Hong Kong J Psychiatry 2008;18:49-54
Original Article
Cognitive-behavioural Therapy by Novices for Supervised Community Hostel Residents with Treatment-resistant Schizophrenia in Hong Kong: a Pilot Study
資淺的治療師以認知行為療法,治療社區院舍中抗精神病藥物的精神分裂病人的一項先導研究
Dr Roger MK Ng, MBChB (CUHK), MSc (Birm), MRCPsych (UK), FHKAM (Psychiatry), FHKCPsych, Department of Psychiatry, 7/F, Main Block, Kowloon Hospital, Argyle Street, Hong Kong, China.
Dr LK Hui, MBChB (CUHK), MRCPsych (UK), Department of Psychiatry, 7/F, Main Block, Kowloon Hospital, Argyle Street, Hong Kong, China.
Dr L Pau, MBChB (CUHK), Department of Psychiatry, 7/F, Main Block, Kowloon Hospital, Argyle Street, Hong Kong, China.
7/F, Main Block, Kowloon Hospital, 147A, Argyle Street, Hong Kong, China. Tel: (852) 3129 7111; Fax: (852) 2711 4601;
E-mail: rmkng@netvigator.com
Submitted: 5 November 2007; Accepted: 7 December 2007
Abstract
Objective: Despite extensive research in cognitive-behavioural therapy (CBT) for psychosis in the United Kingdom and the United States, there are very limited data about its efficacy in other parts of the world. This pilot study aimed to investigate the efficacy of CBT by novice therapists (mainly social workers) for regularly supervised community hostel residents with treatment-resistant psychotic symptoms.
Participants and Methods: Ten novice CBT therapists with a social work background provided weekly individual CBT to a group of hostel residents, who had an ICD-10 diagnosis of schizophrenia and with persistent psychotic symptoms despite adequate medication. Before the commencement of CBT, the severity of psychotic symptoms, emotions associated with psychosis (depression, anger, and anxiety), insight, and self-esteem were measured. The measurements were repeated after 6 months of CBT.
Results: At the end of the sixth month, there was a reduction in the severity of psychotic symptoms (as measured by the Positive and Negative Syndrome Scale, and Psychotic Symptom Rating Scale) and improvement in self-esteem. However mood symptoms and insight level remained relatively unchanged.
Conclusion: Cognitive-behavioural therapy conducted by novice therapists under regular supervision may be useful in reducing symptoms and distress in a group of supervised community hostel residents in Hong Kong. Due to the small sample size and other methodological limitations, this conclusion is only tentative. A randomised controlled trial is warranted to confirm these preliminary finding.
Key words: Cognitive therapy; Community mental health services; Psychotic disorders
摘要
目的:雖然一些國家己廣泛研究以認知行為療法治療精神病,但對於此療法在其他國家的效果,資料卻十分有限。本先導研究探討資淺的治療師,以認知行為療法治療抗精神病藥物的精神分裂病人的效果,對象為在社區宿舍居住的病人。
參與者與方法: 十名擁有社會工作者背景的資淺治療師,每星期為住院病人進行個別的認知行為治療。這些病人被診斷為患有「國際疾病分類ICD-10編碼」中的精神分裂症,即使服食足量藥物仍出現長期精神病徵狀。在治療開始前和治療六個月後,病人接受精神病徵狀的評估(抑鬱、憤怒、焦慮)、自知力和自尊心。
結果: 治療六個月後,用「陰性和陽性症狀量表」和「精神病徵狀評定量表」量度,病人的精神病徵狀得到舒緩,自尊心亦有所提高,但情緒病徵和自知力則維持不變。
結論:以定期指導的方式訓練香港資淺治療師,替病人作認知行為治療有助減低病人的徵狀和憂慮。由於本研究對象數目較少和方法學上的限制,上述結論只屬初步,需要進行隨機對照試驗方能作出確認。
關鍵詞:認知療法、社區精神健康服務、思覺失調
Introduction
Cognitive-behavioural therapy also appears to reduce psychotic symptom severity, speed up recovery from acute psychosis,14,15 enhance medication adherence,16 and be an efficacious adjunct for treating psychosis, although there are still unanswered questions as to its impact on relapse, quality of life, and violent behaviour.17 However, most of these studies were conducted in the West and in Caucasian populations. Thus, it is not clear whether CBT (a short-term individual-directed psychological treatment emphasising collaboration, scientific empiricism, and Socratic dialogue) would be equally acceptable and applicable to non- western populations. Notably, recent studies support the value of CBT for some psychiatric disorders in Chinese populations,18-20 but there are no data with regard to Chinese patients suffering from psychosis. This was therefore a preliminary study to investigate the effectiveness of CBT in patients suffering from treatment-resistant schizophrenia. Furthermore, if an empirically validated psychological treatment is to be delivered to a full range of sufferers of schizophrenia in the community, then such an intervention must have demonstrably worthwhile clinical outcomes.13
