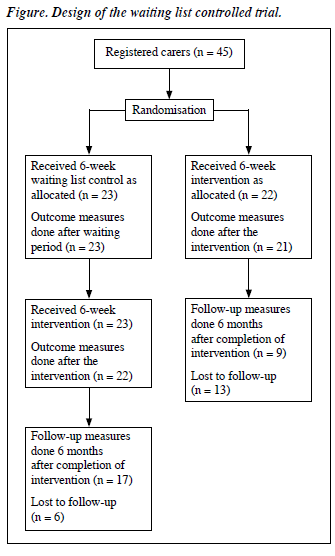
All 45 carers fulfilling the above criteria were recruited from 3 study sites (Kwai Chung Hospital, Prince of Wales Hospital, and Queen Mary Hospital). Recruitment and randomisation took place between 6 and 12 months after the index patient’s entry into the EASY service, when their psychotic symptoms were generally stabilised with medication. With the patient’s permission, each carer was contacted to discuss details of the study. Following baseline (pre-intervention) assessment, the carers were randomly assigned by a computer to an active intervention or waiting list (control) group, as shown in the Figure.
All corresponding carers’ patients were treated with antipsychotic medication, and efforts were made to ensure that their regular medical service was unaffected.
Active Intervention
Active intervention for carers of patients with first-episode psychosis took place at Kwai Chung Hospital (n = 29), Queen Mary Hospital (n = 7), and a youth centre (n = 9) 1 evening per week for a period of 6 weeks. Each session lasted approximately 1.5 hours. Participants were divided into 8 groups of 4 to 8 each. A Masters level psychologist ran the sessions under the supervision of the first author. The group therapist initiated phone engagements with the carers before the first session, facilitated group discussions, and contacted the carers when they missed a session. The patients were not contacted except for the purpose of outcome assessment.
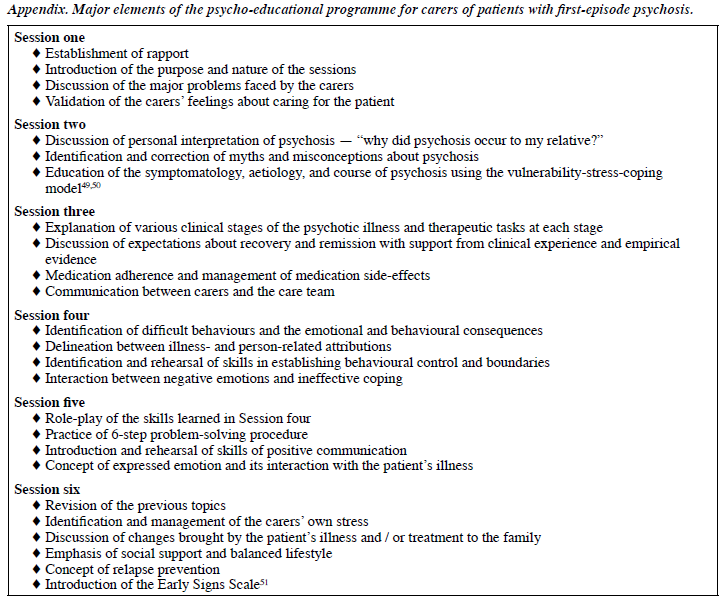
The first 3 active intervention sessions were organised to consolidate the carers’ knowledge about psychosis, whereas the last 3 were aimed at enhancing their skills in handling the patients’ illness and their own caregiving stress. Major components in the 6 sessions entailed education on early psychosis and its treatment, handling difficult behaviours, stress management, communication skills, and relapse prevention. The Appendix provides a brief description of the intervention programme and a detailed protocol is available from the first author.
Attempts were made to balance content delivery with support and experience sharing; open discussion and questions were encouraged. Each session began with a few minutes of socialising and a brief review on the week’s events, or on the progress of assignments set in the last session. Participants were also encouraged to ask questions and make suggestions regarding topics for discussion. A 15- minute break was introduced in the middle of each session. Such breaks were of significant value in encouraging more interpersonal interaction among the participants.
By protocol, carers in the study were not given any intensive individual or family psychotherapy other than to those assigned to the active intervention. Only continued engagement with the patient’s case manager (usually a psychiatric nurse or medical social worker) was provided. All the case managers were briefed about those receiving active intervention beforehand and agreed to adhere to the same case management package that they usually used, whether or not the carers were recruited into the study.
