Hong Kong J Psychiatry 2008;18:76-80
Original Article
Efficacy of Pharmacotherapy and Cognitive Therapy, Alone and in Combination in Major Depressive Disorder
以藥物治療、認知療法,以及混合療法醫治抑鬱症的效用
F Shamsaei, A Rahimi, MK Zarabian, M Sedehi
Dr F Shamsaei, Department of Psychiatric Nursing, Behavioural Disorders & Drug Substances Research Center, Hamadan University of Medical Sciences, Iran.
Dr A Rahimi, Department of Psychiatry, Behavioural Disorders & Drug Substances Research Center, Hamadan University of Medical Sciences, Iran.
Dr MK Zarabian, Behavioural Disorders & Drug Substances Research Center, Hamadan University of Medical Sciences, Iran.
Dr M Sedehi, Department of Biostatistics, Hamedan University of Medical Sciences, Iran.
Address for correspondence: Dr F Shamsaei, Faculty of Nursing, Hamadan
University of Medical Sciences, Hamadan 65178, Iran. Tel: 98-811 8276051; Fax: 98-811 8276052;
E-mail: shamsaei68@yahoo.com
Submitted: 8 February 2008; Accepted: 9 April 2008
Abstract
Objective: To assess the efficacy of pharmacotherapy (citalopram) and cognitive therapy alone, or in combination for the treatment of major depressive disorder.
Participants and Methods: This study was a randomised controlled clinical trial. In all, 120 adults with a major depressive disorder were assigned to an 8-week treatment with either citalopram, cognitive therapy, or both. Major depressive disorder was diagnosed using DSM-IV criteria. Patients were assessed with the Beck Depression Inventory before and after treatment.
Results: Statistical analysis showed that cognitive therapy, pharmacotherapy, and combined therapy were effective in the treatment of depression. There was no significant difference between the effects of medication and cognitive therapy. Combined treatment with the cognitive therapy and citalopram yielded better responses than treatment with citalopram or cognitive therapy alone.
Conclusion: Although antidepressant treatment or cognitive therapy effectively reduces the clinical symptoms and functional impairment associated with major depressive disorder, combination treatment is more efficacious.
Key words: Pharmacotherapy; Cognitive therapy; Depressive disorder
摘要
目的:評估軍以西酞普蘭作藥物治療或認知療法, 以及混合療法醫治抑鬱症的效用。
參與者與方法: 以隨機控制臨床測試,把1 20名抑鬱症成人患者分成純西酞普蘭療法、認知療法,及混合療法三組,全部接受8星期治療。抑鬱症根據《精神疾病診斷準則手冊》第四版的標準診斷,並以Beck 抑鬱量表評估患者治療前後的效果。
結果:統計學分析顯示,認知療法、藥物治療和混合療法均有效治療抑鬱症。藥物治療和認知療法並無顯著分別 ;與上述兩種比較,混合療法的效果較佳。
結論:雖然抗抑鬱劑治療或認知療法能有效減少臨床徵狀和與抑鬱症相關的功能缺損,但混合療法仍是較佳的選擇。
關鍵詞:藥物治療、認知療法、抑鬱症
Introduction
Antidepressant medications (ADMs) are the most widely used treatments for major depressive disorder.1 Evidence from randomised placebo-controlled trials has supported their efficacy, particularly for more severely depressed patients.2 Cognitive therapy pioneered by Beck et al has also shown promise in the treatment of major depressive disorder.3,4 In a randomised, comparative trial, Rush et al5 reported that cognitive therapy was more effective than ADM. However, their ADM dosages were low and the medications were tapered 2 weeks before final outcome assessment. Despite these shortcomings, their findings generated enthusiasm for cognitive therapy as an alternative to ADM for the treatment of depression.
