Hong Kong J Psychiatry 2006;16:109-16
Original Article
Characteristics and Outcome Predictors of Conditionally Discharged Mental Patients in Hong Kong
有條件釋放下出院的香港精神病患者的特徵及入院因素
YC Wong, DWS Chung
黃業就、鍾維壽
Dr YC Wong, MBBS, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, Tai Po Hospital, Tai Po, New Territories, Hong Kong, China.
Dr DWS Chung, MB ChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, Tai Po Hospital, Tai Po, New Territories, Hong Kong, China.
Hospital, Tai Po, New Territories, Hong Kong, China. Tel: (852) 2689 2000; Fax: (852) 2667 6353;
E-mail: edmycwong2@yahoo.com.hk
Submitted: 20 December 2006; Accepted: 22 February 2007
Abstract
Objective: To explore the characteristics and short-term outcomes of mentally ill patients conditionally discharged in Hong Kong and identify factors associated with the risks of readmission 1 year after the first conditional discharge.
Participants and Methods:A retrospective case notes review was undertaken. Subjects included all adult patients first conditionally discharged before 31 August 2005 and currently under the care of the psychiatric service of the New Territories East Cluster of Hong Kong. Socio-demographic data, clinical variables and outcomes during the first year after conditional discharge were retrieved. A comparison between patients with or without readmission was made using univariate and logistic regression analyses in order to identify risk factors associated with readmission.
Results: A total of 140 subjects were included. The subjects were characterised by diagnoses of psychotic disorders, poor compliance with treatment, and a history of committing psychotically based serious dangerous acts in the recent past. In the first year after conditional discharge, 10% displayed violent behaviour, about 5% had forensic contacts, and 1% attempted suicide or deliberate self-harm. One-fourth of subjects were readmitted. Factors associated with readmission were prior psychiatric admissions, younger age on index date, persistent substance misuse, and being brought up in the care of the social welfare department.
Conclusion:Most subjects did not display violent behaviour 1 year after conditional discharge. The identification of avoidable risk factors for readmission such as persistent substance misuse sheds light on possible ways to enhance community aftercare. The results provide useful information for clinical practice, service provision, and future research.
Key words: Forecasting; Mentally ill persons; Patient readmission
摘要
目的:探索有條件釋放下出院的香港精神病患者的特徵和短期成效,以及在首次有條件釋放下出院後一年再次入院的危機因素。
參與者與方法:此項研究主要為病歷回顧。其中包括所有在2005年日月31 日之前首次有條件釋放下出院,以及正在新界東醫院聯網接受精神科服務的病人,並且提取他們有條件釋放下出院後第一年的社會人口學數據、臨床狀況以及成效的有關資料。研究以單變數和邏輯數據分析將沒有及再度入院病人作比較以確定再重覆入院危機因素。
結果:共140位有條件釋放下出院的病人參與,當中主要診斷為恩覺失調、不服從治療和因精神問題導致的暴力行為。在出院後首年, 10%患者再有暴力行為,約5%有犯罪活動、1%企圖自殺或自殘。四分之一的患者須再度入院,相關因素包括以往入院紀錄、在有條件釋放下出院時較年輕、持續濫用藥物,和由自福利機構撫養。
結論:大部分患者在有條件釋放下出院後首年沒有暴力行為。研究結果顯示一些可介入的再度入院危機因素,例如持續濫用藥物。顯示改善社區出院後照顧服務是有可行的方法。研究結果提供有用資料,有助臨床實習、提供服務和作進一步研究。
關鍵詞:預測、精神病患者、病人再度入院
Introduction
1 The management of this group of patients is difficult. While they may become stable in hospital with the use of medication, they may discontinue these and quickly decompensate after discharge. Despite the wide variability in implementation and practice,2-5 all services aim to enhance community psychiatric care in patients who have poor insight and high-risk behaviour. The term Compulsory Community Treatment (CCT) was coined to refer to policies covering a wide range of interventions including community treatment orders, involuntary outpatient commitment, extended leave, conditional discharge (CD), conditional release, and supervised discharge.6 Use of CCT has, in fact, been expanding in western countries despite controversy over the legal, social, and ethical issues involved.7,8
Most studies have found that patients under CCT are male and those aged under 65 years.2,9-11 They are commonly single,12 and more likely to be living away from their families or to have changed their addresses shortly before being committed.2 They are generally of low educational level, unemployed, and relying on social security.13-15 Although schizophrenia is the most common diagnosis among patients under CCT, this group of patients also exhibit high diagnostic complexity.10-12