Control Condition
A 6-week period, whilst patients were on the waiting list served as the control condition, whereby the carers received nothing more than continued engagement and needs-based counselling with each patient’s case manager. The case management package for the control period was available from the first author. Although case managers answered questions about individual patient illnesses and recovery, they did not provide systematic psycho-education as in the intervention group. Also, there was no active participation by the carers, by way of completion of required homework assignments. Since the participation in a group was believed to have therapeutic benefits over and above usual treatment, for ethical reasons after the 6 weeks of waiting period (control) treatment, carers were also provided an identical group intervention by the same therapist.
Outcome Measurements
Major outcome measures were: carers’ knowledge about psychosis, caregiving experience, coping style, and expressed emotion. Associated measures included carers’ general health and stressful life events.
Except for the Positive and Negative Syndrome Scale (PANSS), all measures were administered at baseline, after their group therapy sessions (6 weeks), and 6 months after completion of the session. Carers acting as waiting list controls had additional measurements 6 weeks after the baseline measurement. Most outcome measures were self-administered by the carers, except for the Level of Expressed Emotion (LEE) which was self-administered by the patients. The major outcome measures for this study are described below.
Knowledge about psychosis scale (available from the first author) was an ad-hoc measure developed by the researchers. The scale comprised 19 fill-in-the-blank and 5 dichotomous forced-choice items. It targeted illness-related topics covered in the active intervention programme,
namely psychopathology, aetiology, treatment, and illness management. A pilot study conducted with a sample of 203 patients with first-episode psychosis showed that the scale had fair internal consistency with an overall alpha of 0.67 and 0.72 for the fill-in-the-blank and dichotomous items, respectively. Participants in the present study also showed a high internal consistency, with an overall alpha of 0.79, and the frequency plot of all items showed a normal distribution.
The Experience of Caregiving Inventory (ECI) was a self-reported measure of the experience of caring for a mentally ill person,29 conceived as a measure of appraisal. It comprised 10 subscales, 8 negative (difficult behaviours; negative symptoms; stigma; problems with services; effects on family; need to backup; dependency; sense of loss) and 2 positive (rewarding personal experiences; good aspects of the relationship with the patient), derived from 66 items. Each subscore indicated the extent that the respondent was concerned about that respective area of caregiving; total scores could range from 0 to 264.
The Chinese Ways of Coping Questionnaire30 (CWCQ) was a 16-item scale designed to measure coping activities among Chinese students and adults, and was reduced from its original 66-item version.31 This new version included 4 subscales: rational problem-solving; resigned distancing; seeking support and ventilation; and passive wishful thinking. Each subscore reflected the extent to which the respondents used to cope with events in daily living. The potential score for each subscale ranged from 0 to 12. Chan30 reported on the internal consistency of the CWCQ, with an alpha of 0.62 for resigned distancing and alphas ranging from 0.70 to 0.74 for the other 3 subscales. In this study, participants were asked to respond to the CWCQ in the context of coping with their child’s psychotic illness.
The LEE32 scale was a self-reporting measure of the perceived emotional climate in a person’s influential relationships. The scale was constructed on the basis of a conceptual framework described by expressed emotion theorists. In addition to providing an overall score, the 60- item scale assessed the following 4 characteristic attitudes or response styles of significant others: intrusiveness, emotional response, attitude toward illness, and tolerance / expectations. The potential score ranged from 0 to 60. Cole and Kazarian32 reported excellent internal consistency, with a KR-20 coefficient for the overall scale of 0.95; for the subscales they ranged from 0.84 to 0.89. Stability for the overall scale was also high, with a 6-week test-retest correlation on a subsample of 0.82.
To control for other variables that may account for the changes observed, the following measures were also included.
The General Health Questionnaire (GHQ)-12 is one of the most widely used screening instruments covering a range of psychiatric symptoms – anxiety, depression, somatic, and social dysfunction. Several versions of the GHQ have been developed, including 60-, 30-, 28-, and 12-item scales. The GHQ-1233 is the most commonly used version, because of its brevity and the availability of normative data.34-36 The GHQ scoring method was used. Potential scores ranged from 0 to 48.
The Life Events Questionnaire37 focused on 12 categories of common life events that are highly likely to be threatening (e.g. bereavement or being sacked from a job). The respondents were asked to indicate whether any of such events impinged on them in the past month.
The PANSS38 was one of the most widely used screening instruments for assessment of positive and negative psychotic symptoms. The scale has a total score and 4 subscores: positive subscale, negative subscale, general subscale, and aggressiveness subscale, and was administered by the patient’s treating psychiatrist on a regular basis.