The largest workforce in regular contact with patients with schizophrenia consists of mental health nurses and social workers. Cognitive-behavioural therapy conducted by mental health nurses in this setting provides clear benefits to the patients.12 Traditionally, social workers have adopted a case management approach to manage the disorder. Whether training social workers to deliver brief CBT would benefit psychotic patients with a serious disorder remains unclear. This pilot study was therefore planned, with a view to involving social workers in the community with no previous training in CBT.
Methods
Sample
Patient Recruitment
Ten patients were recruited from a community non- government organisation (NGO) serving patients with severe mental illness in Hong Kong. The patients fulfilled the following inclusion criteria: (1) age 18 to 65 years; (2) ability to read and speak Chinese; (3) resident in any halfway house run by the NGO; (4) suffering from schizophrenia, as defined by ICD-10 criteria; (5) previous treatment with at least 2 different antipsychotics (conventional or atypical antipsychotics); (6) persistent psychotic symptoms (delusions or hallucinations); (7) subjective distress or functional disabilities related to such symptoms; and (8) ability to give informed consent. Eligible patients also had to have no exclusion criteria: (1) presence of alcohol or drug abuse in the past 6 months; (2) showing active or immediate risk of violence to self or others; (3) with significant co- morbidities. The patients were selected from the caseload of each nominated therapist (see ‘Therapist Recruitment’ below) and their suitability for CBT was discussed during the first few supervision sessions (see ‘Therapist Training’ below). All the selected patients were deemed to fulfil the above inclusion and exclusion criteria, and all gave informed consent to participate in this research project.
Therapist Recruitment
The novice therapists consisted of 10 experienced professionals who were working in an NGO in Hong Kong, which provides a range of rehabilitation services for persons suffering from serious psychiatric disorders. Such services were to be provided at halfway houses, sheltered workshops, supported employment services, and community outreach establishments. The professionals were recruited for training through the recommendation of senior managers of the NGO, based on the trainees’ expressed interests in learning CBT and the nature of work. Therefore, only trainees who expressed a definite interest in learning CBT for psychosis and were caring for psychotic patients on a regular basis were selected.
Originally, 12 workers were nominated by the director and accepted for training; all were Chinese, 8 of whom were female. All were registered social workers except 1 female trainee, who was an enrolled nurse by profession; their mean age was 39 (range, 28-46) years. Three had attained a Master’s degree in Social Work, 4 a Bachelor’s degree, while 5 had graduate diplomas in Social Work. They had a mean of 7 years of experience working with psychotic patients (range, 2-12 years). At the commencement of patient recruitment, only 10 remained. All the trainees reported previous experience in providing counselling sessions to psychotic patients residing in halfway houses, considered to be in line with client-centred principles, although none had received any formal training in this respect. None had previous experience of conducting cognitive therapy for patients with psychiatric problems.
