Hong Kong J Psychiatry 2007;17:81-6
ORIGINAL ARTICLE
Dr Anna YK Wu, MBChB (CUHK), MRCPsych (UK), FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, Hong Kong, China.
Dr WF Chan, MBBS (HK), MRCPsych (UK), FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, Hong Kong, China.
Address for correspondence: Dr Anna YK Wu, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, Lok Man Road, Chai Wan, Hong Kong, China.
Tel: (852) 2595 6111; Fax: (852) 2595 9721; E-mail: wu_anna@hotmail.com
Submitted: 21 May 2007; Accepted: 4 July 2007
Abstract
Objectives: To identify the clinical characteristics and outcome of Hong Kong Chinese elderly persons who attempted suicide.
Participants and Methods: Thirty seven Chinese elders with suicidal ideas were evaluated over a 6-month follow-up period.
Results: There was a slight female predominance (1.2:1). Approximately 70% of patients had experienced stressful life events. Logistic regression showed that in these elders, medical burden was a significant predictor of suicidal attempts. Experiencing a stressful life event and severity of depression were significant determinants of the severity of suicidal ideation; 97% (n = 36) presented with depressive disorders. During the follow-up period, mortality was 5% (n = 2), the default rate was 8% (n = 3), and 3% (n = 1) attempted suicide. Suicidal ideation, severity of depression, and anxiety improved with treatment over 6 months.
Conclusions: The majority of elderly suicidal patients had depressive disorders. While the medical burden may be a modifiable risk factor, elderly with depression and stressful life events should be identified early for closer
Key words: Aged; Depression; Prognosis; Risk factor; Suicide, attempted
摘要
目的:識別企圖自殺的香港華裔老人的臨床特徵和治療結果。
參與者與方法:37位曾有自殺念頭的華裔老人接受為期6個月的隨訪追縱評估。
結果:37位老人中,女性稍多( 1.2: 1 )。七成病人經歷過沉重的生活事件。邏輯回歸分析顯示,在這群老人中,面對軀體病患的負擔是企圖自殺的一個重要預測因子。生活壓力事件和抑鬱的嚴重度明顯影響到老人產生自殺念頭的嚴重程度,而97%的老人(36名)有抑鬱障礙的情。在隨訪期,死亡率5% (2名),中斷治療比率8% ( 3名),企圖自殺率3% (1 名)。經過6個月的治療,自殺念頭的產生、抑鬱嚴重度、以及焦慮都有所減輕。
結論:大部分自殺的老年病人都有抑鬱障礙。接受治療的負擔可能是一個可變的危險因素,醫護人員反而要及早識別出有抑鬱又經歷過沉重生活事件的老人,予以更嚴密的監視。
關鍵詞:老人、抑鬱、預後、危險因素、企圖自殺
In 1998, suicide represented 1.8% of the global burden of disease. It is expected to increase to 2.4% by the year 2020. Suicide is among the 10 leading causes of death in all ages in most countries. Hong Kong’s suicide rate ranks in the middle of the global scale, and is comparable to that of Singapore among Asian countries.1 There is a clear tendency for suicide rates to increase with age, being about 2 to 3 times more frequent in the elderly than in younger persons.2 Hong Kong has among the highest old-age suicide rates in the world, being about 4 to 5 times the average.
Suicide in the elderly is of considerable medical and social significance, has a great social impact, and leads to intense stress among families. It remains a social taboo in the Chinese population. Due to long life expectancy, the proportion of elderly is increasing. In 2003, 11.7% of Hong Kong population was older than 60 years. The figure is expected to rise to about 27% in the year 2033 (http://www. info.gov.hk/censtatd). Thus the imminent expected growth in elderly suicides warrants appropriate interventions.