Statistical Analysis
All analyses of the quantitative data were conducted using the Statistical Package for the Social Sciences version 11.0. In Study 1, the treatment effect of the intervention group was compared with the waiting list participants (controls). Differences in scores before and after the active and control interventions were computed for continuous variable outcomes, and the association to treatment allocation was analysed by the independent samples t test, whenever assumptions of normality and homogeneity of variances were acceptable. In Study 2, data in the 2 allocation groups were combined to evaluate the effect of the intervention programme on outcome measures pre-intervention, post- intervention, and at the 6-month follow-up, using a one-way analysis. The level of statistical significance was chosen as p < 0.05.
Results
The socio-demographic characteristics of the carers are displayed in Table 1. There were no statistically significant differences in socio-demographic characteristics between allocation groups or study sites, both for carers and patients. Patients’ baseline measure on PANSS (mean [SD], 52.90 [22.13]) and duration of untreated psychosis (mean [SD] number of days, 181.13 [191.42]) also showed no difference between the allocation groups.
There were similar high attendance rates for the active and control intervention groups; the mean (SD) percentage of attendance being 87.0 (13.5) and 88.0 (13.8), respectively. There was no significant difference between the groups with respect to the number of life events reported and total scores on the GHQ.
Study 1: Intervention Group Versus Waiting List Control
Table 2 summarises the findings for major and associated outcome variables. Carers receiving the active intervention displayed a statistically significant increase (p = 0.01) in knowledge about psychosis after the intervention, a significant decrease in the total scale score (p = 0.004) and in 3 of the 4 subscales of the CWCQ (rational problem- solving, resigned distancing, and passive wishful thinking; p < 0.05). There were no significant differences in the ECI or LEE between the groups.
Study 2: Analyses of Intervention Effects after Combining Data from the Two Allocation Groups
By protocol, the same intervention was conducted
(eventually at least) by the same therapist for all carers in this study, regardless of their allocation group (Table 1). There was no significant difference between the 2 allocation groups in terms of socio-demographic characteristics. The treatment effects in the active intervention groups were not significantly different from those in the controls. Since the 2 groups were matched for both socio-demographic characteristics and trends of treatment effects, we pooled the data from the 2 allocation groups to obtain a larger sample size.
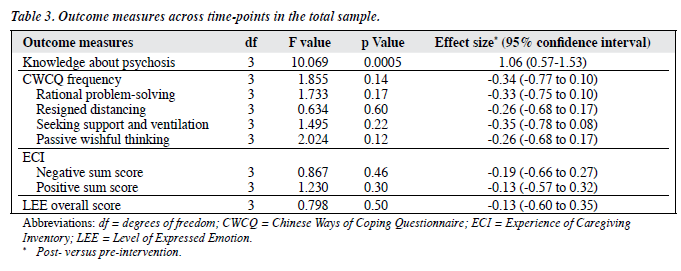
Table 3 shows results of the analysis of variance comparing outcome measures at pre-intervention, post- intervention, and at 6-month follow-up. It shows a signifi- cant change in knowledge about psychosis (p = 0.0005). Post- hoc tests showed that there was a significant increase in know- ledge about psychosis between pre- and post-intervention measurements (mean difference, 4.47; p = 0.0005), which was maintained at the 6-month follow-up (mean difference between post-intervention and follow-up measurement, 0.10; p = 0.93). The effect size of the post-intervention decreases in the CWCQ scores was mild to moderate, and did not attain statistical significance.
Changes in ECI subscores of negative symptoms (p = 0.08) and dependency (p = 0.09) showed trends towards statistical significance. Post-hoc tests revealed that there was a significant decrease in the subscore for negative symptoms between the pre-intervention and follow-up measurements (mean difference, 2.83; p = 0.02). Such decreases continued well after the intervention at the follow-up measurement (mean difference, 2.97; p = 0.02). Subscore dependency decreased significantly between the pre-intervention and follow-up measurements (mean difference, 2.04; p = 0.02).
Discussion
Carer Outcomes
The results of this waiting list controlled trial suggest that the psycho-educational programme significantly improved carers’ knowledge about psychosis, over and above the waiting list controls in receipt of usual psycho-education. The effect was maintained for at least 6 months. This is an important finding, because increased knowledge of the illness and treatment enables the patients and relatives to use the mental health care system more effectively.39
The results also suggest that the frequency of coping methods used decreased after the active intervention, most markedly in the subscales of negative coping (resigned distancing and passive wishful thinking). However, a decrease in rational problem-solving was also noted, which may be due to a general decrease in the number of coping strategies adopted when the carers became more knowledgeable about the illness. Post-hoc correlation analysis showed that passive wishful thinking was most markedly reduced among carers of patients with milder baseline psychopathology. This finding is not consistent with other similar studies,12,14,15,19 which suggested that brief interventions are ineffective in improving carer distress, burden or poor coping.
