Hong Kong J Psychiatry 2005;15(3):71-76
ORIGINAL ARTICLE
GLK Hsu, YM Wan, D Adler, W Rand, E Choi, BYP Tsang
First presented at the 2001 American Psychiatric Association Annual Meeting, New Orleans, USA.
Dr George LK Hsu, MD, FRCPsych, Tufts-New England Medical Center, Boston, Massachusetts, USA.
Dr Yu Mui Wan, EdD, Boston University Center for Psychiatric Rehabilitation, Boston, Massachusetts, USA.
Dr David Adler, MD, Tufts-New England Medical Center, Boston, Massachusetts, USA.
Dr William Rand, PhD, Tufts-New England Medical Center, Boston, Massachusetts, USA.
Dr Elaine Choi, MD, Tufts-New England Medical Center, Boston, Massachusetts, USA.
Dr Bill YP Tsang, EdD, Research Associate, Hong Kong Chinese University Department of Social Work, Hong Kong, China.
Address for correspondence: Dr George LK Hsu, Professor of Psychiatry,
Tufts-New England Medical Center, Tufts University School of Medicine, Tufts-NEMC, 750 Washington Street, Box, #1007, Boston, MA 02111, USA.
Tel: 617 636 7584; Fax: 617 636 4852;
E-mail: ghsu@tufts-nemc.org
Submitted: 11 April 2005; Accepted: 29 December 2005
Abstract
Objective: To assess the prevalence of major depressive disorder in Chinese Americans in the greater Boston area.
Patients and Methods: Chinese American participants were recruited through 10 primary care clinics in greater Boston. Depression was determined by assessment on 2 screening instruments, the Mental Health Index-5 and Primary Care Screener for Affective Disorders for the first-stage survey and by Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, 4th edition for the second-stage interview.
Results: The prevalence of major depressive disorder among Chinese Americans attending primary care clinics (one-year prevalence of about 10%) appeared similar to the prevalence reported in other ethnic groups. The brief survey (Mental Health Index-5) performed as well as the lengthier one (Primary Care Screener for Affective Disorders). Few Chinese Americans with identified major depressive disorder had received antidepressant treatment from their primary care physician.
Conclusion: Cultural beliefs about mental health appeared as barriers to both detection and treatment in this study.
Key words: Chinese Americans, Major depressive disorder, Prevalence, Primary health care, Questionnaires
Introduction
Depression is a common disorder in the USA. Between 5% to 12% of men and 10% to 25% of women have an episode of major depressive disorder (MDD) during their lifetime.1 Depression is also a serious illness, leading to functional impairment, poor quality of life, loss of economic produc- tivity, greater health care utilisation, and an increased risk for suicide and increased mortality.2-9 It has been estimated that MDD is associated with 20,000 suicides and $44 billion in health care costs in the USA annually.10,11 However, little is known about the prevalence of MDD among Asian Americans in the USA, despite the fact that they constitute one of the fastest growing sectors of the population over the last 30 years.12
It is widely acknowledged that Asian Americans shun mental health services,13 as most ethnic minorities do.14 There is evidence to indicate that Asian Americans under- utilise outpatient,15 inpatient16 and emergency17 psychiatric services. Reasons for this may be complex but the stigma of mental illness is thought to be a major factor.18-21 It is possible that the use of alternative methods of treatment (such as acupuncture) along with barriers to care (such as language and cost issues) may also have reduced the use of mainstream psychiatric services by Asian Americans.
Given the antipathy that Asian Americans appear to hold for mental health services, it seemed reasonable to specu- late that Asians who are depressed may be more likely to seek treatment from primary care physicians (PCPs) than from psychiatrists. This may be particularly the case for in- dividuals who experience and present with somatoform symptoms of MDD.22-24 Research in this area is lacking, however. Despite the recent increase in research on MDD in primary care,25-28 only one published study29 was identi- fied that focused specifically on the issue of MDD among Chinese Americans in primary care. A further study by Yeung and colleagues noted that consulting a PCP for symptoms related to MDD was considered more acceptable to Chinese Americans than consulting a psychiatrist.30
In a 14-nation survey conducted by the World Health Organization, rates of depression reported were the lowest in two Asian countries, China and Japan.31 This finding is difficult to explain since China and Japan have suicide rates that are among the highest in the world.32 It is possible that there is under-reporting of depression in such surveys because of the stigma attached.