In Hong Kong, CD was first formalised and implemented in 1988. It can be applied to certified patients hospitalised in mental hospital who are stable enough to be discharged but are liable to have further risky behaviour upon relapse and prone to not comply with treatment. As with other forms of CCT, the legislation requires the patients to comply with certain conditions such as an obligation to be followed up in specified psychiatric clinics, take recommended medications, and allow access or monitoring by social workers and community psychiatric nurses.16 The conditions are clearly written and are fully understood by the patient. When the patient does not comply with these conditions, the responsible psychiatrist has the right to recall the patient to hospital for further management. The main differences between CD and other forms of CCT are that the latter, like involuntary outpatient commitment in the United States, require a court hearing to endorse the application and can also be applied to outpatients. Other forms of CCT not only attempt to prevent relapse and the risks associated with relapse, but also provide the option of a less restrictive place of treatment.
Our study aimed to evaluate the characteristics of CD patients in Hong Kong, explore their short-term outcomes and identify potentially modifiable outcome predictors. It was hoped that the results could provide meaningful preliminary data about the kind of patients the CD system was serving, their outcomes and the risk factors associated with re-hospitalisation.
Methods
Study Design and Subjects
This was a retrospective review of case notes. The target population included all adult CD patients under the care of the New Territories East (NTE) Cluster psychiatric service. Those patients with serious mental illnesses, who had high readmission rates and frequently defaulted follow-up, required priority follow-up (PFU). The PFU system is a system whereby mental patients with a history of criminal violence or a disposition to violence are identified and managed. Patients are categorised into 3 groups under this system. ‘Non-PFU’ means that there is no history of criminal violence or assessed disposition to violence; the ‘PFU target’ means that there is a history of criminal violence or assessed disposition to violence, whereas ‘PFU subtarget’ means that this patient is among the most dangerous of the patients with a history of criminal violence or assessed disposition to violence and requires ‘special assessment’ and extra care. All CD patients are assessed and monitored by the community psychiatric team (CPT). The CPT central registry that is kept for case notes tracing assisted the selection of subjects for this study.
The usual study period adopted by other studies into CCT ranged from 6 months to 1 year,15,17 so for the sake of comparison, we adopted the first year after the date the CD came into effect as the study period. The Hospital Authority (HA) is the only government-funded and statutory body providing public hospital services in Hong Kong. The NTE Cluster is one of the 7 geographically defined hospital management units under the HA. It covers a region with a total population of more than 1.3 million, one-fifth of the population of Hong Kong.
Definition of Terms
In this study, the term “index admission” refers to the admission after which the patient was discharged conditionally for the first time. “Index date” is the date of discharge from the index admission, the day when the CD came into effect. The period before the index admission is referred to as the “pre-CD period”; whereas the first year after the index date is the “post-CD period”. Admission due to relapse, non-compliance with conditions specified, and / or dangerous behaviour during the post-CD period is considered “readmission”. “Non-compliance” is defined as any recorded refusal to take medication or failure to take a depot injection within 2 weeks of the prescribed date unless an explanation was available.2 Any recorded refusal to attend the outpatient clinic, or failure to attend a scheduled appointment and not attending the subsequent or rearranged appointment without any evident explanation is also defined as “non-compliance”.
Data Collection
Data were collected from the case notes provided by 3 outpatient clinics in the NTE region. All data gathered were recorded in the notes by mental health professionals,
including psychiatrists, psychologists, psychiatric nurses, and social workers. Admission and discharge summaries of prior hospitalisation were used to supplement the clinical information recorded in the outpatient notes. The information was retrieved through the Clinical Management System and Psychiatric Clinical Information System, and a data form was designed for the purposes of this study.
