Hong Kong J Psychiatry 2009;19:107-11
ORIGINAL ARTICLE
香港思覺失調年青患者的自我認知體重及自我體型滿意度的準確性
黃美彰、左思賦、呂世裕
Dr Mimi MC Wong, MBBS (HK), MRCPsych, Castle Peak Hospital, 15 Tsing Chung Koon Road, Tuen Mun, Hong Kong.
Dr Steve Tso, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Castle Peak Hospital, 15 Tsing Chung Koon Road, Tuen Mun, Hong Kong.
Dr Simon SY Lui, MBBS (HK), MRCPsych, FHKCPsych, FHKAM (Psychiatry), Castle Peak Hospital, 15 Tsing Chung Koon Road, Tuen Mun, Hong Kong.
Address for correspondence: Dr Mimi MC Wong, Castle Peak Hospital, 15 Tsing Chung Koon Road, Tuen Mun, Hong Kong.
Tel: (852) 2456 7111;
E-mail: wmc009@ha.org.hk
Submitted: 22 December 2008; Accepted: 19 February 2009
Abstract
Objectives: Satisfaction with body weight is more closely related to one’s perception rather than one’s actual body weight. It is important to understand the body weight perceptions of individuals with psychotic disorders to enhance appropriate weight management.
Participants and Methods: Information regarding body mass index, attitude towards body weight and figure rating was gathered from 87 young adults with psychotic disorders and 102 age- and education- matched controls.
Results: Patients were significantly heavier than controls and were aware of their overweight status. Members of both groups wished to lose weight even when their body weight was within the normal range. The wish to do something about their weight status correlated highly with their perception of their weight status (rs = 0.96-1.00, p < 0.01) rather than their actual weight status (rs = 0.62-0.68, p < 0.01).
Conclusions: Young adults with psychotic disorders are concerned about their weight. As the wish to do something about weight is more closely correlated to how their weight is perceived, it is important to assess the individual’s perception of their body weight status. Health care professionals should be aware of this in order to assist body weight management.
Key words: Antipsychotic agents; Body image; Body mass index; Obesity; Psychotic disorders
摘要
目的:是否滿意自己體重與實際體重並不相符,反而與自我認知體重更有關係。所以要有適當的體重控制行為,先要了解思覺失調患者的自我認知體重。
參與者與方法:87位思覺失調的年青患者,及102位年齡及教育背景相符的對照組參與本研究。找出參與者的體重指數,及他們對自我體重及自我體型的態度。
結果:思覺失調患者的體重比對照組明顯較重,他們也知悉自己的超重情況。縱然體重屬正常,兩組的參與者都希望減肥。他們改變自己體重的願望與自我認知體重明顯相關(rs = 0.96- 1.00,p < 0.01),而並非與他們的實際體重相關(rs = 0.62-0.68,p < 0.01)。
結論:思覺失調的年青患者很重視自己的體重。由於他們改變自己體重的願望與自我認知體重明顯相關,有需要評估個人的自我認知體重情況。醫護人員要先了解這一點,才能協助病者進行體重控制計劃。
關鍵詞:抗精神病藥物、自我形象、體重指數、肥胖、思覺失調
Introduction
Body image refers to a person’s perceptions, attitudes, and experiences about his / her body. Weight perception is an important part of this concept. Body weight perceptions are not in agreement with actual weight all the time. One study found that 12% of Taiwanese men and 57% of Taiwanese women overestimated their body shape.1 Weight control behaviours are motivated by perceived weight rather than actual body mass index (BMI).2 It has been shown that dissatisfaction with one’s body weight is an important predictor for engagement in various weight loss activities.1 This is also true for patients with schizophrenia.3 Whether accurate or not, people who perceive themselves as overweight wish to, or even try to, lose weight. A discrepancy between the actual and perceived body weight can lead to harmful unnecessary weight reduction if a person perceives that he is overweight but is actually not. On the other hand, if a person is not aware that he is overweight, he is unlikely to get involved in a weight reduction programme.
