Hong Kong J Psychiatry 2008;18:136-43
ORIGINAL ARTICLE
兒童事件影響量表(修訂版)在量度道路交通事故兒童生還者 之心理測量學特性及結構驗證性分析
胡潔瑩、陳潔冰、洪凱揚、曹韻芝
Dr Kitty K Wu, PhD, Department of Clinical Psychology, Caritas Medical Centre, Hospital Authority, Hong Kong, China.
Ms Sumee K Chan, MSocSc (Clin Psy), Department of Paediatrics and Adolescent Medicine, Princess Margaret Hospital, Hospital Authority, Hong Kong, China. Mr Ocean H Hung, MSocSc (Clin Psy), Hong Kong Red Cross, Hong Kong, China.
Ms Valda W Cho, MSocSc (Clin Psy), Department of Clinical Psychology, Caritas Medical Centre, Hospital Authority, Hong Kong, China.
Address for correspondence: Dr Kitty K Wu, Department of Clinical
Psychology, Caritas Medical Centre, Hospital Authority, Hong Kong, China. Tel: (852) 3408 7975; Fax: (852) 2307 5894;
E-mail: wukyk@ha.org.hk
Submitted: 14 March 2008; Accepted: 5 May 2008
Abstract
Objective: This study examined the psychometric properties of the Children’s Impact of Event Scale– Revised.
Participants and Methods: Sixty one children (aged 8 to 17 years) who attended the hospital accident and emergency service after road traffic accidents participated in the study. The Children’s Impact of Event Scale–Revised, Children’s Depression Inventory, and Revised Children’s Manifest Anxiety Scale completed by the children 1 month after the road traffic accidents were studied.
Results: A 3-factor structure accounting for 72% of the variance was identified for the 11-item Children’s Impact of Event Scale–Revised. The test-retest reliability was satisfactory; the moderate correlations between the Children’s Impact of Event Scale–Revised scores (i.e. intrusion, avoidance, and hyperarousal), Children’s Depression Inventory, and Revised Children’s Manifest Anxiety Scale supported the validity of the Children’s Impact of Event Scale–Revised as a measure of post-traumatic stress in children. Results of the confirmatory factor analysis support generalisation of the post-traumatic stress disorder framework for the present sample of Chinese children.
Conclusions: The 11-item Children’s Impact of Event Scale–Revised has satisfactory psychometric properties as a screening instrument for stress responses after traumatic incidents.
Key words: Accidents, traffic; Anxiety; Depression; Stress disorders, post-traumatic; Wounds and injuries
摘要
目的:探討兒童事件影響量表(修訂版)的心理測量學特性。
參與者與方法:共有61名介乎8至17歲,因道路交通事故而到急症室求診之兒童參予是項研究。研究探討了這組參與者在意外後一個月填寫的心理量表之結果,這些量表包括兒童事件影響量表(修訂版)、兒童抑鬱量表以及兒童顯性焦慮量表(修訂版)。
結果:在是項研究中,從包含11個項目的兒童事件影響量表(修訂版)中提取了三個公因子,它們的總解釋變異量為72%。其重測信度令人滿意;兒童事件影響量表(修訂版)各分數(即侵入感、迴避及過度反應)、兒童抑鬱量表及兒童顯性焦慮量表(修訂版)之間的相關性是中度,這表示兒童事件影響量表(修訂版)作為量度創傷後壓力反應有一定的效度。同時,結構驗證性因素分析的結果亦支持將創傷後壓力症候群之架構應用在這組華裔兒童上。
結論:包含11個項目的兒童事件影響量表(修訂版)有滿意的心理測量學特性,以支持其作為量度創傷事件後壓力反應之篩查工具。
關鍵詞:交通事故、焦慮、抑鬱、創傷後壓力症候群、傷口及受傷
Introduction
The Impact of Event Scale (IES) developed by Horowitz and colleagues1 has been widely adopted for research studying the psychological impact of trauma in both adults2 and children.3 For child survivors, the impact of traumatic events documented include that of a cruise ship sinking,3 sexual abuse,4,5 and surviving war.6,7 Some studies have addressed the cross-cultural validity of assessing post- traumatic stress disorder (PTSD) in children by examining the factor structure of the IES for children in different cultures. A 3-factor solution (intrusion, avoidance, and emotional numbing) has been found among Cambodian youth8 and for British child survivors of a shipping disaster.9 In contrast, a 2-factor solution (intrusion and avoidance) was identified in a Croatian study6 and a study of children from Bosnia.10
Some recent developments of the IES may affect utilisation of the IES in children. Weiss and Marmar2 revised the IES by including items tracking the response in the domain of hyperarousal symptoms. The psychometric properties of the Impact of Event Scale–Revised (IES-R) for adults in different languages have been demonstrated in previous studies.2,11 Some studies have reported that a number of items in the original IES are misinterpreted by children.3,6 As a result, 8 items that best reflect the underlying factor structure identified in these studies have been selected for a shortened version, namely, the Children’s Impact of Events Scale.12 In a more recent study, 5 items used for tapping the hyperarousal symptoms related to PTSD in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) were included. A 3-factor solution (intrusion, hyperarousal, and avoidance) was identified when a 3-factor model was specified in the principal component analysis.10 However, the empirical evidence for cross-cultural application of this 3-factor PTSD framework to children who have experienced civilian trauma is scarce.