Suicidal behaviour includes suicidal ideation, suicidal attempts, and completed suicides. Suicide refers to any death that is a direct or indirect result of a positive or negative act accomplished by the victim himself / herself, which he / she knows or believes will produce such a result. Suicidal ideation refers to cognition that varies from fleeting thoughts that life is not worth-living, through very concrete, well-thought-out plans for killing oneself, to an intense delusional preoccupation with self-destruction.3 Although elderly suicidal risk factors have been extensively studied in previous studies, the focus is mainly on completed suicides. Longitudinal studies of elderly suicidal ideation and attempts are limited.4
There have been extensive studies about the risk factors or correlates of elderly suicide.5-10 Findings from these studies have yielded vast differences. Old-old groups have a higher rate of suicidal ideation11 and completed suicide.5,12 Female gender is associated with suicidal ideation11,13 and suicidal attempts,14 while males have the highest risk for completed suicide.5,15 Regarding marital status, results are inconclusive, though widowers have highest risk of having suicidal ideation.6 Poor social support,7 institutionalisation, and social isolation are associated with increased suicidal ideation,13 suicidal attempts, and completed suicides.8,16 Stressful life events like bereavement, family discord, physical illness, and other losses are risk factors of suicidal ideation.8,9 Medical burden is strongly associated with suicidal ideation and completed suicide,6,15,17 as is low level of functioning.17 Depressive disorders have been found in the majority of suicidal patients and suicide victims undergoing psychological autopsy.12,18
Local suicidal studies showed that single men had the highest rate of completed suicide. Economically inactive persons had a 6 times higher suicidal risk than those who were active.19 In that study, about half of the patients attempting suicide suffered from a mood disorder, the rate of repeated suicidal attempts was 3.6% and the rate of completed suicide was 5.5%. The female-to-male ratio was 1.6:1, most were married.20 In a recent psychological autopsy study, 86% of suicidal subjects suffered from psychiatric problems. Depressive disorders and a history of suicidal attempt are risk factors of late-life suicide in Hong Kong.21 Depressive symptomatology may be present but may not be sufficient to give rise to suicidal behaviour. The roles of different socio-demographic and psychological variables remain inconclusive.
The present study aimed to identify clinical factors contributing to suicidal behaviour and to examine outcomes, after an Elderly Suicide Prevention Programme (ESPP) had been implemented. It aimed to provide further information to facilitate more effective prevention and management of suicidal behaviour in the elderly.
Methods
Patients
From October 2002, the Hospital Authority of Hong Kong implemented an ESPP. Pamela Youde Nethersole Eastern Hospital (PYNEH), a regional acute general hospital, was 1 of the 5 centres for the programme. Elderly people with suicidal risks were referred to the ESPP from different sources including within PYNEH, general outpatient clinics, general practitioners, and non-governmental organisations, etc. Subjects for this study were recruited from the ESPP of the PYNEH from September 2003 to March 2004; interviews with the patients were conducted within 1 to 3 days of initial contact. Socio-demographic and clinical variables were documented. Information was obtained from interviews, and supplemented by informants and medical records. Those who had attempted suicide (suicidal attempters, SA) and those with suicidal ideation only (suicidal ideators, SI) were compared. Patients were observed in a naturalistic manner and reassessed 6 months later, though they continued to be followed up at the psychiatric clinic of PYNEH throughout that period. Pharmacological and psychological treatments were offered as appropriate, as well as domiciliary visits and telephone contacts made by psychogeriatric outreach team. Patients who lived outside the catchment area of PYNEH were excluded.
Those recruited had to give informed consent, and the aims of the study and procedures were explained to the patients and their relatives. The Ethics Committee of PYNEH endorsed the entire study.