Therapist Training
The training programme21 comprised 2 phases. The first phase (didactic lectures) was a 10-week training programme lasting a total of 25 hours. The second phase (group supervision) entailed discussions about respective patients receiving CBT. The topics (and number of sessions) dedicated to the didactic phase included: (1) basic techniques for CBT (session 1); (2) cognitive formulation of delusions (session 2); (3) cognitive model of voices and negative symptoms (session 3); (4) cognitive and behavioural techniques for delusions, voices, and negative symptoms (sessions 4 to 6); (5) schema work (session 7); (6) cognitive and behavioural interventions for medication-adherence problems (session 8); (7) relapse prevention work (session 9); (8) case formulation for psychosis and its relationship with intervention strategies (session 10); (9) relationship ruptures and repair of therapeutic alliances (session 11); (10) current evidence for CBT for psychosis and brief update on other new interventions like mindfulness, and acceptance and commitment therapy (session 12). All trainees were also assigned homework (reading) after each didactic lecture, which was based on the therapist’s manual ‘Cognitive- behavioural therapy for schizophrenia’.22 Specific time was allocated before commencement of every lecture for feedback on reading assignments. The second phase comprised weekly group supervision between the trainer (first author) and those receiving supervision and lasted 6 months. Due to the work commitments, only 6 to 8 persons being supervised could attend each supervisory session, which was composed of 2 parts. First, there was a discussion of progress achieved by 2 or 3 patients and review of a therapy session / segment of a pre-determined individual being supervised. Each trainee was also required to submit every videotaped session for the record and for research purposes. One-third of the videotaped sessions (n = 30) were subjected to systematic review for compliance and fidelity checking. All sessions were confirmed to comply with the application of cognitive- behavioural techniques for psychosis.
Skills in cognitive therapy (like setting up of behavioural experiments and completion of dysfunctional thought records) were discussed in both didactic and group supervision sessions. In group supervision sessions, such skills were explicitly focused and coached, using role-plays and role-reversals. Cognitive therapy skills (what, how, and when to apply certain skills) were implemented with explicit referral to the case formulation of each patient. The review of a pre-determined videotaped sessions with trainees provided a particularly important experiential exercise, as trainees were encouraged to provide constructive comments on the performance among themselves, and on role-play of a problematic segment. Such role-play would then be followed up by extensive discussion of the problems experienced by the patient and the therapist.
The trainer was a psychiatrist with over 16 years of clinical experience with psychotic patients. Being a certified cognitive therapist and cognitive therapy trainer / supervisor, he was experienced in CBT for psychosis, and in supervising psychiatric trainees in the application of CBT. This was the first of the group supervision and training course for social workers on CBT for psychosis organised by the trainer.
Intervention
The intervention consisted of weekly individual psychological treatment conducted according to the principles of cognitive therapy and lasted 6 months. There were several essential ingredients in CBT — (1) time limitation: 12- to 16-weekly 1-hour sessions; (2) collaboration: emphasising exploration rather than direct teaching; (3) homework assignment; and (4) feedback encouraged after every session. Due to the cognitive deficits or paranoid attitudes common to patients with psychosis, modifications were often made: (1) the first few sessions might be shorter but more frequent (once every 2 to 3 days) to enhance engagement; (2) unequal collaboration, with the therapist taking a more active role in the sessions; (3) homework could be less structured and simpler. The interventions could be summarised as having 3 phases. The early phase (sessions 1 to 5) focused on engagement, identification of goals and targets of intervention, and collection of data for construction of case formulation. The middle phase (sessions 6 to 11) was directed at behavioural strategies to cope with distressing emotions due to voices or delusions, and entailed problem-solving skills, behavioural experiments to examine the validity of delusions, behavioural / cognitive strategies to deal with the identity and power of voices, and the identification of life goals and steps to attain them. The final phase (sessions 12 to 16) entailed discussions about medication adherence and relapse prevention strategies. ‘Cognitive-behavioural therapy for schizophrenia’22 was used as the reference source for this pilot study.
Assessors
Assessments were conducted 4 to 6 weeks before delivery of CBT, and within 4 to 6 weeks after termination. Observer- rated assessments were conducted by the second and third authors (LKH & LP), and the first author’s research assistant (for another research project). The 3 raters were not involved in the intervention or training of the therapists. All raters achieved a criterion inter-rater reliability of more than 0.85 in all the observer-rated assessments with the first author (RMK), who was an experienced researcher in using all the observer-rated assessments. Two raters (LKH & LP) were experienced psychiatrists, working with patients suffering from psychosis for more than 5 years, while the research assistant was a psychology graduate student.