Assessment
Baseline Measures (Pre-conditional Discharge Period)
Information included demographic characteristics, family history of mental and related illness, childhood history, medical history, history of violence and forensic record, attempted suicide or self-harm, substance misuse, psychiatric history, PFU status, details of index admission, and treatment history.
Outcome Measures (Post-conditional Discharge Period)
Information included readmission, history of interval violence, forensic contact, suicidal attempt or self-harm, substance misuse and compliance. Readmission to a psychiatric ward was chosen as the main outcome for analysis. Patients with readmissions in the post-CD period were classified as the ‘readmission group’ whereas those subjects who could be managed in outpatient settings without further readmission during the study period were categorised as the ‘no readmission group’. Hospitalisation due to reasons other than relapse, breaching conditions, and violence was excluded.
Statistical Analysis
The results were analysed using the Statistical Package for the Social Sciences version 14.0. The Chi-square test was used to compare categorical data between the 2 groups. Fisher’s exact tests were used when the expected cell count was less than 5. The independent t test was used to compare continuous variables. A multivariate analysis was used to investigate factors associated with readmission. A logistic regression was performed to estimate the odds ratio of factors associated with readmission in the post- CD period. A two-sided 5% level of significance was considered significant, 95% confidence intervals were provided when appropriate. The Joint Clinical Research Ethics Committee of the Chinese University of Hong Kong and NTE Cluster Hospitals approved the study. Data collection was executed in compliance with the Personal Data (Privacy) Ordinance. Measures taken included using number codes for subjects during data entry instead of their names and all data obtained were used in this study only.
Results
Characteristics of Conditional Discharge Patients
A total of 140 CD patients were being followed up in the NTE Cluster and had been first conditionally discharged before 31 August 2005. All were Chinese and aged between 18 to 65 years on the index date. Ninety six (68.6%) of them were male and 44 (31.4%) were female, giving a male to female ratio of 2.18:1. The mean age on the index date was 38.5 (SD, 9.4) years. Sixty five (46.4%) of them were single and 72 (51.4%) had studied at secondary level.
Comparison of Readmission Versus No Readmission Groups
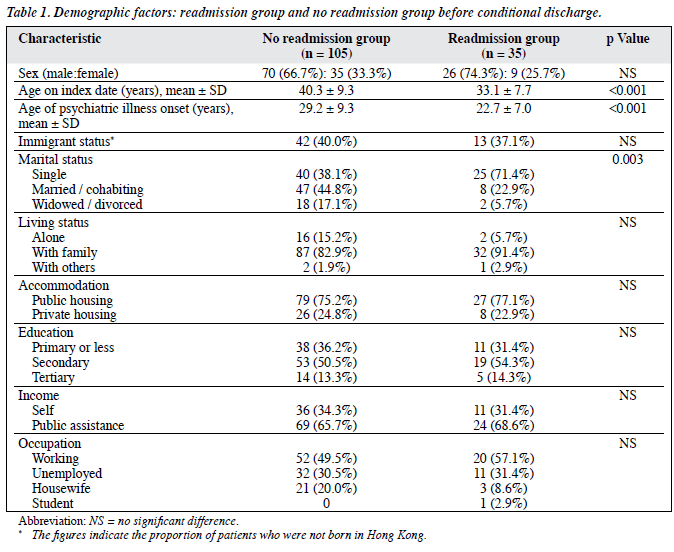
Thirty five (25%) subjects were readmitted during the study period. The readmission group was significantly younger on the index date (33.1 vs. 40.3 years, t = 3.79, p < 0.001) and more likely to be single (71.4% vs. 38.1%, χ2 = 11.89, p = 0.003). There was no statistically significant difference between the 2 groups in the other demographic factors (Table 1). More subjects were raised by the social welfare service in the readmission group (8.6% vs. 1.0%, Fisher’s exact test, p = 0.05) and more of those in the readmission group had a family history of suicide (17.1% vs. 2.9%, Fisher’s exact test, p = 0.01). Overall, 22% had a history of physical disease(s) but there was no significant difference between the groups in terms of medical history.