The only statistically significant post-intervention change in the ECI scale was the reduced subscore for problems with services, especially among carers of patients with less severe baseline psychopathology. Carers with the greater reductions in perceived burden about problems with services also had greater reductions in the CWCQ subscore for resigned distancing. This implies that active intervention reduced the participants’ distress about relating to services and increased their initiative for help-seeking, although such change was not maintained after 6 months. Further studies using behavioural measures of help-seeking may be needed to test this hypothesis. Significant reductions in the ECI subscores for negative symptoms and dependency were found, yet such changes took place relatively slowly and suggested a continuous decrease between the pre- intervention and follow-up assessments. Possibly the core skills taught in treatment may be consolidated over time in the absence of ongoing therapy, but could also be attributable to the natural course of recovery from the psychotic illness.
There was no statistically significant active intervention–associated change in the perceived expressed emotion reported by patients. The reason could be that the duration of the intervention was insufficient for marked changes in emotional relations. In a meta-analysis of family interventions, Mari and Streiner40 only found marginally significant changes in expressed emotion status in spite of reductions of relapse. This indicates that expressed emotion in relatives of patients with psychosis can be difficult to influence, even by more comprehensive interventions. Besides, in this study the findings of expressed emotion could also have been limited by the use of a rather brief measurement tool.
Methodological Issues and Clinical Implications
The 6-week intervention programme under study met carers’ phase-specific needs by providing information about first-episode psychosis and promoting interpersonal support. The comparable effectiveness of this study, albeit briefer than studies of similar design, may shed light on the inclusion of ‘core components’ in a cost-effective psycho- educational programme for carers of patients with first- episode psychosis. The clinical components included in this intervention programme (education, coping and problem- solving, behavioural skills training, stress management, and communication enhancement) were chosen based on the evidence from previous studies.5 Limited by the rather small sample size, this study could only show benefit to carers of patients with first-episode psychosis by combination of clinical components. Further studies with a larger sample size may show more specific associations between each treatment component and specific outcome measures.
This intervention programme appeared to confer improvements over and above those accruing in waiting list controls (i.e. engagement and psycho-education). This indicates the importance of having a group that allows the carers to have access to each other, to learn of other families’ successes and failures, and to solicit emotional and social support. Since participants were allowed to make suggestions about topics for discussion, adaptations for culture-specific issues were flexibly incorporated into the programme. However, generalisability of the results may be limited by having only 1 therapist and lack of ongoing measurements of the patients’ symptomatic and clinical recovery. As in other treatment studies, potential impact from non-specific treatment effects must be carefully considered before interpreting the results.
Given that unselected carers were recruited under the usual circumstances of a service setting, this study had a relatively high attendance rate. This was not consistent with findings of other studies showing high dropout rates and difficulty in engagement.41,42 This difference could be attributed to the lower demand for time commitment in this study, as well as the therapist’s follow-up of absentees. Whenever therapists no longer contacted participants, a significant percentage of participants were lost to follow-up within months. However, sample selectivity of this study was limited, as the rate of carers refusing to participate was not reported.
While other investigations to date mostly measured outcomes reported by carers, this study included patients’ reports in the measurement of expressed emotion. This is purported to provide additional collateral information. While the importance of reducing expressed emotion is well- established in studies on chronic schizophrenia, it may be of less significance in first-episode psychosis. Studies have shown that expressed emotion changes over time and can be affected by the patient’s course of illness. The latter often waxes and wanes in the early phase of psychosis.43-45 Besides, recent studies argue that elements that focus on problem- solving, anxiety management, coping and communication skills training, and enhanced social networks and support may be more directly associated with relapse prevention than reductions in expressed emotion.46-48 Findings in these investigations as well as the current study indicate that important therapeutic goals may be achieved by following the professionally led intensive intervention programme by consumer-led self-help groups. Moreover, they extend social support without impinging on already limited clinical resources.
Shorter psycho-educational programmes for relatives are important to evaluate because comprehensive family interventions are impossible to implement in all psychiatric services. Furthermore, decisions regarding the optimal content, intensity and duration of these interventions could make for more specific and effective psycho-education interventions. The present study suggests that a short psycho-educational programme for carers of patients with first-episode psychosis increases and maintains knowledge about psychosis for as long as 6 months. It also brings about some short-term improvements in coping and the caregiving burdens.