The present study aimed to develop the Children’s Impact of Event Scale–Revised (CHIES-R) and examine its psychometric properties in Chinese children in Hong Kong. Aims include: (a) gathering data for the CHIES-R from a group of children and adolescents 1 month after they experienced a road traffic accident (RTA) that required them to attend hospital accident and emergency (A&E) services; (b) examining the psychometric properties of the CHIES-R; (c) examining the validity of the CHIES-R by investigating its relationship with other self-reported measures of psychological distress; (d) examining the cross-cultural application of the PTSD framework by investigating the underlying factor structure of CHIES-R in children who have survived a RTA in Hong Kong.
Methods
Measures
The measures used were standardised self-reporting questionnaires. Though parents may need to explain the aims of the study to younger children, parental participation was not required for completing the different measures. The measures used include the following.
Children’s Impact of Event Scale–Revised
The development of the CHIES-R was based on the Children’s IES12 which originated from the IES,13 and the Chinese version of the IES-R which has good psychometric properties for the adult population.11,14 The Chinese IES-R was used as a reference in this study because the 22 items of the Chinese IES-R include all the items in the original IES and the Children’s IES. The comparability of the CHIES- R and these referenced scales have been validated using stringent back-translation procedures.
The 8 items for intrusion and avoidance features used in both the Children’s IES and the Chinese IES-R were included in the Chinese CHIES-R. An additional intrusion item “I had dreams about it” used in the IES-R was also included for its clinical relevance to the child population. Four hyperarousal items from the IES-R were included; 2 items were excluded because they were likely to be misunderstood by children.10 A pilot study involving 118 boys and 266 girls, aged 8 to 17 years (mean, 12.80; standard deviation [SD], 2.26 years) from 2 primary and 2 secondary normal schools, who had not been screened for traumatic event experiences in Hong Kong, was conducted. Based on previous studies,2,11,14 children were asked to report the degree of distress caused by each psychological symptom related to final examinations. A simple Likert method (0 to 4) was used for scoring. The subscale score was equal to the mean of the non-missing items. It takes approximately 5 minutes to complete the CHIES-R. The pilot study results confirmed that the administration of the test and the items presented in the Chinese language was appropriate and comprehensible for children and adolescents in Hong Kong. Since the incident used in the pilot study, ‘final examination’, was not a traumatic event, our study further examined the clinical relevance of the scale by applying it to child survivors of RTA.
Children’s Depression Inventory
The Children’s Depression Inventory (CDI)15 is a 27-item self-rating, symptom-oriented scale designed for children. The instrument quantifies a range of depressive symptoms including disturbed mood, hedonic capacity, vegetative functions, self-evaluation, and interpersonal behaviours. The psychometric properties of the CDI have been studied in many research studies since 1992.15 The CDI has been translated into Chinese and a normative study is currently being conducted by the Division of Clinical Psychology, Hong Kong Psychological Society (KK Wu and SK Chan, personal communication, 15 December 2007). It takes approximately 5 minutes to complete the CDI.