Attitudes towards body size and preferences for a particular level of fatness are mediated by local social and cultural factors.4 Under the influence of 21st century culture, where thinness equals beauty, negative views towards fatness have been magnified. Studies of body weight perceptions among adolescents in Hong Kong have found poor agreement between BMI and perceived weight in adolescents, particularly in females who frequently overestimated their weight.2 The weight perception in obese schizophrenic patients has been found to be fairly accurate in overseas studies3 but there is little local data concerning the weight perception of patients with psychotic disorders. A group of schizophrenic patients were found to be significantly more likely to underestimate their weight than normal controls (46% versus 18%).5 It would be interesting to compare the body weight perceptions of individuals with psychotic disorders with those of normal controls in Hong Kong.
This study aimed to examine (1) the body figure and weight satisfaction and the accuracy of body weight perception in cohorts with psychotic disorders and those without psychotic disorders in Hong Kong; and (2) the relationship between perceived and actual body weight and weight change behaviour.
Methods
Samples
The patient group was recruited at the Early Assessment Service for Young People with Psychosis (EASY) outpatient clinic of a psychiatric hospital serving a population of about one million in Hong Kong. Inclusion criteria were as follows: patients had a primary diagnosis falling into the schizophrenia spectrum disorder category as per the criteria of the International Classification of Disease – 10th Revision (ICD-10) classification of mental and behavioural disorders; were able to give informed consent; and had adequate command and understanding of Chinese. Patients who were intellectually subnormal or were diagnosed with eating disorders were excluded.
The controls were recruited from a local secondary school and were matched for age and educational level with the patient group. Inclusion criteria required that they were able to give informed consent and to communicate in written Chinese. Those who had histories of being diagnosed with schizophrenia spectrum disorders and eating disorders under the ICD-10, and those with a score higher than or equal to 2 on the Chinese version of the SCOFF questionnaire, which is a highly sensitive screening tool for eating disorders,6 were excluded.
The study was performed during 3 visits in 3 consecutive weeks to the clinic. Subjects who fulfilled the study selection criteria and were able to give consent were enrolled. Those who did not attend the clinic were interviewed when they came back for follow-up on another day. The diagnoses of the patient group were confirmed clinically by interviewing the patient and caregivers and reviewing the case notes. Patients’ body weights and heights were measured in the clinic. For the control group, teachers distributed the questionnaires to the students and measured the students’ body weights and heights at school.
Measurements
Demographic data collected included age, gender, educational level, occupation, and physical health status.
Objective Weight Status
Weight and height were assessed for all participants. The BMI was calculated using weight in kilograms divided by the square of the height in metres. It was classified according to the BMI classification for Asian populations proposed by the World Health Organization7 — BMI: lower than 18.5 kg/m2 as underweight, 18.5-22.9 kg/m2 as normal weight, and equal to or greater than 23 kg/m2 as overweight.8 For subjects younger than 18 years old, local growth charts with BMI and age were used to define underweight, normal weight, and overweight, because BMI changes with age.9 Those with a BMI below 10% of the age-adjusted BMI were defined as underweight, while those with a BMI above 90% were defined as overweight.10 Those between 10 and 90% were defined as having normal weight.
Subjective Weight Perception
A body image questionnaire comprising 2 parts — the Figure Rating Scale (FRS)11 and cognitive attitude towards body size1 — was used to assess body and weight satisfaction. In the FRS, there were 7 male / female contour drawings, in increasing body size from left to right. Participants were asked to choose the figure drawing that most accurately represented the size of their own bodies and the one that represented their ideal figure. Dissatisfaction with body figure could be calculated by the difference between the 2 ratings (current figure – ideal figure). For the cognitive attitude assessment, participants were asked whether they thought they were underweight, of normal weight, or overweight and whether they would like to gain weight, stay the same, or lose weight.
Discrepancy between Perceived and Actual Body Weight
The group chosen by the participants (underweight, normal weight, overweight) was compared to the group their BMI belonged to (underweight, normal weight, overweight).