This paper reports a two-stage survey to determine the prevalence of MDD in Chinese Americans in primary care conducted in metropolitan Boston. Chinese Americans were the focus of the survey because they constitute the largest group among Asians in Massachusetts.12 The study was ap- proved by the Human Institutional Review Committee of Tufts-New England Medical Center, and was designed to answer the following questions:
- Is a simple screening instrument, the Mental Health Index-5 (MHI-5),33 better or worse at detecting depres- sion in primary care in Chinese Americans than the Primary Care Screener for Affective Disorders (PC-SAD),34 a detailed screening instrument?
- What is the estimated prevalence of depression in this population?
- Do Chinese Americans diagnosed with MDD under- utilise mental health services? If so which of the 3 factors that Rogler and colleagues14 identified as rea- sons for mental health service underutilisation (cultural beliefs that impede use of services, use of alternative pathways of care, and actual barriers to care) are responsible for underutilisation in Chinese Americans?
- What is the influence of the level of acculturation on the performance of the screening instruments, the prevalence of depression, and the pattern of service utilisation?
Patients and Methods
Participants and Procedure
The study was conducted at ten PCP offices in the metro- politan Boston area. Five of the PCPs belonged to the Gen- eral Medical Associates of Tufts-New England Medical Center. The other 5 were private practitioners, 3 with of- fices in the Chinatown area, and 2 with offices in nearby towns (Quincy and Malden) with large Chinese immigrant populations. The questionnaire phase of the study was con- ducted between November 1999 and March 2000 and the interview phase from February 2000 to July 2000.
Chinese patients attending one of the 10 above-mentioned PCP clinics were approached for recruitment to the study. During the first 4 weeks of the recruitment phase, a study packet containing a one-page flyer describing the study, a copy of the consent form, the MHI-5 and PC-SAD were placed at the receptionist's counter at each clinic. All Chi- nese patients who came to register at the receptionist's counter were given the study packet by the receptionist. Those who expressed an interest in participating in the study were encouraged to call the research assistant (RA) at Dr Hsu's office regarding study participation. The initial response was very poor and after 4 weeks, RAs trained by one of the authors on how to approach a patient for a research study, were stationed at each PCP clinic for 4 to 12 hours each week. The RA would approach each Chinese patient at the clinic and describe the study. The patient would complete the MHI-5 and PC-SAD after they had signed the consent form. The RA was present to answer any questions that the patient had regarding the questionnaires, but the questionnaires were not administered orally by the RA. Subjects were reimbursed $5 for comple- tion of the questionnaires.
Instruments
The two questionnaires were: (1) MHI-5,33 a subscale of the SF-36,35 a 5-item general mental health screening instrument for psychiatric symptoms that have occurred in the past 4 weeks. The MHI-5 took 2 to 3 minutes to complete; and (2) PC-SAD, a 37-item self-administered questionnaire consisting of a 3-item pre-screener, a 26-item MDD section, and an 8-item dysthymia section. The pre-screener, designed to reduce respondent burden by terminating the question- naire when all responses to the 3 items are negative, con- sists of 2 depression questions closely related to the World Health Organization depression screening tool36 and one dysthymia question. The PC-SAD provides a breakdown of each of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) MDD/dysthymia symp- toms for the diagnosis of current MDD (sensitivity 87.2%, specificity 95%) and dysthymia according to DSM-IV criteria.34 It takes 1 to 2 minutes to complete the PC-SAD pre- screener, but about 30 minutes for the full questionnaire if the individual answers "yes" to any of the pre-screening questions. To obtain a valid Chinese version of both questionnaires, the authors followed the guidelines for the cross-cultural adaptation of health measures.37 The 2 questionnaires were translated into Chinese and then translated back into English. Equivalence in conceptual content for the Chinese and English versions of the two questionnaires was achieved after several revisions by discussion among the authors.
Second-stage Interview
All subjects who had a positive score on the MHI-5 or PC-
SAD were approached by telephone for an interview, as was a randomly chosen group (20%) of subjects with a negative score on both questionnaires. Every effort was made to con- duct the interview as soon as possible after the questionnaire screening. Subjects were reimbursed $50 for the interview. A trained and experienced assessor administered the Struc- tured Clinical Interview for the DSM-III-R (SCID),38 which had been translated into Chinese, and an Acculturation Questionnaire.39
Follow-up
All subjects who were diagnosed as having MDD on interview were approached by telephone at 6 months for a telephone interview by one of the authors. Questions on current mental status and service utilisation were administered over the telephone to those who consented to the telephone interview.