Assessment
Psychotic Symptoms
General psychopathology was measured using the Positive and Negative Syndrome Scale (PANSS),23 which consists of 3 subscales — the positive, the negative, and the general. The scale has 30 seven-point items, each item rating from 1 (absent) to 7 (extremely severe) according to the manual instructions. Thus, both the positive and negative subscales contain 7 items each, and each can yield scores ranging from 7 to 49. The general psychopathology subscale contains 16 items, whose total scores could range from 16 to 112. The total PANSS score could therefore range from 30 to 210, with higher scores indicating more severe psychopathology. The PANSS is an observer-rated scale requiring some training.
The degree of distress, preoccupation, and emotional investment were measured by the Psychotic Symptom Rating Scale (PSYRATS).24 The PSYRATS consists of 2 subscales: for auditory hallucination and delusion. The 11 auditory hallucination items assess different dimensions of auditory hallucinations over the past week, which can be clustered into 3 factors — physical characteristics, emotional characteristics, and cognitive interpretation. Each item is rated from 0 to 5, with higher ratings for greater severity. The delusion subscale, which consists of 6 items, can be clustered into 2 factors — cognitive interpretation and emotional characteristics; in which each item can be rated from 0 to 5; higher scores indicating greater severity. The psychometric properties of PSYRATS have been extensively researched and both scales have excellent inter-rater reliability and good validity. The inter-rater reliability for PSYRATS was found to be uniformly high for all delusion scale items (intra-class correlation ranging from 0.884 to 1.000) and auditory hallucination scale items (intra-class correlation ranging from 0.788 to 1.000).24 Like working with PANSS, this is an observer-rated scale requiring some training.
Insight
Insight was measured by the scale to assess unawareness of mental disorder (SUMD25). The SUMD is a semi-structured interview that assesses awareness of illness. In turn, the first 3 items assess the subject’s general awareness of a mental disorder (SUMD1), the effects of medication on the disorder (SUMD2), and a general understanding of the consequences of the disorder (SUMD3). These 3 items are asked of all subjects, and their level of awareness (current and past) is rated on a 5-point Likert scale (1 = full awareness and 5 = full unawareness). Items 4 to 20 pertain to specific symptoms, such as delusions, hallucinations, thought disorder, alogia, avolition, and flat affect, and are only pursued if established via chart reviews and interviews with the treating clinical psychologist or psychiatrist. Corresponding subjects are then asked if they have experienced the symptom either currently or in the past, using the same 5-point Likert scale. If the subject shows awareness of a symptom, defined as a score of between 1 (full awareness) and 3 (partial awareness), the subject’s attribution of the symptom is assessed and rated on a 5-point Likert scale (1 = correct attribution and 5 = incorrect attribution). The inter-rater intra-class correlation (ICC) was 0.95 and test-retest ICC was 0.62 for the first item, the general insight measure, i.e. awareness of mental disorder. The other insight items all had excellent inter-rater ICCs (range, 0.76-0.99; median, 0.89) and fair to good test- retest ICCs (range, 0.36-0.80; median, 0.51). For this study, only the first 3 items of the SUMD were asked to assess a general level of insight. In a local study on the relationship between level of insight and deficit syndrome, the SUMD was found to be reliable and valid in a sample of Hong Kong Chinese outpatients suffering from schizophrenia.26
Mood Symptoms
Depressive symptoms were assessed by the Chinese version of Beck Depression Inventory (BDI-II27). The BDI-II is a 21-item self-report rating inventory measuring characteristic attitudes and symptoms of depression. The score ranges from 0 to 63. A total score below 8 is regarded as normal, while a score exceeding 21 is strongly suggestive of clinical depression.28
The Beck Anxiety Inventory (BAI29) was used to measure the severity of anxiety. The BAI scale consists of 21 items. Respondents were asked to rate how much they were bothered by anxiety symptoms over the past week on a 4-point scale ranging from 0 to 3. The items were summed to obtain a total score, ranging from 0 to 63; higher score suggesting higher levels of anxiety. The scale’s psychometric properties have been reported,29 and suggest good reliability and validity.