Assessment
Demographic data were collected. Life events were codified according to the Social Readjustment Rating Scale.22 Nine events were selected from the Scale and one additional event termed ‘relationship problem with children’. Presence and absence of individual stressful events was documented. Nine major systematic disease categories (cardiac, vascular, endocrine, respiratory, gastric, hepatobiliary, renal, musculoskeletal, and neurological) and sensory impairment were documented. In addition, the Cumulative Illness Rating Scale23 (CIRS) was used as a measure of the overall physical illness burden. The psychiatric subscore was omitted. Scoring was by consensus at meetings with a consultant geriatric psychiatrist. Autonomy in activities of daily living was assessed by Activities of Daily Living24 and Instrumental Activities of Daily Living tools.25
Suicidal attempts involved behaviour that could vary from suicidal gestures and manipulative attempts to serious but unsuccessful attempts to kill oneself. Any suicidal attempts made prior to recruitment were documented. The Chinese version of the Geriatric Depression Scale26 (GDS) was administered upon recruitment. The Chinese version of the Hamilton Depression Rating Scale was used to measure the severity of depressive symptoms (HAMD score).27 The Hamilton Anxiety Rating Scale for Anxiety (HAMA) was used to measure the severity of anxiety.28 Severity of suicidal ideation was measured by the Chinese version of the Beck Scale for Suicidal Ideation (BSS).29 Cognitive function was assessed with the Mini-Mental State Examination (MMSE).30 Psychiatric diagnosis was made according to the 10th edition of the International Classification of Diseases.31 Suicidal behaviour (attempted or completed suicide), its method, mortality, resulting psychiatric admission, and instances of defaulted follow-up were also documented.
Statistical Analysis
The clinical characteristics of the subjects were reported. Mean and standard deviation were calculated for continuous variables. Frequency tables were used to describe categorical variables. Pearson correlations were used to examine correlations between GDS and HAMD, HAMD and HAMA, BSS and GDS, BSS and HAMA. Since suicidal ideation is a significant symptom of depressive disorder, correlation between depression and suicidal ideation was calculated by using the Pearson correlation between BSS and HAMDns (HAMD score minus suicidal subscore). Groups of SI and SA were compared for socio-demographic and clinical factors by the t and Chi-square tests. Linear regression analyses were performed on socio-demographic and clinical factors in order to identify the actual contribution of each factor to suicidal ideation. Logistic regression analyses were also performed on socio-demographic and clinical factors, with a view to identifying significant predictors of suicidal attempts. As for outcome at 6-month follow-up, paired sample t tests were used to test the changes of BSS, HAMA, HAMDns. Mortality and defaulted cases were represented as percentages. Defaulted and dead patients were analysed by comparison to active cases. Confidence intervals (95%) were used in all statistical analyses. All analyses were performed using the Statistical Package for Social Sciences, Windows version 11.5 (SPSS Inc., Chicago [IL], US).
Results
Socio-demographic Profiles of Subjects
There were a total of 37 consecutive patients recruited from September 2003 to March 2004, amounting to a 100% response rate from ESPP recruits. Of these cases, 7 had made suicidal attempts with suicidal ideation (SA); 30 had suicidal ideation without an attempt (SI). Demographic and clinical characteristics of the cases are summarised in Table 1. A minority of patients were still working (n = 2, 5%). Five (14%) lived in an old-aged home and 1 (3%) lived alone at home. Eleven (30%) reported no stressful life events. The most frequently reported stressful life events were personal physical illness (n = 11, 30%), death of a spouse (n = 3, 8%), and change in sleep habits (n = 3, 8%) [Table 2]. The MMSE was 20.9 (SD, 6.9) when entering into the study. The distribution was skewed, with 63% of the cases having an MMSE more than 20 and 30% (n = 11) were diagnosed with dementia.
Thirty six (97%) were diagnosed with depressive disorders, most commonly major depression (n = 23, 62%). Eight (22%) had dementia with depressive symptoms. Three (8%) had dementia with mixed symptoms; 2 (5%) had dysthymia. Only 1 (3%) did not have a depressive disorder. He had organic psychosis, precipitated by steroid administration for physical illness during inpatient medical care.