Most (80%) of the subjects had a history of violence prior to the index admission (Table 2). Thirty percent had a past forensic record, and 20% had a history of attempted suicide or self-harm (Chi-square, p = not significant). About 20% had a history of substance misuse before the index admission. No significant difference was found between the readmission group and the no readmission group in the types of substance misuse reported. Eighty five percent had a psychiatric diagnosis before the index admission and 23 (16.4%) subjects had documented co-morbidities. More than half (65.7%) had prior inpatient treatment before the index admission. The mean number of prior admissions was 2.3, with a range from 0 to 17. The average length of hospital stay was over 100 days. Nearly 90% of subjects with prior psychiatric treatment showed poor compliance. There was a statistically significant difference between the readmission group and no readmission group in terms of co-morbidities, prior psychiatric admissions, and frequency of psychiatric admissions before the index admission (Table 2) but no significant differences for psychiatric history and treatment compliance.
Details of Index Admission
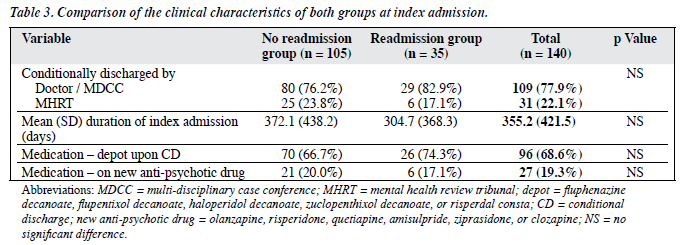
Table 3 gives a summary of the features of the index admission. Most (80.7%) subjects had a psychiatric diagnosis18 of schizophrenia while the others had a range of disorders (delusional disorder 7.9%; bipolar affective disorder, 5.0%; depression with psychosis, 2.1%; substance- related psychotic disorder, 4.3%). Secondary diagnoses were identified in 12.8% of subjects. Most (95%) patients were given a CD because of recent serious violence but in 7 (5%) subjects it was given for repeated serious suicidal attempts. The pattern of violence leading to the index admission involved, in over 70% of incidents, violence against people. In one-fourth of the incidents, patients carried weapon for threatening other people, attacking victims, or self-defence against a persecutory delusion. Two-thirds of the victims were patients’ parents, siblings, spouses, friends, acquaintances, or neighbours. Nine victims were documented as having serious injuries and 4 victims died as a result of the violence committed by the subjects. The other violent incidents involved property damage, starting fires, and creating a nuisance in public areas. Before the index admission, 35 (25%) patients had ‘priority follow-up target’ (PFU-T) status and 6 (4.3%) subjects had ‘priority follow- up subtarget’ (PFU-ST) status. After the index admission, 94 (67.1%) subjects were classified as PFU-T status and 32 (22.9%) subjects had PFU-ST status.
For treatment upon discharge, 68.6% of subjects were given depot, 3 of which were given a new generation depot, risperdal consta. Twenty percent of the patients were given new generation oral antipsychotic drugs. Six (22.9%) patients were given clozapine due to a refractory response to psychiatric treatment. Both groups had similar treatments upon discharge.
Outcomes
Readmission
Overall, 25% of the subjects were readmitted in the first year after the index admission. The main reason for readmission was a deterioration in the mental condition. The average length of hospitalisation was 114.3 (SD, 127.3) days (range, 12-609 days). Only 4 patients were readmitted more than 1 time in the study period. There were 20 recall admissions and 2 subjects were recalled to hospital because of non- compliance with psychiatric treatment without evidence of mental deterioration. Violence was documented in the records of 10% of the subjects post-CD. Four subjects displayed violence during verbal arguments and conflicts that were unrelated to psychiatric symptoms. The rest of the subjects displayed violence due to a deterioration in their mental condition and all of them were subsequently hospitalised. None of the violence resulted in serious injury to victims. The most common psychiatric symptoms related to violence were delusions of persecution and agitation. None reported commanding auditory hallucinations related to violence.