Acknowledgements
The authors are grateful to the patients and carers who participated in the study, to the Stewards who provided the venue and also to Miss Joanne Yip who conducted the intervention group. The research was funded by the Centre on Behavioral Health, the University of Hong Kong.
References
- Barrowclough C, Tarrier N. ‘Psychosocial’ interventions with families and their effects on the course of schizophrenia: a review. Psychol Med 1984;14:629-42.
- Fung C, Fry A. The role of community mental health nurses in educating clients and families about schizophrenia. Aust N Z J Ment Health Nurs 1999;8:162-75.
- Glick ID, Burti L, Okonogi K, Sacks M. Effectiveness in psychiatric care. III: Psychoeducation and outcome patients with major affective disorder and their families. Br J Psychiatry 1994;164:104-6.
- Solomon P, Draine J, Mannion E, Miesel M. Impact of brief family psychoeducation on self-efficacy. Schizophr Bull 1996;22:41-50.
- McFarlane WR, Dixon L, Lukens E, Lucksted A. Family psychoeducation and schizophrenia: a review of the literature. J Marital Fam Ther 2003;29:223-45.
- McFarlane WR. Multiple family groups in the treatment of schizophrenia. In Nasrallah HA, editor, Handbook of Schizophrenia. Vol. 4. Amsterdam: Elsevier; 1990:167-89.
- McFarlane WR. The multifamily group. New York: Oxford University Press; 2000.
- Falloon I, Boyd J, McGill C. Family care of schizophrenia. New York: Guilford; 1984.
- Anderson CM, Hogarty GE, Reiss DJ. Family treatment of adult schizophrenic patients: a psycho-educational approach. Schizophr Bull 1980;6:490-505.
- Leff J, Berkowitz R, Shavit N, Strachan A, Glass I, Vaughn C. A trial of family therapy v. a relatives group for schizophrenia. Br J Psychiatry 1989;154:58-66.
- Leff J, Kuipers L, Berkowitz R, Sturgeon D. A controlled trial of social intervention in the families of schizophrenic patients: two year follow- up. Br J Psychiatry 1985;146:594-600.
- Solomon P, Draine J, Mannion E, Meisel M. Effectiveness of two models of brief family education: retention of gains by family members of adults with serious mental illness. Am J Orthopsychiatry 1997;67:177-86.
- Cozolino LJ, Goldstein MJ, Nuechterlein KH, West KL, Snyder KS. The impact of education about schizophrenia on relatives varying in expressed emotion. Schizophr Bull 1988;14:675-87.
- Posner CM, Wilson KG, Kral MJ, Lander S, McIlwraith RD. Family psychoeducational support groups in schizophrenia. Am J Orthopsychiatry 1992;62:206-18.
- Szmukler GI, Herrman H, Colusa S, Benson A, Bloch S. A controlled trial of a counselling intervention for caregivers of relatives with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 1996;31:149-55.
- Carpentier N, Lesage A, Goulet J, Lalonde P, Renaud M. Burden of care of families not living with young schizophrenic relatives. Hosp Community Psychiatry 1992;43:38-43.
- Bustillo JR, Lauriello J, Horan W, Keith S. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry 2001;158:163-75.
- Linszen D, Dingemans P, Van der Does JW, Nugter A, Scholte P, Lenior R, et al. Treatment, expressed emotion and relapse in recent onset schizophrenic disorders. Psychol Med 1996;26:333-42.
- Cuijpers P. The effects of family interventions on relatives’ burden: a meta-analysis. J Ment Health 1999;8:275-85.
- Goldstein MJ. Psychoeducation and family treatment related to the phase of a psychotic disorder. Conference Proceedings. Denmark 1996:1-4.
- Addington J, Gleeson J. Family intervention in early psychosis. In McGorry PD, Jackson HJ, editors. The recognition and management of early psychosis. Cambridge, UK: Cambridge University Press; 2003:367-406.
- Addington J, McCleery A, Addington D. Three-year outcome of family work in an early psychosis program. Schizophr Res 2005;79:107-16.
- EPPIC (Early Psychosis Prevention and Intervention Centre). Psychoeducation in early psychosis. Melbourne: Psychiatric Services Branch, Department of Human Services; 1997.