Association between Depression and Anxiety
The mean HAMD score was 20.5 (SD, 6.9). Mean HAMDns was 18.0 (SD, 6.5). For anxiety symptoms, the mean HAMA score was 17.3 (SD, 7.3). Severity of suicidal ideation measured by the BSS was 15.8 (SD, 5.1). The GDS was significantly correlated with HAMD (Pearson correlation, r = 0.50, p = 0.003). Both HAMA and HAMD were found to be statistically significantly correlated (Pearson correlation = 0.66, p < 0.001). The BSS was not correlated with the GDS (Pearson correlation = 0.30, p = 0.08), but was significantly correlated with HAMDns (Pearson correlation = 0.36, p = 0.03). The BSS and HAMA displayed a statistically significant association (Pearson correlation = 0.34, p = 0.04).
Factors Associated with Suicidal Ideas and Attempts
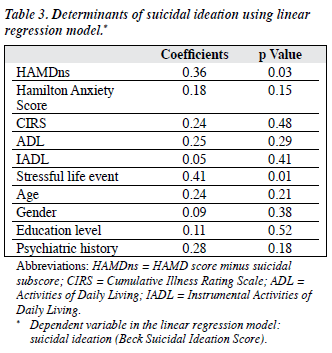
Associated factors for suicidal ideation were stressful life events (p = 0.01) and severity of depression (HAMDns) [p = 0.03] from linear regression analyses, which were all significant on deviance analysis (Table 3). Predictors of suicidal tendency (at the beginning state of the study period) were measured by logistic regression analysis of the cases (SA and SI groups together). Medical burden (CIRS score) was found to be a significant determinant of suicidal ideation (p = 0.01). Other factors were not significant on analysis.
Clinical Outcome at Six Months
After 6 months, 32 (86%) were still being regularly followed up at the psychiatric unit of PYNEH. Three (8%) patients had defaulted, 2 (5%) had died of physical problems during the study period. All active cases (n = 32) continued antidepressant medication. All the 3 defaulting patients refused psychiatric service — one opted for psychotherapy, and 2 expressed being depressed and suicidal, yet were ‘rational’ and displayed ‘normal process of ageing’. They also expressed concern at being discriminated by others receiving psychiatric services. All 3 were contacted by the psychogeriatric outreach team by telephone after 6 months and noted to be alive; evidently none had attempted suicide during the study period. One (3%) from SI group attempted suicide during the follow-up period, taking an overdose of a hypnotic. Five (14%) were hospitalised for in-patient psychiatric care in PYNEH during the follow-up period.
The mean HAMDns was 3.7 (SD, 3.8) after 6 months. The severity of depressive symptoms had significantly decreased after 6 months (paired t test, t = 12.4, p < 0.001). The mean HAMA was 5.0 (SD, 4.1) and was significantly reduced (paired t test, t = 9.6, p < 0.001). The mean BSS score was 1.09 (SD, 2.66), it was also significantly reduced at follow-up (t = 13.9, p < 0.001). The BSS score still correlated significantly with HAMDns (Pearson correlation = 0.62) and HAMA (Pearson correlation = 0.81) after 6 months (both p < 0.001).