Statistical Analysis
Data were analysed using the Statistical Package for the Social Sciences (SPSS) Windows version 16.0. Data were reported as mean and standard deviation. Spearman’s rank correlation coefficients were computed between actual body weight, perceived body weight and the wish to do something about their weight. Student’s t test was used to test the significance of the difference in age between groups. The significance of figure-rating differences was tested with the Mann-Whitney U test. Chi-square analyses were used to calculate the significance of differences between the genders and patient / control groups in the actual and perceived BMI groups. P values less than 0.05 were considered significant.
Ethics Approval
The New Territories West Cluster Clinical and Research Ethics Committee approved the research protocol.
Results
Demographic Characteristics
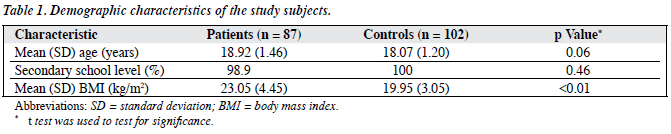
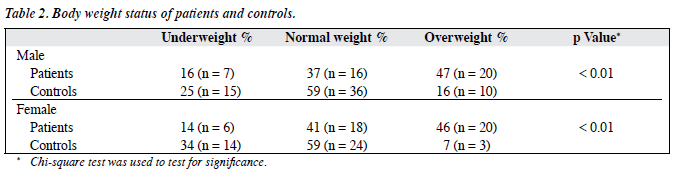
A total of 95 patients were interviewed and 87 who fulfilled the inclusion criteria were recruited into the study. Of 112 questionnaires received from the control group, 10 were excluded from the study due to incomplete data or inability to fulfil the inclusion criteria. There were no significant differences in the baseline characteristics of excluded and included individuals. In the patient group, the gender ratio was approximately 1:1 (male, 49.4% and female, 50.6%) but in the control group, 59.8% were male. The patient group had a significantly higher BMI than the control group (p < 0.01) [Table 1]. The actual BMI and perceived weights of patients and controls are shown in Table 2. Nearly half of the patient group was overweight, which was significantly more than the control group.
Perception of Body Weight
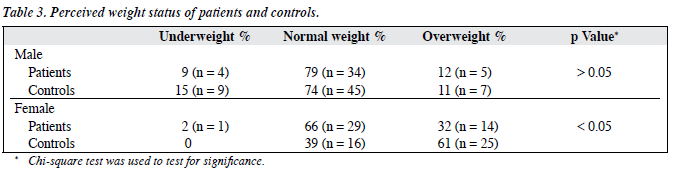
As with the control subjects, about 90% of male overweight patients and all of the female overweight patients accurately perceived their overweight status. Both groups overestimated their weight status, a trait more severe among females. About 32% of female patients perceived they were overweight compared to 12% of male patients (p < 0.05) [Table 3]. Among the controls, 61% of females perceived they were overweight compared to 11% of males (p < 0.01). Even though they were in the underweight group, 83% of the female controls and 64% of the female patients perceived themselves to be overweight or normal.
Correlation between Actual Weight Status, Perceived Weight Status, and the Wish to Do Something about Weight
The correlation between actual weight status and self-perceived weight status was rs = 0.67 and rs = 0.72 (p <0.01) in the control and the patient groups, respectively. The correlation between the wish to do something about their weight status and the perception of weight status was rs = 0.96 in the control group and rs = 1.00 in the patient group which was higher than the correlation between the wish to do something about their weight and the actual weight status (rs = 0.62 in the control group and rs = 0.68 in the patient group).
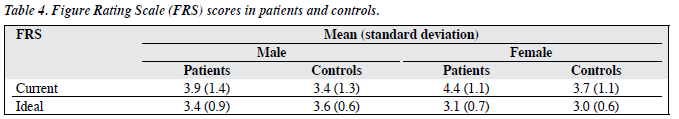
Male patients chose a heavier figure as their current figure than male controls (z score = –2.0, p < 0.05). This applied to female patients and controls as well (z score = –2.4, p < 0.05). The correlation between the current figure and ideal figure in the FRS was rs = 0.24 (p < 0.05).