The degree of anger was measured by the Novaco Anger Inventory (NAI)–Short Form.30 The NAI-Short Form was adapted from the long form31 and contains 25 of the original 90 items. The NAI–Long Form purports to measure the degree of provocation or anger persons would feel, if placed in certain situations. The NAI–Long Form scale displays a convergent validity of 0.46 with the Buss-Durke Hostility Inventory, and 0.41 with the Aggression subscale of the Personality Research Form32 and has a test-retest reliability of between 0.78 and 0.91.33 In order to ascertain the validity of the NAI–Short Form, a factor analysis was applied to the full data set at intake (n = 207) and 4 factors with an eigenvalue above 1.00 were derived. However, 1 factor derived an eigenvalue of 12.62 and accounted for over 50% of the variance. Only 1 item had a higher factor loading on any of them other than factor 1. The factor loadings for factor 1 ranged between 0.53 and 0.79, with an average loading of 0.71. It is therefore suggested that this scale should consist of only 1 factor (anger). A Cronbach’s alpha of 0.96 was derived for the scale with an average inter- item correlation of 0.49, an item-total correlation of between 0.50 and 0.77, and a split-half reliability of 0.93. The Short Form was translated into Chinese by a qualified translator and then back-translated into English by the first author. The NAI (translated Chinese version) was used in this study.
Self-esteem
The self-esteem of each participant was measured by a Chinese version of the Rosenberg Self-esteem Scale (RSS).34,35 The RSS questionnaire is self-administered, and comprises 10 questions — 5 of which are worded as affirmatives and 5 are in a negative direction. The total score ranges from 10 to 40, with higher scores indicating higher self-esteem. The RSS has been found to have high test-retest reliability of 0.87 and good internal consistency with a Cronbach’s alpha coefficient exceeding 0.80.34
Statistical Analysis
Results were analysed using the Statistical Package for Social Sciences Windows version 11.36 Differences between the pre- and the post-intervention conditions were calculated using paired t tests, after checking for normality of the distribution of the various outcome measures.
Results
Baseline Demographics
Ten patients were recruited for this pilot study, with a mean age of 44 (standard deviation [SD], 15) years; 5 were male. They had been ill for a mean duration of 12 (SD, 7) years and had a median of 3 previous admissions to psychiatric hospitals. Four were in receipt of atypical antipsychotics, while 6 were taking conventional antipsychotics (mean chlorpromazine equivalent dosage, 730 mg/day; SD, 218 mg/day), indicating relatively high dosage therapy with antipsychotics. None of the patients had a history of receiving any form of psychotherapy.
Therapist Competence
Therapist competence was reported in a separate paper.37 In brief, the mean total score of Cognitive Therapy Rating Scale (CTRS38) was 31 at the commencement of group supervision. By the end of 6-month group supervision training, there was an improvement in mean total score to 34. None of the therapist was able to achieve the minimum requirement of a ‘competent therapist’, defined by attainment of a total score of more than 44.
Psychotic Symptoms
There was a significant improvement in the positive and negative symptoms, as measured by PANSS.23 There was a corresponding reduction in the delusion hallucination subscales over the 6-month intervention period. The reductions are shown in Table 1.
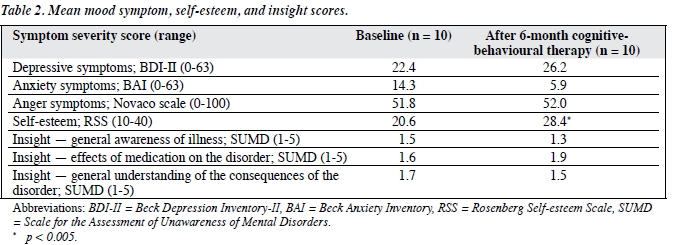
Mood Symptoms, Insight, and Self-esteem
After the 6-month intervention, there was a corresponding improvement in self-esteem. Nevertheless, there was little change in the level of depressive, anxiety, and anger symptoms, and relatively little change in the level of insight as measured by SUMD. The results are shown in Table 2.