Results
Number of Subjects
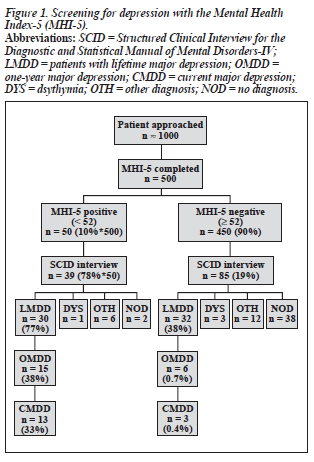
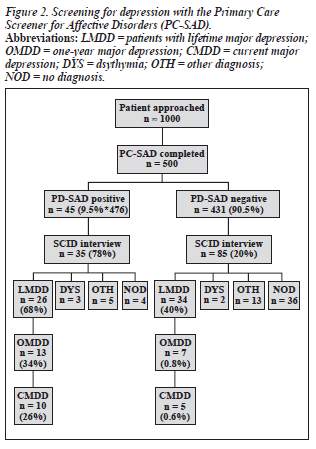
It was estimated that about 1000 patients were approached for the Phase I Study. An exact count was not possible be- cause it was unclear how many patients received the study packet during the initial 4 weeks of the study. The number of subjects who participated at each stage of the study is summarized in Figures 1 and 2.
First Phase: Screening
A total of 560 questionnaires were returned. Among the returned questionnaires, 500 MHI-5 (293 female, mean age [± SD] 44.8 ± 10.4 years; 207 male, mean age 45.9 ± 10.7 years) and 476 PC-SAD (282 female, mean age 44.9 ± 10.5 years; 194 male, mean age 46.0 ± 10.8 years) were usable. For the MHI-5, when a cut-off score of 52 was used (ie, a score of less than 52 was considered "depressed", a score of 52 or above was considered not depressed), 50 out of 500 sub- jects (10%) had a positive score. For the PC-SAD, 45 of the 476 (9.5%) had a positive score. Therefore, both question- naires identified about 10% of subjects as being depressed.
Second Phase: Interview
Interviews with the SCID were conducted in person by one of the authors. Due to the one- to five-month gap between the questionnaire survey and the interview, subjects were asked specifically for: (1) the presence of depression around the time of the questionnaire survey, defined for the purpose of this study as current depression (CMDD) and specifically about why they had visited their PCP at the time; (2) presence of depression within the past 12 months (one-year depression, OMDD); and (3) lifetime depression (LMDD).
Thirty nine of the 50 MHI positive cases and 38 of the 45 PC-SAD positive cases were interviewed. Among the MHI-5 and PC-SAD negative cases, 85 of 110 approached were interviewed. The findings are summarised in Figures 1 and 2.
Estimated Prevalence of Depression
The prevalence of current depression, as indicated by interview, was estimated as 6.5% of the 500 who provided usable MHI-5 and 7.8% of 476 usable PC-SAD results (Table 1). Since not all subjects were interviewed, these es- timates are based on projecting the depression percentages of those interviewed to the full sample. The estimated one- year rate was 10.2% according to the MHI-5, and 10.7% according to the PC-SAD. The estimated lifetime rate was about 41% for both questionnaires.
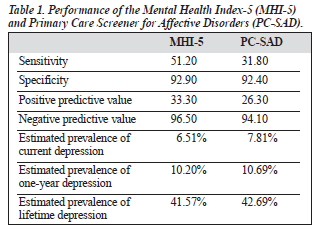
Performance of Each Questionnaire for Detecting Current Depression
The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the MHI-5 and PC- SAD are presented in Table 1, as determined by the "gold standard" of interview with the SCID.
Level of Acculturation
Of 126 subjects interviewed, 20 were at Level 1 (Very Chinese), 100 at Level 2 (Mostly Chinese), and only 4 at Level 3 (Bicultural). A further 2 subjects did not complete the acculturation scale.
Subsequent Treatment
Eleven of the 16 CMDD patients identified by MHI-5 and SCID were interviewed by telephone at 6 months. Two pa- tients returned to consult their PCP for their MDD, with neither receiving antidepressant medication. Two were treated at a mental health clinic with antidepressant medi- cation. Two sought alternative treatment (Qigong, traditional Chinese medicine). All still had some residual symptoms at follow-up. The 5 patients who declined follow-up had received no treatment from their PCP. Therefore, most pa- tients received no antidepressant treatment for their MDD.