Revised Children’s Manifest Anxiety Scale
The Revised Children’s Manifest Anxiety Scale (RCMAS)16 is a 37-item self-administered inventory designed for children aged from 6 to 19 years. The anxiety measured is categorised into 3 domains including physiological anxiety, worry / oversensitivity, and social concern / concentration. It also includes a Lie subscale. The instrument has continued to be used in research as a tool for studying anxiety manifested by children and adolescents in different contexts,17,18 including children who have had traumatic experiences.19-21 The scale has been translated into Chinese and a normative study has been conducted locally (KK Wu and SK Chan, personal communication, 15 December 2007). It takes approximately 5 minutes to complete the RCMAS.
Participants
The study was conducted with the approval of the hospital’s Ethics Committee for Research. Children (aged 8 to 17 years) who attended the Caritas Medical Centre (a general ospital) A&E service during the period November 2003 to July 2006, after surviving a RTA, were invited to participate in the study. Children unable to fill in self-reporting questionnaires due to impediments such as intellectual disabilities or severe head injuries were excluded from the study. Participants were required to complete the CHIES-R, CDI and RCMAS 1 month after the RTA. Thirty six boys and 25 girls, aged 8 to 17 years (mean, 12.53; SD, 2.59 years), participated with written consent from their parents. Accident and emergency physicians rated the severity of the children’s physical symptoms. Fifty (82%) of the children had physical injuries rated as “Mild: operation or plaster of Paris (POP) not required; Glasgow Coma Score (GCS) of 15”, and 11 (18%) were rated as “Severe: hospital admission required; GCS of 14 or 15”. No child was rated as “Moderate: operation or POP required; GCS of 15” or “Life Threatening: hospital admission required; GCS of 13 or below”.Results
Principal Component Analysis
Previous studies on use of the IES-R in adults revealed a single-factor structure indicating that the 3 symptom- clusters of PTSD were highly related when hyperarousal items were added to the IES-R.2,11 In order to include more specific items for each symptom cluster, a Principal Component Analysis (PCA) was first carried out on the 9 intrusion and avoidance items as seen in a recent study for developing the IES scale with additional hyperarousal items for children.10 The initial varimax-rotated solution gave 2 factors corresponding to intrusion and avoidance items with an Eigenvalue greater than 1, accounting for 69.3% of variance. The factor loadings were comparable with those found in previous studies using the 8-item IES for children10,12 except for 1 intrusion item (“other things kept making me think about it”) which loaded onto the Avoidance factor, and one avoidance item (“I tried not to think about it”) which loaded onto the Intrusion factor. Based on results from our study, these 2 items were excluded from the full version of the CHIES-R (Table 1).
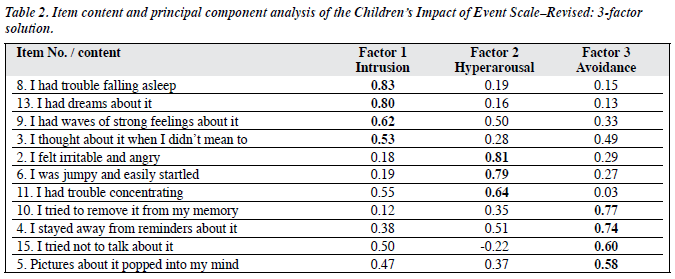
A PCA was carried out on the full 11-item CHIES-R. The initial varimax-rotated solution gave 2 factors that split the scale into Avoidance and Intrusion with Hyperarousal items spreading into both factors. The two factors accounted for 63.4% of the variance. After an examination of the scree plots, factor loadings were re-examined when the third factor, with an Eigenvalue of 0.94, and accounting for 8.6% variance was included. After varimax rotation, 3 factors corresponding to intrusion, hyperarousal, and avoidance items accounting for 72.0% of variance were found. Our findings were comparable to those of Smith et al.10 They found a 3-factor solution accounting for 49.3% of variance when a third factor with an Eigenvalue of 0.93 and a 3- factor solution was forced. As presented in Table 2, the component loadings of most of the 11 items were higher for the component made up by the items assigned for the same subscale than with other components made up by items assigned for other subscales. There was one arousal item (“I had trouble falling asleep”) that loaded onto the Intrusion factor. This suggested that in children, sleeping difficulties were more closely related to intrusion features than other hyperarousal symptoms. There was also an intrusion item (“pictures about it popped into my mind”) that loaded more on the Avoidance (0.58) than the Intrusion factors (0.47). This indicated that this particular item might not be specific for differentiation between intrusion and avoidance symptoms in children.