Discussion of the comparative efficacy of ADM and cognitive behaviour therapy for the treatment of severely depressed patients has been marked by controversy. Findings from early comparative studies led many to conclude that cognitive behaviour therapy is at least as effective as ADM for the acute treatment for depression.5-8 However, other reports suggested that it is not an effective treatment for severely depressed patients.9-13 Findings from yet other randomised trials of ADM and cognitive behaviour therapy also need to be considered. Using criteria and measures employed by Elkin et al,9 Hollon et al14 found a very small advantage for cognitive behaviour therapy in their more severely depressed subgroup. This finding was at odds with the Treatment of Depression Collaborative Research Program, in which ADM outperformed cognitive behaviour therapy among the more severely depressed patients.15 To examine the effects of both pharmacotherapy and cognitive therapy, we conducted a clinical trial comparing the 3-month efficacy of cognitive therapy and pharmacotherapy with that of combined therapy in patients with major depressive disorder of mild or moderate severity, defined according to DSM-IV criteria.16
Methods
Study Sample
The study sample consisted of consecutive new patients referred to 2 outpatient clinics of the Farshchian psychiatric centre in Hamadan, Iran. Farshchian psychiatric centre is a large psychiatric facility with several inpatient and outpatient clinics, covering a third of the population of Hamadan city. A total of 204 patients were screened. Of the 84 who did not undergo randomisation, 36 did not meet the study entry criteria (given below), 19 withdrew their consent, and 29 were excluded for other reasons (failure to return for further evaluation or non-compliance). One hundred and twenty patients underwent randomisation—40 were assigned to receive citalopram, 40 received cognitive therapy, and 40 received combined treatment.
Diagnosis was based on the DSM-IV,16 with the Structured Clinical Interview for Axis I DSM-IV Disorders.17 The inclusion criteria were: age 18-65 years, first visit after onset of depressive disorder, and not being in receipt of any prior therapy. Patients were excluded from the study if they had any of the following: a history of seizures, abnormal findings on electroencephalography, severe head trauma, or stroke; evidence suggesting high risk of suicide; a history of psychotic symptoms or schizophrenia; bipolar disorder, an eating disorder (if not in remission for at least 1 year), obsessive-compulsive disorder, or dementia; antisocial, schizotypal, or severe borderline personality disorder; a principal diagnosis of panic, generalised anxiety, social phobia, or post-traumatic stress disorders or any substance- related abuse or dependence disorder (except those involving nicotine) within the last 6 months.
Study Design
This study was approved by the institutional review board at each study centre. All patients provided written informed consent. According to a central computerised randomisation schedule, patients who remained eligible at the end of a 2- week evaluation period were assigned to receive citalopram, cognitive therapy, or a combination of citalopram and cognitive therapy, in a 1:1:1 ratio.
Pharmacotherapy
Pharmacotherapy for mild and moderately depressed patients was initiated in the outpatient clinic at the standard dosage of citalopram (20 mg / day) used in Farshchian psychiatric centre. The treatment continued for 8 weeks, with a focus on medication management, education about medications, adjustment of dosage and dosage schedules as necessary, and discussions about adverse effects.
Cognitive Therapy
This was aimed at reducing the participant’s level of depression and increasing his / her coping skills, and entailed 8 sessions of therapy. The first half of each session was devoted to presenting a social learning view of depression and guidance on learning how to identify and differentiate mood states. The second half addressed acquiring skills in 3 specific areas: increasing pleasant activities, changing negative cognitions, and improving social skills to increase positive social interactions. Each participant was encouraged to develop a personalised plan to work on problem areas by means of a participant workbook. Each session entailed a review of material from the previous session, presentation of new material, discussion, exercises related to the new material, and a homework assignment. The treatment was administered in 60-minute individual sessions by a single therapist, who was a psychiatric nurse.
Measurement
Patients were assessed with the Beck Depression Inventory (BDI) before and after treatment.18
Statistical Analysis
Analysis of covariance, including the initial measures as co- variants, and multivariate analyses of variance were used to test intra- and inter-group differences. In addition, for each group pre- and post-effect sizes and comparative effect sizes were calculated as the standard difference between 2 means, using the pooled standard deviation as denominator.19-22 The t test was used for comparative mean scores of the BDI pre- and post-treatment results in the 3 groups.
Results
The mean age of the participants was 36 years (standard deviation, 11 years). There was no significant difference in the demographic, social, and clinical characteristics between the 3 treatment groups (Table 1).
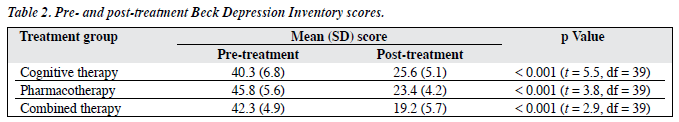
Mean pre- and post-intervention BDI scores of the 3 treatment groups are shown in Table 2. Analyses revealed significant improvements in post-intervention scores (after 8 weeks) in all 3 patient groups (t test, p < 0.001).