In the post-CD period, 4% had new forensic records. Most offences were related to the use of dangerous / illicit drugs. None required imprisonment or hospital orders in the study period. There was no difference between the readmission group and no readmission group in forensic records. Suicide attempts were documented in 2 (1.4%) cases. One had poor compliance with treatment and took an overdose of medication due to a relapse of mental illness. The other patient overdosed after a conflict with a spouse, but was not readmitted for this suicide attempt. Seventy percent of subjects misused various substances. All had prior histories of substance abuse and misused similar types of substances as those misused during the pre-CD period. Among them, 60% had a relapse of their mental illness and were readmitted.
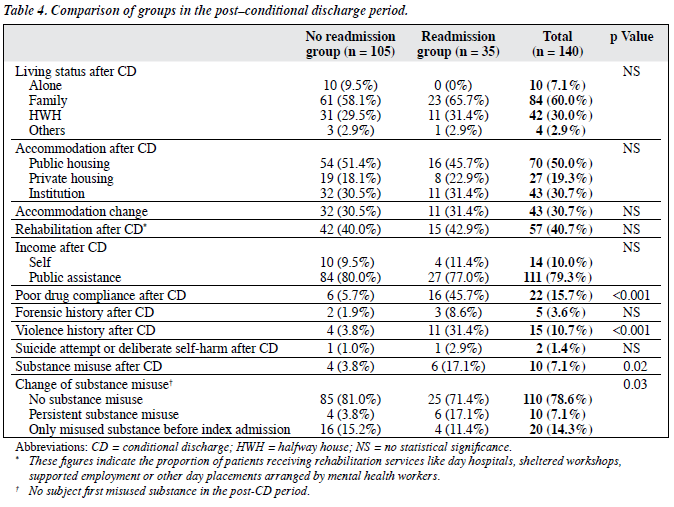
Over 80% of subjects had good treatment compliance levels. Nearly half of those subjects with poor compliance required readmission in the post-CD period. At the end of the study period, only 1 subject had his CD status revoked and none of the subjects had died (Table 4).
Factors Associated with the Risk of Readmission
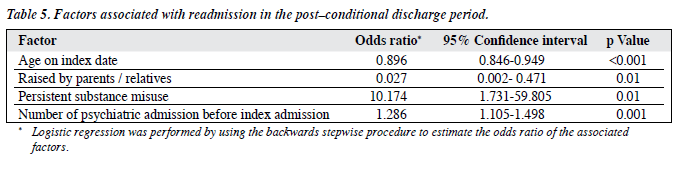
Multivariate analyses were used to identify those factors associated with a risk of readmission during the post-CD period (Table 5). Patients who had numerous psychiatric admissions before the index admission and persistently misused psychoactive substances after the index admission were found to be at risk of readmission. Patients who were older on the index date or who were raised in foster care were also found to have a higher risk for readmission during the post-CD period.
Discussion
This study identified the socio-demographic characteristics of CD patients in Hong Kong and found that, as in other studies, such patients are mostly male, single, and of young age.12,18,19 Most had a lower educational level and schizophrenia was the most common diagnosis. The subjects commonly had a history of psychiatric care and psychiatric inpatient treatment before the index admission and a history of violence and forensic records. All of these features were consistent with findings in previous studies.2-10
When compared with similar studies in Caucasian populations, the level of secondary diagnoses in our group was low. This could be explained by possible differences in documentation and diagnostic practice in Hong Kong.18
In future prospective studies, the prevalence of co-morbid diagnoses should be determined using structured diagnostic instruments. Overall, the short-term outcomes for patients on CD were satisfactory with low rates of recurrent violence and few attempted suicides. None committed serious violence within the study period. These outcomes may be associated with improvement in treatment compliance and the increased level of service and enhanced supervision provided to this group after being put on CD.11 On the other hand, it may simply be due to the coercive effect of the legislation.