Discussion
Suicidal behaviour is a continuum, the ‘suicidal process’ is used to describe the intra-individual process in reaction to the environment. It starts with feelings of despair, then fleeting suicidal thoughts, evolving with concrete plans, suicidal attempts, and eventually may result in completed suicide (involving increased levels of intent and lethality).32 In this study, the mean age of the subjects fell marginally in the younger-old group, which was comparable to findings of a recent local elderly suicidal ideation study.33 The slight female predominance was not marked, when compared with previous study findings,13 and lower than 1.6:1, the ratio noted in a previous local elderly suicidal attempt study.20 Our findings showed that 57% of suicidal elderly patients were married, which was contrary to western studies where widowhood9,34 and not being married were correlated with suicidal ideation. Local studies showed single males having highest rate of suicide19 but more elderly suicidal attempters were married.21
The majority of subjects lived with their family or others (e.g. domestic helpers), which was vastly different from previous studies7,13 that incriminated social isolation and institutionalisation in suicidal ideation. However, the living arrangements for Hong Kong elderly differ from those in western societies. Merely using living arrangement may not be adequate to examine relationships between suicidal ideation and social isolation. Life events are well- known precipitants for major psychiatric illnesses. Our study concurred with the results from previous studies8,9 that personal physical illness and bereavement were important stressful life events associated with suicidal ideation in the elderly. Change in sleep habits was the third most common life event. Sleep problems are very common in the elderly and may be due to physiological changes with ageing. A local study showed 75% of elderly had sleep disturbance; 42% of whom reported persistent sleep disturbance.35 Several studies have found that sleep disturbance (that can be bi-directional) predicts depression in elderly adults. Association of sleep disturbance and depression needs to be further explored. Many patients report sleep disturbances of various durations before presentation of depressive symptoms. Despite the controversy about sleep disturbance as a cause or effect of elderly depression, it was nevertheless a marker of one of the stressful events in this study.
We found 97% of patients had depressive disorders, which agreed with findings from completed suicide studies,3,17 and similar to findings from a local study,21 where 87% of suicidal victims had a psychiatric diagnosis (mainly depressive disorders). It can be postulated that depression plays a major part in both suicidal ideation and completed suicide in the elderly. Severity of suicidal ideation correlated positively significantly with modified severity of depression, which also agreed with previous studies.13,18 Major depression occurs in 1 to 3% of the general elderly population with an additional 8 to 16% having clinically significant depressive symptoms. However, fewer than 20% of these are detected or treated.36 Bereavement, sleep disturbance, disability, prior depression, and female gender were found to be significant risk factors for elderly depression. Elderly depression is frequently undiagnosed due to atypical presentations, where vegetative symptoms are more common. Co-morbid medical illnesses also hinder a precise diagnosis. Elderly depression is frequently undertreated, as grief, concurrent medications, altered physiology, co-morbid medical conditions, etc. all complicate management. Depressive disorders also hinder the treatment of medical illnesses and increase the burden of illness and costs. As depressive disorders afflict the majority (of elderly patients with suicidal ideation), elderly depressed patients should be targeted for intervention.
For anxiety symptoms, the mean HAMA score was clinically significant. In the elderly, depression is commonly present with concurrent symptoms of anxiety or co-morbid anxiety disorders. Such co-morbidity is associated with a severe depressive illness and greater suicidality.37 It also explains the positive correlation between suicidal ideation and severity of anxiety. It causes great distress, poor social function, and a high level of somatic symptoms. A similar study38 found a relatively high rate of current and lifetime anxiety disorders in elderly depressed patients. It is debatable as to whether anxiety symptoms are part of the depressive disorder or a separate co-morbidity. A recent study suggested that a dimensional classification is more appropriate than a categorical classification of depression and generalised anxiety.39
Vast number of studies identified different socio- demographic and clinical factors contributing to suicidal behaviour. Linear regression studies we undertook show that only a stressful life event and severity of depression were significant in our elderly patients with suicidal ideation. This finding agreed with previous studies.13,18 From the logistic regression study, medical burden was the only clinical determinant of suicidal tendency in elderly patients. We postulate that medical burden works through depression, as almost all patients had depressive disorders.
The HAMDns and HAMA decreased at the 6-month follow-up. Thereafter, the persistent correlation of BSS with HAMDns and HAMA indicated that improvement of depressive and anxiety symptoms resulted in (a) decreased severity of suicidal ideation, and in all suicidal ideation, (b) decreased severity of depression and (c) decreased post– follow-up period of anxiety. A low default and reattempt rate, and absence of suicidal mortality suggest that the current service is promising. Use of telecommunications was confirmed in earlier studies,40 as a means of alleviating subjective feelings of social isolation and improving access to help for elderly suicidal patients. In addition, community nurses in psychiatry have long adopted the use of domiciliary visits in psychiatry.