The correlation coefficients between the 3 subscales also indicated that they were moderately interdependent. The coefficients were as follows: Intrusion with Avoidance (r = 0.64), Intrusion with Hyperarousal (r = 0.72), and Avoidance with Hyperarousal (r = 0.59). The close relationship between the Intrusion and Hyperarousal features was consistent with a previous study using IES with 5 hyperarousal items added to the scale.10
The results of the PCA and subscale correlation were consistent, suggesting that the 3 subscales of the CHIES- R were related but possibly independent of one another, each of them representing a different type of reaction when faced with stressful events. An alternative explanation for the interdependence between the 3 PTSD symptom clusters was due to the fact that the sample in this study was not a clinical sample seeking treatment for diagnosed PTSD. Most of the children rated themselves as not affected or only slightly affected by the CHIES-R items. Thus, this sample of children who experienced a relatively mild form of civilian trauma might have blurred the boundary between the 3 subscales.
As argued by Zilberg et al,22 subscale independence might be more easily demonstrated with the PTSD patient sample at the pre-therapy evaluation point. These researchers argued that the pre-therapy evaluation point was a time when the subject as a group would present a well- defined syndrome. If this interpretation is valid, the non- clinical sample in our study is not the most suitable sample for examining the independence of the subscales of CHIES- R. Nevertheless, the data collected from a non-clinical sample have their value as a basis of comparison for future investigations. On the other hand, even with the present non-clinical sample, the validity of most items assigned to specific subscales and the subscale independence was preliminarily supported.
Confirmatory Factor Analysis
A confirmatory factor analysis (CFA) was conducted to evaluate the cross-cultural validity of the PTSD framework in this sample. This was done with the Structural Equation Modeling, using EQS for Windows Version 6.123 in which the maximum likelihood method was used to investigate the overall fit of the models to the correspondent observed variance and covariance matrices. This technique provides a number of measures of the fit of the hypothetical PTSD model to the observed data. Model fit was assessed in several ways. The goodness-of-fit indices, the Comparative Fit Index (CFI), the Root Mean Square Error of Approximation (RMSEA) and Non-normed fit index (NNFI), were examined. The CFI has a range between 0 and 1, with values greater than 0.90 indicating a good fit.24 The RMSEA is a measure of the discrepancy between the model and the data per degree of freedom. Values of RMSEA which are below 0.08 indicate a satisfactory fit.25 The NNFI measures the relative improvement in fit by comparing a target model with a baseline model with respect to the degree of freedom. It ranges from 0 to 1, with values greater than 0.90 implying a good fit.26
Using the PTSD symptom clusters listed in the DSM- IV, a 3-factor structure for the CHIES-R was examined. If items carrying almost equal loadings for more than 1 factor were included, the fit would be poor. Thus, consistent with a previous study examining the model fit of the Post- traumatic Growth Inventory for Chinese cancer survivors,27 items included in the CFA were selected based on the criteria that their loadings on a factor exceed 0.7 and the difference between their highest loading and second highest loading on different factors was at least 0.2 in the PCA for the 11-item CHIES-R. Based on these criteria, 6 items from the 11-item CHIES-R were used in the CFA with 2 items as the observed variables for each of the 3 latent PTSD factors. The results demonstrated a good fit of the 3-factor structure in the current sample that included intrusion, hyperarousal, and avoidance (χ2 (6) = 6.465, p = 0.37; CFI = 0.996; RMSEA = 0.036; NNFI = 0.991). Our findings were consistent with the existing literature on theoretical and clinical presentations of PTSD for Western28,29 and Chinese populations,30 and previous findings in children using the IES.10 The factor loadings were significant at the p < 0.05 level and are presented in the Figure.
Reliability
The standardised coefficient alpha was used to estimate internal consistency for the Intrusion, Avoidance, Hyperarousal subscales, and the Total score of the 11-item CHIES-R. The results produced the following coefficients: Intrusion (α = 0.86), Avoidance (α = 0.71), Hyperarousal (&alpha = 0.81), and Total (α = 0.91).
All items were positively correlated with their assigned subscale with the target item removed from the assigned subscale when their correlations were examined by standard alpha coefficient analyses. The results of these corrected item-subscale correlations yielded the following coefficients: Intrusion (rs = 0.64 to 0.77), Avoidance (rs = 0.39 to 0.60), Hyperarousal (rs = 0.50 to 0.72), and Total (rs = 0.44 to 0.79). These data suggest that the internal consistency of the 3 subscales and the total score is satisfactory and each of the individual items is consistent with the other items.