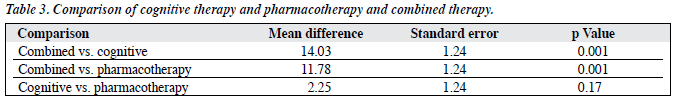
One-way analysis of variance showed significant differences between the combined treatment group and those who received only cognitive therapy, or only citalopram (p < 0.001). However, there was no significant difference between the citalopram and cognitive therapy groups. The magnitude of responses was significantly greater in the combined treatment group than in the pharmacotherapy or the cognitive therapy groups (p < 0.001; Table 3).
Discussion
Previous reports suggested that the tricyclic antidepressant, monoamine oxidase inhibitors, and selective serotonin reuptake inhibitors are effective in the treatment of depression. Several reports also highlighted the efficacy of cognitive therapy in the treatment of depression.22-34
The present study confirmed that an 8-week treatment course with citalopram or cognitive therapy effectively reduced the symptoms of depression. We also showed that cognitive therapy alone was similar in efficacy to citalopram treatment.
We also found that combined treatment (citalopram + cognitive therapy) offered significant advantages over either treatment alone. Our results seem to concur with those of Keller et al,32 who reported a superior efficacy of combined therapy over psychotherapy. Certain depressive symptom may respond differently to treatment by cognitive therapy than to standard ADM.5,35 After successful relief of their symptoms following pharmacotherapy, many depressed patients seem to require psychotherapy to cope with the problems of living arising in relation to their depression.36
Our study should be interpreted in the context of its limitations. For the BDI, a self-reported questionnaire was used to measure outcomes (clinical responses). Second, though randomised treatment allocation to the 3 groups was used, the present study was non-blinded. Third, an 8-week treatment may be inadequate to detect delayed responses, particularly from psychological treatment. Fourth, responses might have differed with higher doses of antidepressants. In summary, we found that for patients with major depressive disorder, the combination of antidepressant pharmacotherapy and the cognitive therapy was significantly more efficacious than either treatment alone. The response to either treatment alone was similar to the rates reported in previous trials for the treatment of major depression.
Acknowledgement
This research was carried out by a grant from Hamadan University of Medical Sciences.
Declaration
The authors declare that there was no pharmaceutical sponsorship in conducting this trial.
References
- Olfson M, Klerman GL. Trends in the prescription of antidepressants by office-based psychiatrists. Am J Psychiatry 1993;150:571-7.
- Thase ME, Kupfer DJ. Recent developments in the pharmacotherapy of mood disorders. J Consult Clin Psychol 1996;64:646-59.
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979.
- American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder (revision). Am J Psychiatry 2000;157(4 Suppl):S1-45.
- Rush AJ, Beck AT, Kovacs M, Hollon S. Comparative efficacy of cognitive therapy and pharmacotherapy in the treatment of depressed patients. Cognit Ther Res 1977;1:17-37.
- Murphy GE, Simons AD, Wetzel RD, Lustman PJ. Cognitive therapy and pharmacotherapy. Singly and together in the treatment of depression. Arch Gen Psychiatry 1984;41:33-41.
- Dobson KS. A meta-analysis of the efficacy of cognitive therapy for depression. J Consult Clin Psychol 1989;57:414-9.
- Antonuccio D. Psychotherapy for depression: no stronger medicine. Am Psychol 1995;50:450-2.
- Elkin I, Shea MT, Watkins JT, Imber SD, Sotsky SM, Collins JF, et al. National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments. Arch Gen Psychiatry 1989;46:971-82.
- Klein DF. Preventing hung juries about therapy studies. J Consult Clin Psychol 1996;64:81-7.
- Jacobson NS, Hollon SD. Cognitive-behavior therapy versus pharmacotherapy: now that the jury’s returned its verdict, it’s time to present the rest of the evidence. J Consult Clin Psychol 1996;64:74-80.
- Jacobson NS, Hollon SD. Prospects for future comparisons between drugs and psychotherapy: lessons from the CBT-versus- pharmacotherapy exchange. J Consult Clin Psychol 1996;64:104-8.
- Elkin I, Gibbons RD, Shea MT, Shaw BF. Science is not a trial (but it can sometimes be a tribulation). J Consult Clin Psychol 1996;64:92- 103.
- Hollon SD, DeRubeis RJ, Evans MD. Wiemer MJ, Garvey MJ, Grove WM, et al. Cognitive therapy and pharmacotherapy for depression. Singly and in combination. Arch Gen Psychiatry 1992;49:774-81.