Our results suggest that being of single status and having a younger age at the onset of psychiatric illness are factors associated with readmission. This finding is consistent with an earlier study that showed that poor outcomes in schizophrenia are associated with a younger age of onset.20 A younger age at the onset of psychiatric illness was also associated with increased violence. Patients with a family history of attempted suicide were found to have an increased risk of further attempts at suicide. Previous studies have shown that patients with a family history of suicide have reduced vulnerability / resiliency and poor problem- solving.21,22 As social stress is one of the precipitating factors for the relapse of psychotic disorders, this vulnerable group of patients might have a relatively higher risk of readmission because of further mental deterioration provoked by social stress. Mental co-morbidity, violence, and poor treatment compliance during the post-CD period were found to be significantly associated with risk of readmission.
An increased number of prior psychiatric admissions was predictive of future re-hospitalisation, a finding consistent with previous studies.5,11 This could be explained by the complex interaction between such factors as the severity of mental illness, treatment compliance, effectiveness of treatment, and community support. The risk of readmission increased if subjects continuously misused psychoactive substances, a finding consistent with an earlier study.14 Readmission of subjects who misused psychoactive substances could be directly or indirectly related to substance misuse. Psychoactive substance can both provoke violence23,24 and trigger psychotic symptoms.25
That age on index date emerged as one of the strongest risk factors for readmission was an interesting finding. It could suggest that the index admission indicated a ‘stage’ at which these patients decompensated to a considerable degree, leading to serious violence. If a CD is imposed at an early age it may imply a faster and more severe mental deterioration from the onset of mental illness. Patients brought up in residential placements had a higher risk of readmission. This finding might be explained by the underlying reasons for the social welfare placement as well as by the change in the social support systems for these patients. A study into the clinical characteristics of youths who lived away from families found that youths living away from their families were more seriously emotionally disturbed and more likely to receive treatment in residential care programmes.26 A history of physical abuse occurring before the age of 16 was found to have a significant relationship with violence,27 but because the number of subjects raised by welfare placement was small in the present study, this finding should be interpreted with caution. There were no significant differences in suicide attempts between the readmission group and no readmission group. The practice of placing patients on CD may account for this finding but this study could not ascertain whether or not CD can help to reduce suicidal behaviour.
As with any retrospective study, this study is limited by recording biases. Information needed by the study might not be documented in the case records and the quality of record keeping strongly determined the accuracy and completeness of data collection. The findings merely reflected the patterns of use of CD, largely within the catchment area, but may not represent the situation within the whole territory. Lastly, the study design was limited when determining the causal relationship of the association. Further prospective studies are required to assess in what way the variables might be related to the outcome measures.
This study provides preliminary local data on CD patients in Hong Kong. The identification of potentially modifiable risk factors for readmission such as persistent substance misuse suggests there are problems with the existing services for patients with co-morbid substance misuse. The recognition of risk factors predicting short-term readmission should facilitate effective clinical assessment and management. This study should be used as a base for future studies relating to CD and other community treatment orders.
Acknowledgement
The authors would like to thank Drs I Kam, S Fong, J So, and Professor Ungvari for their comments and advice on this report.
References
- Kastrup M. Who became revolving door patients? Findings from a nation-wide cohort of first time admitted psychiatric patients. Acta Psychiatr Scand 1987;76:80-8.
- Sensky T, Hughes T, Hirsch S. Compulsory psychiatric treatment in the community. I. A controlled study of compulsory community treatment with extended leave under the Mental Health Act: special characteristics of patients treated and impact of treatment. Br J Psychiatry 1991;158:792-9,804.
- Ajzenstadt M, Aviram U, Kalian M, Kanter A. Involuntary outpatient commitment in Israel: treatment or control? Int J Law Psychiatry 2001;24:637-57.
- O’Reilly RL, Keegan DL, Elias JW. A survey of the use of community treatment orders by psychiatrists in Saskatchewan. Can J Psychiatry 2000;45:79-81.
- Preston NJ, Kisely S, Xiao J. Assessing the outcome of compulsory psychiatric treatment in the community: epidemiological study in Western Australia. BMJ 2002;324:1244.