- Edwards J, Francey SM, McGorry PD, Jackson H. Early psychosis prevention and intervention: evolution of a comprehensive community- based specialist service. Behav Change 1994;11:223-33.
- McGorry PD. Psychoeducation in first-episode psychosis: a therapeutic process. Psychiatry 1995;58:313-28.
- Leff J, Vaughn CE. Expressed emotion in families. New York: Guilford; 1985.
- Chen EY. Developing an early intervention service in Hong Kong. In: Ehmann T, MacEwan GW, Honer WG, editors. Best care in early psychosis intervention: global perspective. Oxford: Taylor & Francis; 2004:125-30.
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders. Geneva: World Health Organization; 1992.
- Szmukler GI, Burgess P, Herrman H, Benson A, Colusa S, Bloch S. Caring for relatives with serious mental illness: the development of the Experience of Caregiving Inventory. Soc Psychiatry Psychiatr Epidemiol 1996;31:137-48.
- Chan DW. Stress, coping strategies, and psychological distress among secondary school teachers in Hong Kong. Am Educ Res J 1998;35:145- 63.
- Folkman S, Lazarus RS. Manual for the ways of coping questionnaire. Palo Alto, California: Consulting Psychologist Press; 1988.
- Cole JD, Kazarian SS. The Level of Expressed Emotion Scale: a new measure of expressed emotion. J Clin Psychol 1988;44:392-7.
- Goldberg D, Williams P. A user’s guide to the general health questionnaire. Windsor: NFER-Nelson; 1991.
- Banks MH. Validation of the General Health Questionnaire in a young community sample. Psychol Med 1983;13:349-53.
- 35. Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27:191- 7.
- Winefield HR, Goldney RD, Winefield AH, Tiggemann M. The General Health Questionnaire: reliability and validity for Australian youth. Aust N Z J Psychiatry 1989;23:53-8.
- Brugha TS, Cragg D. The List of Threatening Experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand 1990;82:77-81.
- Kay S, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76.
- Falvo DR. Effective patient education: a guide to increased compliance. Gaithersburg: Aspen; 1994.
- Mari JJ, Streiner DL. An overview of family interventions and relapse on schizophrenia: meta-analysis of research findings. Psychol Med 1994;24:565-78.
- Barrowclough C, Tarrier N, Lewis S, Sellwood W, Mainwaring J, Quinn J, et al. Randomised controlled effectiveness trial of a needs- based psychosocial intervention service for carers of people with schizophrenia. Br J Psychiatry 1999;174:505-11.
- Szmukler G, Kuipers E, Joyce J, Harris T, Leese M, Maphosa W, et al. An exploratory randomised controlled trial of a support programme for carers of patients with a psychosis. Soc Psychiatry Psychiatr Epidemiol 2003;38:411-8.
- Jarbin H, Gråwe RW, Hansson K. Expressed emotion and prediction of relapse in adolescents with psychotic disorders. Nord J Psychiatry 2000;54:201-5.
- Patterson P, Birchwood M, Cochrane R. Preventing the entrenchment of high expressed emotion in first episode psychosis: early developmental attachment pathways. Aust N Z J Psychiatry 2000;34 Suppl:S191- 197.
- Stirling J, Tantam D, Thomas P, Newby D, Montague L, Ring N, et al. Expressed emotion and schizophrenia: the ontology of EE during an 18-month follow-up. Psychol Med 1993;23:771-8.
- Dyck DG, Hendryx MS, Short RA, Voss WD, McFarlane WR. Service use among patients with schizophrenia in psychoeducational multiple- family group treatment. Psychiatr Serv 2002;53:749-54.
- McFarlane WR, Dushay RA, Stastny P, Deakins SM, Link B. A comparison of two levels of family-aided assertive community treatment. Psychiatr Serv 1996;47:744-50.
- McFarlane WR, Dushay RA, Deakins SM, Stastny P, Lukens EP, Toran J, et al. Employment outcomes in family-aided assertive community treatment. Am J Orthopsychiatry 2000;70:203-14.
- Nuechterlein KH, Dawson ME. A heuristic vulnerability/stress model of schizophrenic episodes. Schizophr Bull 1984;10:300-12.
- Zubin J, Spring B. Vulnerability – a new view of schizophrenia. J Abnorm Psychol 1977;86:103-26.
- Birchwood M, Smith J, Macmillan F, Hogg B, Prasad R, Harvey C, et al. Predicting relapse in schizophrenia: the development and implementation of an early signs monitoring system using patients and families as observers, a preliminary investigation. Psychol Med 1989;19:649-56.