The FRS score means and standard deviations are presented in Table 4. The mean body dissatisfaction score (current figure rating – ideal figure rating) was 0.6 ± 1.5 for male patients, -0.2 ± 1.1 for male controls, 1.3 ± 1.2 for female patients, and 0.7 ± 1.1 for female controls. The differences were statistically significant. Using a Chi-square analysis, a significant number of patients and controls who had normal body weights were found to be dissatisfied with their body size and wanting to be slimmer, with body dissatisfaction scores equal to or larger than 1 (p < 0.01). The problem was more severe in females, particularly the female controls. While most underweight females were satisfied with their body size, more of the underweight males wished to be heavier (71.4% of males versus 16.7% of females).
Discussion
In this study, young adults with psychotic disorders tended to overestimate their body weights. This was particularly true for females, although the severity of the problem was less than that in female controls. Most overweight patients are aware of their weight status and, like the controls, would overestimate their weight status even if underweight or of normal weight. Underweight male patients wanted to have a larger body size but female patients always wished to be slimmer, even those who were in the underweight group.
Westernisation and the influence of the media have caused people in this part of the world to constantly seek a slim body figure. Adolescents and young adults are particularly vulnerable due to their developing cognition and body images. Findings from this study concur with research done locally as well as internationally that body weight perceptions tend to be inaccurate when compared 2,12 with actual BMI. It is interesting to find that this problem of overestimation of body weight was less severe in the female patients than in the controls. The difference may be accounted for by the higher prevalence of obesity in the patient group.
There are no local data concerning body weight perception in individuals with psychotic disorders. Research done in the United States studied the accuracy of body image perception in a group of patients with schizophrenia with a mean age of 50 years and of whom 91% were male.5 We found that the patient group was more likely to be obese and to underestimate their body size independent of the effects of obesity. In general, the patient group had a higher BMI than the control group. A higher prevalence of obesity was also found in patients with schizophrenia in a study in Taiwan.13 This may be related to the medications (antipsychotic medications) they are taking which cause weight gain,14 as well as the symptoms of their illness, particularly negative symptoms, which affect their motivation to exercise.15 Indeed, it has been established that the prevalence of obesity is increased in young patients with schizophrenia.16
In older patients there is a danger that they may underestimate their body size, which increases the risk of obesity. Our study found that young adults with psychotic disorders are actually aware of their body weight status. Like other young adults, they long for a slim body. Dissatisfaction with self-perceived fatness may not only induce unnecessary weight reduction behaviours, it may also lead to poor medication adherence, which will affect the prognosis of their illness.17 Awareness of this misperception concerning body weight status is important in psychiatrists working with young adults with psychotic disorders. In actual clinical practice, it is always important to identify co- existing eating disorders. Correction of the misperception is certainly beneficial to the therapeutic alliance, particularly as a means of promoting medication adherence.
The wish to lose or gain weight is driven by one’s perception of how fat or thin one is. This may not be related to actual body size. Successful weight reduction programmes can only be implemented if the participants are aware of their overweight status. As all overweight patients in this study were dissatisfied with their body weight, advice concerning proper weight reduction would be beneficial and important for them. Various methods that can be used include substituting weight-inducing antipsychotics with other suitable antipsychotic medications and involving the patient in a suitable weight loss programme.18 There are few strategies available for dealing with overweight patients with first-episode psychosis in Hong Kong. This study highlights the attitude of young adults with psychotic disorders towards their body weight and weight reduction.
This study has several limitations. First, there is an inherent problem with the use of self-reported data for calculating BMI in the control group. Previous studies have shown a tendency to over-report height and under-report weight in adolescents.12 Nevertheless, teachers measured the height and weight at school and the students were asked to record the data in the questionnaire. This should increase the reliability of the data. A second limitation is that all members of the patient group were recruited from the EASY clinic at a regional hospital in Hong Kong, making them much younger and with a shorter duration of psychotic disorders (mean duration, 2 years) than most patients with psychotic disorders. The results cannot therefore be generalised to patients with psychotic disorders of different age-groups. Thirdly, the controls were assessed by self-rated questionnaires only, making it possible that psychopathologies were missed. It is possible that there were subjects with eating disorders among the control group, thus affecting the results, although the high sensitivity of the SCOFF questionnaire should have minimised this effect. Fourthly, no formal symptom severity rating was performed to assess the patient group, so any association between the findings and symptom severity could not be evaluated. Fifthly, the control group all belonged to the same local secondary school. It would be better if more sources were available for comparison so that the control group would be more representative of the local secondary school population. Lastly, more of the patients than controls were overweight. If the BMI of the control group could be matched with the patient group, a better comparison of weight perception could be made.