There are a few methodological limitations that should be addressed. At the outset, the sample size was small. This may result in type-1 and type-2 statistical errors. Based on a recent local study, the prevalence of suicidal ideation in the elderly was 6%,4 for which reason a far greater number of suicidal elderly were expected. This low prevalence could be explained by the study being performed in a tertiary centre. The problem studied only represented the tip of an iceberg. Moreover, the study period only lasted for 6 months so that longitudinal courses of suicidal ideation may not have been fully examined. This study could be viewed as a preliminary outcome examination, requiring longitudinal studies of longer duration in the future. Elderly patients may present with silent, subtle behaviours with unconscious intent to die. The number of elderly at suicidal risks may be underestimated. As suicide is still a taboo in Chinese societies, patients with such ideation may remain undisclosed and psychiatric services not used. The study could have been improved with more resources and if it was multi-centred and community-based. Controls could be recruited from several groups (elderly community centres or from general household surveys). Lastly, further studies with longer follow-up periods should be performed.
It is clear that detection of depression in the elderly is a prime target for the ESPP. Social services, which provide assistance to improve coping, are also important in decreasing the impact of stressful life events on the elderly. Since medical burden is an important clinical determinant for suicidal attempts in elderly patients, healthcare workers of different specialties should be educated in the proper detection of elderly depression. Current services providing collaborative care to elderly suicidal patients should be continued. General education of the public also helps to improve acceptance of psychiatric services for the treatment of depression, and to correct the misconception that depression and suicidality are a normal part of ageing.
References
- Figures and facts about suicide. WHO/MNH/MBD/99.1. Geneva: World Health Organization; 1999.
- Diekstra RF, Gulbinat W. The epidemiology of suicidal behaviour: a review of three continents. World Health Stat Q 1993;46:52-68.
- Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry 2002;1:181-5.
- Chiu HF, Chan S, Lam LC. Suicide in the elderly. Curr Opin Psychiatry 2001;14:395-9.
- Harwood DM, Hawton K, Hope T, Jacoby R. Suicide in older people: mode of death, demographic factors, and medical contact before death. Int J Geriatr Psychiatry 2000;15:736-43.
- Szanto K, Gildengers A, Mulsant BH, Brown G, Alexopoulos GS, Reynolds CF 3rd. Identification of suicidal ideation and prevention of suicidal behaviour in the elderly. Drugs Aging 2002;19:11-24.
- Alexopoulos GS, Bruce ML, Hull J, Sirey JA, Kakuma T. Clinical determinants of suicidal ideation and behavior in geriatric depression. Arch Gen Psychiatry 1999;56:1048-53.
- Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav 2002;32:1-9.
- Szanto K, Prigerson H, Houck P, Ehrenpreis L, Reynolds CF 3rd. Suicidal ideation in elderly bereaved: the role of complicated grief. Suicide Life Threat Behav 1997;27:194-207.
- Barraclough BM. Suicide in the elderly: recent developments in psychogeriatrics. Br J Psychiatry 1971;(Suppl 6):S87-97.
- 1 Skoog I, Aevarsson O, Beskow J, Larsson L, Palsson S, Waern M, et al. Suicidal feelings in a population sample of nondemented 85-year-olds. Am J Psychiatry 1996;153:1015-20.
- Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry 1996;153:1001-8.
- Scocco P, Meneghel G, Caon F, Dello Buono M, De Leo D. Death ideation and its correlates: surveys of an over-65-year-old population. J Nerv Ment Dis 2001;189:210-8.
- Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Joyce PR, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med 1999;29:9-17.
- Waern M, Rubernwitz E, Runeson B, Skoog I, Wilhelmson K, Allebeck P. Burden of illness and suicide in elderly people: case-control study. BMJ 2002;324:1355.