Discussion
This was the first local longitudinal study on the efficacy of CBT for psychosis in Hong Kong. The subjects recruited were patients suffering from chronic schizophrenia and residing in supervised community residences. Their levels of disabilities were more severe than in outpatients living with family members or independently. This was a small study with many methodological limitations. The sample was small and non-random. The assessors were not blinded to the interventions for the patients, though they had no prior training or knowledge about the efficacy of CBT for psychosis. Although one-third of the videotaped sessions were reviewed by the trainer using cognitive-behavioural techniques, it was possible that some of the other two-thirds were not truly CBT in nature. The absence of a control intervention like supportive psychotherapy could not rule out a possible placebo effect of enhanced individual attention, to explain the improvement in objective negative and positive symptoms, as well as the improved self-esteem.
The failure of novice therapists to attain levels of competence necessary for a cognitive therapist as measured by CTRS is not surprising, as they were only supervised to treat 1 patient each. However it is encouraging that they were assessed to have improved in competence level from 31 to 34, which is quite meaningful.21 Notably, in a UK study12 involving CBT provided by mental health nurses, the interventions were assessed to be meaningful and of significant value in reducing psychotic symptoms in their sample of patients with treatment-resistant psychotic symptoms. Their findings were also in line with this study. However, given the methodological limitations discussed above, our results should still be regarded as extremely tentative. Our study may therefore serve as a pilot project for conducting a more definitive randomised controlled trial of CBT for psychotic patients in Hong Kong.
Acknowledgements
We would like to thank the 2 anonymous reviewers for their helpful comments. In addition, we thank all the therapists and patients involved in this pilot study, without whom this study could not have been conducted at all. We also express our gratitude to Dr Timothy Chan, Executive Director of Richmond Fellowship, for facilitating the project.
References
- Kuipers E, Garety P, Fowler D, Dunn G, Bebbington P, Freeman D, et al. London-East Anglia randomised controlled trial of cognitive- behavioural therapy for psychosis. I: effects of treatment phase. Br J Psychiatry 1997;171:319-27.
- Tarrier N, Yusupoff L, Kinney C, McCarthy E, Gledhill A, Haddock G, et al. Randomised controlled trial of intensive cognitive behaviour therapy for patients with chronic schizophrenia. BMJ 1998;317:303-7.
- Chadwick P, Birchwood M. The omnipotence of voices. A cognitive approach to auditory hallucinations. Br J Psychiatry 1994;164:190-201.
- Gumley A, O’Grady M, McNay L, Reilly J, Power K, Norrie J. Early intervention for relapse in schizophrenia: results of a 12-month randomized controlled trial of cognitive-behavioural therapy. Psychol Med 2003;33:419-31.
- Sensky T, Turkington D, Kingdon D, Scott JL, Scott J, Siddle R, et al. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry 2000;57:165-72.
- Lewis S, Tarrier N, Haddock G, Bentall R, Kinderman P et al. Randomised controlled trial of cognitive-behavioural therapy in early schizophrenia: acute-phase outcomes. Br J Psychiatry 2002;181(Suppl 43):S91-7.
- Valmaggia LR, van der Gaag M, Tarrier N, Pijnenborg M, Slooff CJ. Cognitive-behavioural therapy for refractory psychotic symptoms of schizophrenia resistant to atypical antipsychotic medication. Randomised controlled trial. Br J Psychiatry 2005;186:324-30.
- Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O’Brien R, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J Psychiatry 2001;158:1706-31.
- Morrison AP, French P, Walford L, Lewis S, Kilcommons A, Green J, et al. Cognitive therapy for the prevention of psychosis in people at ultra- high risk: randomised controlled trial. Br J Psychiatry 2004;185:291-7.
- Turkington D, Kingdon D. Cognitive-behavioural techniques for general psychiatrists in the management of patients with psychoses. Br J Psychiatry 2000;177:101-6.
- 1 Turkington D, Kingdon D, Turner T; Insight into Schizophrenia Research Group. Effectiveness of a brief cognitive-behavioural therapy interven- tion in the treatment of schizophrenia. Br J Psychiatry 2002;180:523-7.