Of the 61 study participants, 35 (57.3%) agreed to complete the CHIES-R again 3 months after the RTA. Their data were used to examine the test-retest reliability of the CHIES-R with a 2-month interval, yielding the following correlation coefficients: Intrusion (r = 0.56), Avoidance (r = 0.57), Hyperarousal (r = 0.66), and Total (r = 0.74). No significant difference was found between these respondents and those who did not respond 3 months after the RTA in terms of age, gender, severity of physical injury, and CHIES-R scores 1 month after the RTA.
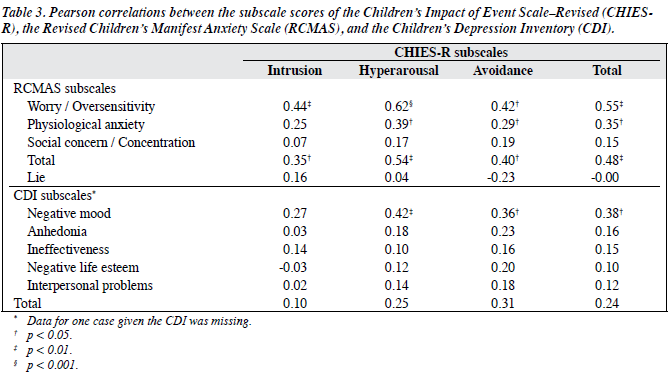
Convergent Validity
To examine the convergent validity of the CHIES-R with other measures of psychological distress in children, the relationships of the subscale and total scores from the CHIES- R and those from the CDI and RCMAS were examined. Table 3 presents the correlation coefficients from these subscale and total scores. The correlations indicated that the relationships between the subscale and total scores for the CHIES-R and those for the other 2 self-reported measures, excluding the Lie subscale of the RCMAS, were low to moderate (rs = 0.02 to 0.62). Our data demonstrated that the CHIES-R Intrusion, Avoidance and Hyperarousal subscales contributed information that was not captured by other self- reported measures of psychological distress in children. Moreover, the correlation coefficients between the scores for the CHIES-R and RCMAS were, in general, higher than those between the CHIES-R and the CDI. For the CHIES-R and the RCMAS, the mean rs = 0.35 (range, 0.07 to 0.62) with the highest correlation found between the Hyperarousal subscale of the CHIES-R and the Oversensitivity subscale of the RCMAS. For the CHIES-R and the CDI, the mean rs = 0.18 (range, 0.02 to 0.42). This is consistent with the DSM-IV31 nomenclature as PTSD is classified as an anxiety disorder, while depression is classified as a mood disorder.
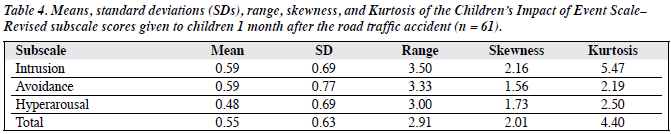
Descriptive Statistics
The means and SDs of the 11-item CHIES-R, the CDI and RCMAS are shown in Table 4. Independent sample t tests showed no significant differences between boys and girls, or between children with mild and severe physical injury in terms of the CHIES-R scores. The Pearson correlations between age and CHIES-R scores were not significant.
Discussion
This study provides preliminary data on the reliability and validity of the CHIES-R for Chinese children in Hong Kong, suggesting that it has potential application as a tool for assessing the psychological distress experienced by clinical populations and for evaluation of treatment outcomes in the child and adolescent populations. As suggested by the National Institute for Health and Clinical Excellence,32 in individuals at high risk of developing PTSD following a major disaster, consideration should be given to the routine use of a brief screening instrument for PTSD at 1 month after the disaster. Moreover, identification of post- traumatic stress in children can be improved if children are asked directly about their experiences. In this context, the CHIES-R may be considered a standardised self-reporting measure for screening children who are at risk of developing prolonged distress after experiencing traumatic events. The CHIES-R may also be utilised for examining the application of the PTSD model in Chinese children. In the present study, the results of the factor analysis and the moderate correlations between the 3 subscales suggest that intrusion, avoidance and hyperarousal are closely related but separable constructs. Results of the PCA support the validity of items assigned for specific subscale and subscale independence of the 11-item CHIES-R. The CFA results support the cross- cultural application of the 3-factor PTSD framework for children who have experienced civilian trauma. Consistent with previous findings in Bosnian children,10 our findings also indicate that the 3 factors are significantly related to each other and a number of items in the CHIES-R have similar loadings on more than 1 factor.