- Merrill J, Owens J. Age and attempted suicide. Acta Psychiatr Scand 1990;82:385-8.
- Conwell Y, Lyness JM, Duberstein P, Cox C, Seidlitz L, DiGiorgio A, et al. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc 2000;48:23-9.
- Shah A, Hoxey K, Mayadunne V. Suicidal ideation in acutely medically ill elderly inpatients: prevalence, correlates and longitudinal stability. Int J Geriatr Psychiatry 2000;15:162-9.
- Yip PS, Chi I, Yu KK. An epidemiological profile of elderly suicides in Hong Kong. Int J Geriatr Psychiatry 1998;13:631-7.
- Chiu HF, Lam LC, Pang AH, Leung CM, Wong CK. Attempted suicide by Chinese elderly in Hong Kong. Gen Hosp Psychiatry 1996;18:444- 7.
- Chiu HF, Yip PS, Chi I, Chan S, Tsoh J, Kwan CW, et al. Elderly suicide in Hong Kong — a case-controlled psychological autopsy study. Acta Psychiatr Scand 2004;109:299-305.
- Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res 1967;11:213-8.
- Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc 1968;16:622-6.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965;14:61-5.
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179- 86.
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. In: Brink T, editor. Clinical gerontology: a guide to assessment and intervention. New York: The Haworth Press; 1986:165-73.
- Zheng YP, Zhao JP, Phillips M, Liu JB, Cai MF, Sun SQ, et al. Validity and reliability of the Chinese Hamilton Depression Rating Scale. Br J Psychiatry 1988;152:660-4.
- Hamilton M. The assessment of anxiety scales by rating. Br J Med Psychol 1959;32:50-5.
- Zhang J, Norvilitis JM. Measuring Chinese psychological well-being with Western developed instruments. J Pers Assess 2002;79:492- 511.
- Chiu HF, Lam LC, Chi I, Leung T, Li SW, Law WT, et al. Prevalence of dementia in Chinese elderly in Hong Kong. Neurology 1998;50:1002- 9.
- The ICD-10 Classification of Mental and Behavioural Disorders. Geneva: World Health Organization; 1992.
- Van Heeringen K, Hawton K, Williams JM. Pathways to suicide: an integrative approach. In: Hawton K, Van Heeringen C, editors. International handbook of suicide and attempted suicide. Chichester: John Wiley & Sons Ltd; 2000:224-34.
- Yip PS, Chi I, Chiu H, Chi Wai K, Conwell Y, Caine E. A prevalence study of suicide ideation among older adults in Hong Kong SAR. Int J Geriatr Psychiatry 2003;18:1056-62.
- Luoma JB, Pearson JL. Suicide and marital status in the United States, 1991-1996: is widowhood a risk factor? Am J Public Health 2002;92:1518-22.
- Chiu HF, Leung T, Lam LC, Wing YK, Chung DW, Li SW, et al. Sleep problems in Chinese elderly in Hong Kong. Sleep 1999;22:717-26.
- Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry 2003;160:1147-56.
- Lenze EJ. Comorbidity of depression and anxiety in the elderly. Curr Psychiatry Rep 2003;5:62-7.
- Lenze EJ, Mulsant BH, Shear MK, Schulberg HC, Dew MA, Begley AE, et al. Comorbid anxiety disorders in depressed elderly patient. Am J Psychiatry 2000;157:722-8.
- Schoevers RA, Beekman AT, Deeg DJ, Jonker C, van Tilburg W. Comorbidity and risk-patterns of depression, generalised anxiety disorder and mixed anxiety-depression in later life: results from the AMSTEL study. Int J Geriatr Psychiatry 2003;18:994-1001.
- De Leo D, Dello Buono M, Dwyer J. Suicide among the elderly: the long-term impact of a telephone support and assessment intervention in northern Italy. Br J Psychiatry 2002;181:226-9.