- Pinfold V, Bindman J. Is compulsory community treatment ever justified? Psychiatr Bull 2001;25:268-70.
- Allen M, Smith VF. Opening pandora’s box: the practical and legal dangers of involuntary outpatient commitment. Psychiatr Serv 2001;52:342-6.
- Holloway F, Szmukler G, Sullivan D. Involuntary outpatient treatment. Current Opinion in Psychiatry 2000;13:689-92.
- Swartz MS, Swanson JW, Wagner HB, Burns BJ, Hiday VA, Borum R. Can involuntary outpatient commitment reduce hospital recidivism? Findings from a randomized trial with severely mentally ill individuals. Am J Psychiatry 1999;156:1968-75.
- Xiao J, Preston NJ, Kisely S. What determines compulsory community treatment? A logistic regression analysis using linked mental health and offender databases. Aust N Z J Psychiatry 2004;38:613-8.
- 1 Kisely S, Smith M, Preston NJ, Xiao J. A comparison of health service use in two jurisdictions with and without compulsory community treatment. Psychol Med 2005;35:1357-67.
- O’Brien AM, Farrell SJ. Community treatment orders: profile of a Canadian experience. Can J Psychiatry 2005;50:27-30.
- Munetz MR, Grande T, Kleist J, Peterson GA. The effectiveness of outpatient civil commitment. Psychiatr Serv 1996;47:1251-3.
- Riordan S, Haque S, Humphreys M. Possible predictors of outcome for conditionally discharged patients — a preliminary study. Med Sci Law 2006;46:31-6.
- Vaughan K, McConaghy N, Wolf C, Myhr C, Black T. Community treatment orders: relationship to clinical care, medication compliance, behavioural disturbance and readmission. Aust N Z J Psychiatry 2000;34:801-8.
- Mental Health Ordinance, Chapter 136, Laws of Hong Kong. Hong Kong Government; 1997. Bilingual Laws Information System website: http://www.legislation.gov.hk/eng/home.htm. Accessed July 2006.
- Steadman HJ, Gounis K, Dennis D, Hopper K, Roche B, Swartz M, et al. Assessing the New York city involuntary outpatient commitment pilot program. Psychiatr Serv 2001;52:330-6.
- American Psychiatric Association. DSM-IV: Diagnostic and statistical manual of mental disorders, fourth edition. Washington DC: American Psychiatric Association; 1994.
- El YC, Durst R, Rabinowitz J, Kalian M, Teitelbaum A, Shlafman M. Implementation of order of compulsory ambulatory treatment in Jerusalem. Int J Law Psychiatry 1998;21:65-71.
- Lieberman JA, Sobel SN. Predictors of treatment response in course of schizophrenia. Current Opinion in Psychiatry 1993;6:63-9.
- Fergusson DM, Beautrais AL, Horwood LJ. Vulnerability and resiliency to suicidal behaviours in young people. Psychol Med 2003;33:61-73.
- Jeglic EL, Sharp IR, Chapman JE, Brown GK, Beck AT. History of family suicide behaviors and negative problem solving in multiple suicide attempters. Arch Suicide Res 2005;9:135-46.
- Swanson JW. Alcohol abuse, mental disorder, and violent behavior. An epidemiologic inquiry. Alcohol Health and Research World 1993;17:123-32.
- Walsh E, Buchanan A, Fahy H. Violence and schizophrenia: examining the evidence. Br J Psychiatry 2002:180:490-5.
- Dixon I, Haas G, Weiden PJ, Sweeney J, Frances AJ. Drug abuse in schizophrenic patients: clinical correlates and reasons for use. Am J Psychiatry 1991;148:224-30.
- Pottick KJ, Warner LA, Yoder KA. Youths living away from families in the US mental health system: opportunities for targeted intervention. J Behav Health Serv Res 2005;32:264-81.
- Swanson JW, Swartz MS, Essock SM, Osher FC, Wagner HR, Goodman LA, et al. The social-environmental context of violent behaviour in persons treated for severe mental illness. Am J Public Health 2002;92:1523-31.