- Turkington D, Kingdon D, Rathod S, Hammond K, Pelton J, Mehta R. Outcomes of an effectiveness trial of cognitive-behavioural intervention by mental health nurses in schizophrenia. Br J Psychiatry 2006;189:36-40.
- Turkington D, Kingdon D, Chadwick P. Cognitive-behavioural therapy for schizophrenia: filling the therapeutic vacuum. Br J Psychiatry 2003;183:98-9.
- Drury V, Birchwood M, Cochrane R, MacMillan F. Cognitive therapy and recovery from acute psychosis: a controlled trial. I. Impact on psychotic symptoms. Br J Psychiatry 1996;169:593-601.
- Drury V, Birchwood M, Cochrane R, MacMillan F. Cognitive therapy and recovery from acute psychosis: a controlled trial. II. Impact on recovery time. Br J Psychiatry 1996;169:602-7.
- Kemp R, Hayward P, Applewhaite G, Everitt B, David A. Compliance therapy in psychotic patients: randomised controlled trial. BMJ 1996;312:345-9.
- Kuipers E. Evaluation of cognitive behaviour therapy for psychosis. Clinical Psychology: Science and Practice 2005;12:65-7.
- Lee JY, Choy CH. The effects of cognitive-behavioural and exposure therapy for social anxiety. Korean J Counsel Psychother 1997;9:35-56.
- Ng R, Cheung M, Suen L. Cognitive-behavioural therapy for psychosis: an overview and three case studies from Hong Kong. Hong Kong J Psychiatry 2003;13:26-33.
- Ng R. Cognitive therapy for obsessive-compulsive personality disorder — a pilot study in Hong Kong Chinese patients. Hong Kong J Psychiatry 2005;15:50-3.
- Ng R, Cheung M. Supervision of cognitive behavioral therapy for psycho- sis: a Hong Kong experience. Hong Kong J Psychiatry 2007;17:124-30.
- Kingdon D, Turkingdon D. Cognitive-behavioural therapy for schizophrenia. 2nd ed. New York: Guildford; 2005.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76.
- Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med 1999;29:879-89.
- Amador XF, Flaum M, Andreasen NC, Strauss DH, Yale SA, Clark SC, et al. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry 1994;51:826-36.
- Kwan KL. Relationship of insight and deficit syndrome in chronic schizophrenia [thesis]. Hong Kong: Hong Kong College of Psychiatrists; 2006.
- Beck, AT, Steer, RA, Brown, GK. The Beck Depression Inventory — Second Edition. Psychological Corporation; San Antonio, TX; 1996.
- Beck AT, Steer RA, Garbin, MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 1988;8:77-100.
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-7.
- Devilly GJ. The psychological effects of a lifestyle management course on war veterans and their spouses. J Clin Psychol 2002;58:1119-34.
- Novaco RW. Anger control: the development of an experimental treatment. Lexington, KY: Lexington; 1975.
- Huss MT, Leak GK, Davis SF. A validation study of the Novaco Anger Inventory. Bull Psychon Soc 1993;31:279-81.
- Mills JF, Kroner DG, Forth AE. Novaco Anger Scale: reliability and validity within an adult criminal sample. Assessment 1998;5:237-48.
- Rosenberg M. Society and adolescent self-image. Princeton, NJ: Princeton University Press; 1965.
- Lee S, Lee AM. Disordered eating in three communities in China: a comparative study of female high school students in Hong Kong, Shenzen, and rural Hunan. Int J Eat Disord 2000;27:317-27.
- Statistical package for social science. SPSS for Windows, Release 11. Chicago, Ill: SPSS; 2001.
- Ng RM, Cheung MS. Supervision of cognitive behavioural therapy for psy- chosis: a Hong Kong experience. Hong Kong J Psychiatry 2007;17:124-30.
- Vallis TM, Shaw BF, Dobson KS. The Cognitive Therapy Rating Scale: psychometric properties. J Consult Clin Psychol 1986;54:381-5.