This study shows that young patients with psychotic disorders overestimate their body size, particularly when they are female, and will be dissatisfied with their body size even though they are considered normal by local standards. There is not much information concerning co-existing eating disorders in patients with psychotic disorders, nor on the likely consequences of misperception of body size in patients with psychotic disorders, particularly about medication adherence. It would be worthwhile to study the effect of weight gain on weight perception in patients with psychotic disorders. Studies directly exploring those ideas would be beneficial for improving the prognosis of young patients with psychotic disorders.
Acknowledgements
We would like to thank Dr Timothy Yeung and Dr Eric Cheung for their expert opinion, as well as Mr William Wong for statistical advice. We gratefully acknowledge Prof ME Collins and Dr MY Shih for giving their permission to use their assessment scales.
References
- Shih MY, Kubo C. Body shape preference and body satisfaction in Taiwanese college students. Psychiatry Res 2002;111:215-28.
- Cheung PC, Ip PL, Lam ST, Bibby H. A study on body weight perception and weight control behaviours among adolescents in Hong Kong. Hong Kong Med J 2007;13:16-21.
- Strassnig M, Brar JS, Ganguli R. Self-reported body weight perception and dieting practices in community-dwelling patients with schizophrenia. Schizophr Res 2005;75:425-32.
- Chang VW, Christakis NA. Self-perception of weight appropriateness in the United States. Am J Prev Med 2003;24:332-9.
- Loh C, Meyer JM, Leckband SG. Accuracy of body image perception and preferred weight loss strategies in schizophrenia: a controlled pilot study. Acta Psychiatr Scand 2008;117:127-32.
- Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 1999;319:1467- 8.
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-63.
- Ko GT, Tang J, Chan JC, Sung R, Wu MM, Wai HP, et al. Lower BMI cut-off value to define obesity in Hong Kong Chinese: an analysis based on body fat assessment by bioelectrical impedance. Br J Nutrition 2001;85:239-42.
- Leung SS, Cole TJ, Tse LY, Lau JT. Body mass index reference curves for Chinese children. Ann Hum Biol 1998;25:169-74.
- Mok PW, Wong WH, Lee PW, Low LC. Is teenage obesity associated with depression and low self-esteem?: a pilot study. Hong Kong J Paediatr (new series) 2008;13:30-8.
- Collins ME. Body figure perceptions and preferences among preadolescent children. Int J Eat Disord 1991;10:199-208.
- Brener ND, Mcmanus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. J Adolesc Health 2003;32:281-7.
- Hsiao CC, Ree SC, Chiang YL, Yeh SS, Chen CK. Obesity in schizophrenic outpatients receiving antipsychotics in Taiwan. Psychiatry Clin Neurosci 2004;58:403-9.
- Casey DE, Zorn SH. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry 2001;62(Suppl 7):S4-10.
- Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychol Med 1999;29:697-701.
- Theisen FM, Linden A, Geller F, Schäfer H, Martin M, Remschmidt H, et al. Prevalence of obesity in adolescent and young adult patients with and without schizophrenia and in relationship to antipsychotic medication. J Psychiatr Res 2001;35:339-45.
- Weiden PJ, Mackell JA, McDonnell DD. Obesity as a risk factor for antipsychotic noncompliance. Schizophr Res 2004;66:51-7.
- Malhi GS, Mitchell PB, Caterson I. ‘Why getting fat, Doc?’ Weight gain and psychotropic medications. Aust N Z J Psychiatry 2001;35:315-21.