Our findings are not consistent with previous findings suggesting that there are different patterns of post-traumatic psychological distress manifested by subjects traumatised at different ages.33-37 The absence of the age effect on the CHIES-R scores in our sample might be due to the relatively mild traumatic stress experienced as most of the children were found to have mild physical injuries when they attended the A&E.
A number of issues needing further investigation remain, due to the limitations of this study. The power of analysis and generalisability are limited by the sample size. Although the assignment of items for subscale and subscale independence were confirmed by the PCA, many items also have significant loadings on another factor. While this indicates that symptom manifestations in children may not be easily differentiated into 3 independent clusters as in the present PTSD framework for adults, the small sample size and the relatively mild nature of the trauma experienced by our sample have probably limited the power of the study to identify a well-differentiated 3-factor PTSD model. Since the CHIES-R aims to study the psychological impact of traumatic events, it would be more appropriate to examine the psychometric properties of the CHIES-R with a sample of subjects who have experienced life-threatening critical incidents or who have been diagnosed with PTSD. In addition, a split sample or an independent sample approach for exploratory and confirmatory analysis would be more appropriate if a larger sample size is available.
Instead of just including the results of a single PCA on the full 11-item scale, the report of results from 2 PCA on different test items was provided in order to review results that replicate previous findings10 and strategies for the selection of specific items for the final version. Otherwise, the use of the PCA on the full 11-item scale would be sufficient.
This study is limited by the use of self-reported screening instruments, the CDI and the RCMAS, for an examination of the convergent validity of the CHIES- R. Further investigations of the relationship between the CHIES-R and other clinical measurements of PTSD for children, such as clinical interviews, are needed to examine the specificity of the CHIES-R for screening of PTSD in children. For future studies, a number of other issues could be considered including the utilisation of the CHIES-R for the evaluation of treatment outcomes; examining the test-retest reliability over different time intervals because symptoms are not expected to persist in children with a mild level of distress; utilising stratified sampling for a wide age range for development of normative data.
Acknowledgements
This study was supported by the Clinical Psychology Department and the A&E Department of the Caritas Medical Centre. We would like to thank Dr Yiu-wah Fung, Mr Wai- ming Tsang, Ms Mabel Tse, and Ms Catherina Ng for their contributions to the study. We also thank Mr YY Ip, Sr Cynthia Tang and Sr Virginia Wong for arranging participants for the pilot study. We also thank Prof Daniel Weiss for his input into the translation procedure for the IES-R. We also thank the children who participated in the study. The source of the CHIES-R is available from the first author.
References
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979;41:209-18.
- Weiss DS, Marmar CR. The Impact of Event Scale-Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997:399-411.
- Yule W, Udwin O. Screening child survivors for post-traumatic stress disorders: experiences from the ‘Jupiter’ sinking. Br J Clin Psychol 1991;30:131-8.
- Alexander P. The differential effects of abuse characteristics and attachment in the prediction of long-term effects of sexual abuse. J Interpers Violence 1993;8:346-62.
- Murphy SM, Kilpatrick DG, Amick-Mcmullan A, Veronen LJ. Current psychological functioning of child sexual assault survivors: a community study. J Interpers Violence 1988;3:55-79.
- Dyregrov A, Kuterovac G, Barath A. Factor analysis of the impact of event scale with children in war. Scand J Psychol 1996;37:339-50.
- Thabet AA, Vostanis P. Post-traumatic stress reactions in children of war. J Child Psychol Psychiatry 1999;40:385-91.
- Sack WH, Seeley JR, Clarke GN. Psychometric properties of the Impact of Events Scale in traumatised Cambodian refugee youth. Pers Individ Dif 1998;25:57-67.
- Yule W, ten Bruggencate S, Joseph S. Principal components analysis of the Impact of Event Scale in adolescents who survived a shipping disaster. Pers Individ Dif 1994;16:685-91.
- Smith P, Perrin S, Dyregrov A, Yule W. Principal components analysis of the impact of event scale with children in war. Pers Individ Dif 2003;34:315-22.