- Elkin I, Gibbons RD, Shea MT, Sotsky SM, Watkins JT, Pilkonis PA, et al. Initial severity and differential treatment outcome in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol 1995;63:841-7.
- Diagnostic and statistical manual of mental disorders, 4th edition: DSM-IV. Washington D.C.: Am Psychiatric Association; 1994.
- First MB, Spitzer RL, Gibbon M, et al. Structured clinical interview for Axis-I DSM-IV disorders: patient edition (SCID-II, version 2.0). New York: New York State Psychiatric Institute Biometrics Research Department; 1994.
- Beck AT, Steer RA: Manual for the revised Beck Depression Inventory. San Antonio, Tex, Psychological Corp.; 1987.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988.
- Rosnow RL, Rosenthal R. Computing contrasts, effect sizes, and counternulls on other people’s published data: general procedures for research consumers. Psychological Methods 1996;1:331-40.
- Fawcett J, Epstein P, Fiester SJ, Elkin I, Autry JH. Clinical management—imipramine / placebo administration manual. NIMH Treatment of Depression Collaborative Research Program. Psychopharmacol Bull 1987;23:309-24.
- Friedman RA, Markowitz JC, Parides M, Kocsis JH. Acute response of social functioning in dysthymic patients with desipramine. J Affect Disord 1995;34:85-8.
- Kocsis JH, Zisook S, Davidson J, Shelton R, Yonkers K, Hellerstein DJ, et al. Double-blind comparison of sertraline, imipramine, and placebo in the treatment of dysthymia: psychosocial outcomes. Am J Psychiatry 1997;154:390-5.
- Marin DB, Kocsis JH, Frances AJ, Parides M. Desipramine for the treatment of “pure” dysthymia versus “double” depression. Am J Psychiatry 1994;151:1079-80.
- Stewart JW, McGrath PJ, Quitkin FM, Rabkin JG, Harrison W, Wager S, et al. Chronic depression: response to placebo, imipramine, and phenelzine. J Clin Psychopharmacol 1993;13:391-6.
- Versiani M, Nardi AE, Figueira IL, Stabl M. Tolerability of moclobemide, a new reversible inhibitor of monoamine oxidase-A, compared with other antidepressants and placebo. Acta Psychiatr Scand Suppl 1990;360:24-8.
- Pétursson H. Studies of reversible and selective inhibitors of monoamine oxidase A in dysthymia. Acta Psychiatr Scand Suppl 1995;386:36-9.
- Vallejo J, Gasto C, Catalan R, Salamero M. Double-blind study of imipramine versus phenelzine in Melancholias and Dysthymic Disorders. Br J Psychiatry 1987;151:639-42.
- Hellerstein DJ, Samstag LW, Cantillon M, Maurer M, Rosenthal J, Yanowitch P, et al. Follow-up assessment of medication-treated dysthymia. Prog Neuropsychopharmacol Biol Psychiatry 1996;20:427- 42.
- Ravindran AV, Bialik RJ, Lapierre YD. Primary early onset dysthymia, biochemical correlates of the therapeutic response to fluoxetine: I. Platelet monoamine oxidase and the dexamethasone suppression test. J Affect Disord 1994;31:111-7.
- Ravindran AV, Griffiths J, Waddell C, Anisman H. Stressful life events and coping styles in relation to dysthymia and major depressive disorder: variations associated with alleviation of symptoms following pharmacotherapy. Prog Neuropsychopharmacol Biol Psychiatry 1995;19:637-53.
- Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Eng J Med 2000;342:1462- 70.
- Blackburn IM, Bishop S, Glen AI, Whalley LJ, Christie JE. The efficacy of cognitive therapy in depression: a treatment trial using cognitive therapy and pharmacotherapy, each alone and in combination. Br J Psychiatry 1981;139:181-9.
- de Jonghe F, Hendricksen M, van Aalst G, Kool S, Peen V, Van R, et al. Psychotherapy alone and combined with pharmacotherapy in the treatment of depression. Br J Psychiatry 2004;185:37-45.
- Rush AJ, Beck AT, Kovacs M, Weissenburger J, Hollon SD. Comparison of the effects of cognitive therapy and pharmacotherapy on hopelessness and self-concept. Am J Psychiatry 1982;139:862-6.
- Karasu TB. Psychotherapy and pharmacotherapy: toward an integrative model. Am J Psychiatry 1982;139:1102-13.