- Wu KK, Chan KS. The development of the Chinese version of Impact of Event Scale – Revised (CIES-R). Soc Psychiatry Psychiatr Epidemiol 2003;38:94-8.
- Sclare I. The child psychology portfolio. U.K.: Nfer-Nelson; 1997.
- Horowitz MJ. Stress response syndromes. New York: Jason Aronson; 1976.
- Wu KK, Chan KS. Psychometric properties of the Chinese version of Impact of Event Scale – Revised (IES-R). Hong Kong J Psychiatry 2004;14:2-8.
- Kovacs M. Children’s Depression Inventory. New York: Multi-Health Systems, Inc; 1992.
- Reynolds CL, Richmond BO. Revised Children’s Manifest Anxiety Scale. California: Western Psychological Services; 1978.
- Bouldin P, Pratt C. A systematic assessment of the specific fears anxiety level and temperament of children with imaginary companions. Aust J Psychol 2002;54:79-85.
- DeMaso DR, Spratt EG, Vaughan BL, D’Angelo EJ, Van der Feen JR, Walsh E. Psychological functioning in children and adolescents undergoing radiofrequency catheter ablation. Psychosomatics 2000;41:134-9.
- Chemtob CM, Nakashima J, Carlson JG. Brief treatment for elementary school children with disaster-related posttraumatic stress disorder: a field study. J Clin Psychol 2002;58:99-112.
- Dalgleish T, Moradi A, Taghavi R, Neshat-Doost H, Yule W, Canterbury R. Judgements about emotional events in children and adolescents with post-traumatic stress disorder and controls. J Child Psychol Psychiatry 2000;41:981-8.
- Udwin O, Boyle S, Yule W, Bolton D, O’Ryan D. Risk factors for long- term psychological effects of a disaster experienced in adolescence: predictors of post traumatic stress disorder. J Child Psychol Psychiatry 2000;41:969-79.
- Zilberg NJ, Weiss DS, Horowitz MJ. Impact of Event Scale: a cross- validation study and some empirical evidence supporting a conceptual model of stress response syndromes. J Consult Clin Psychol 1982;50:407-14.
- EQS for Windows (Version 6.1) [Computer software] [program]. Encino, CA: Multivariate Software; 2003.
- Byrne BM. Structural equation modeling with EQS and EQS Windows: basic concepts, applications, and programming. Thousand Oaks, CA: Sage Publications; 1994.
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993: 136-62.
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull 1980;88:588-606.
- Ho SM, Chan CL, Ho RT. Posttraumatic growth in Chinese cancer survivors. Psychooncology 2004;13:377-89.
- Asmundson GJ, Frombach I, McQuaid J, Pedrelli P, Lenox R, Stein MB. Dimensionality of posttraumatic stress symptoms: a confirmatory factor analysis of DSM-IV symptom clusters and other symptom models. Behav Res Ther 2000;38:203-14.
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychol Assess 1998;10:90-6.
- Wu KK, Chan SK, Yiu VF. Psychometric properties and confirmatory factor analysis of the Posttraumatic Stress Disorder Checklist for Chinese survivors of road traffic accidents. Hong Kong J Psychiatry 2008;18:144-51.
- Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
- National Institute for Health and Clinical Excellence. PTSD Guideline from National Institute for Health and Clinical Excellence; 2005.
- Norris FH, Murell SA. Prior experience as a moderator of disaster impact on anxiety symptoms in older adults. Am J Community Psychol 1988;16:665-83.
- Solomon Z. Holocaust survivors in the Gulf War. In: Solomon Z, editor. Coping with war-induced stress. New York: Plenum Press; 1995:133- 54.
- Maercker A, Schützwohl M. Long-term effects of political imprisonment: a group comparison study. Soc Psychiatry Psychiatr Epidemiol 1997;32:435-42.
- Maercker A. Lifespan psychological aspects of trauma and PTSD: symptoms and psychosocial impairments. In: Maercker A, Schutzwohl M, Solomon Z, editors. Posttraumatic stress disorder: a lifespan developmental perspective. Toronto: Hogrefe & Huber; 1999:7-41.
- Schützwohl M, Maercker A. Posttraumatische Belastungsreaktionen nach kriminellen Gewaltdelikten [Posttraumatic stress reactions following criminal victimization]. Zeitschrift fr Klinische Psychologie 1997;26:258-268.