Reasons for Mediocre Performance of Screening Questionnaires
The authors were interested in identifying why both ques- tionnaires had a relatively high false-negative rate and, par- ticularly for the PC-SAD, a relatively higher false-positive rate.
The high false-negative rate was related to 2 issues. Many subjects reported a reluctance to endorse the presence of depressive symptoms on a self-report questionnaire. They expressed a fear that if they did they might be perceived to be abnormal or mentally ill. A second reason was a different conceptualisation of depression. Many would not accept that they were "depressed" (ie, that they had a depressive or mental disorder) as they believed their symptoms were explained by their personal circumstances. Therefore, depressive symptoms occurring in the context of a stressful traumatic life event such as immigration, the cultural revolution, or unemployment, they argued, were "natural" and not abnormal ("everyone gets depressed at such times").
The high false-positive rate occurred primarily because our subjects failed to distinguish between current and past depression (ie, presence of lifetime depression but not within the past 4 weeks) on both screening questionnaires, and for the PC-SAD, to distinguish between current major depres- sion and dysthymia. It appeared that subjects either did not understand the questions that specified a time-frame (eg, "In the past 4 weeks¼"), or else did not consider the finer distinctions of symptoms occurring in different contexts to be important.
Finally, many complained predominantly of somatoform symptoms such as dizziness, palpitations, tinnitus, anorexia, insomnia and lack of strength. They believed that subjective dysphoria was a natural reaction to the somatoform symptoms ("Wouldn't you be depressed if you had these symptoms?"). This interpretation precluded them from en- dorsing the presence of depression on the questionnaire.
Discussion
This study found that the prevalence of 7% for current MDD among Chinese Americans in primary care was similar to that of other ethnic groups in a similar setting,40,41 although lower than the 14.6% reported by Yeung et al.30 About 10% of subjects had had an episode of MDD in the last 12 months, a rate that was comparable to that found in the National Comorbidity Survey,42 but about 3 times higher than the 12- month rate of the respondents in the Chinese American Psy- chiatric Epidemiology Study conducted in Los Angeles.43 Differences between samples and study methodology could have accounted for the disparate results across studies, but it seems unlikely that the prevalence of MDD among Chi- nese Americans is very different from that in the other eth- nic groups. It may also be possible that Chinese Americans are more likely to experience depression in terms of somatic or somatoform symptoms.23,44,45
There were 3 methodological limitations with this study. The first was the fact that the questionnaire survey and the SCID interview were not conducted at the same time. The SCID interview, conducted on average 3 months after the screening questionnaire survey, could have yielded biased data because of problems of recall. The second problem was the non-random selection of subjects. Many factors might have determined who in the end chose to complete and return the questionnaire, or to participate in the interview. The third problem was that our subjects were Cantonese or Mandarin speaking. Chinese subjects that did not speak either of these languages were excluded. These findings therefore may not be applicable to the overall population of Chinese Americans attending primary care.
Taking into account these limitations, the study high- lighted the difficulties encountered in the detection of depres- sion in Chinese Americans in primary care. A review by Mulrow and colleagues found that nine widely used depression screening instruments had an average sensitivity of 84% (range, 67% to 99%) and an average specificity of 72% (range, 40% to 95%).46 The sensitivity data for the 2 screen- ing questionnaires in this study were at the lower end of this range, although in terms of specificity they performed well. The mediocre performance of the questionnaires in this study seemed to be related to cultural factors: a fear of disclosure, a different conceptualisation of depression, unfamiliarity with screening instruments, and a somatoform symptom profile. Our findings therefore were in accord with those of Yeung and colleagues.30 They reported that a brief face-to- face screening conducted by an experienced researcher was likely to be more effective than a paper-and-pencil screen- ing procedure for the detection of MDD in Chinese Ameri- cans in primary care. It would be important to study the effectiveness of a two-question face-to-face case-finding interview in this population.47
That Chinese Americans would conceptualise major depression differently than current psychiatric thinking was not surprising,45 and raised ontological issues regarding the nature of MDD which are beyond the scope of this study. From a pragmatic standpoint, the conceptualisation of de- pression resulted in a passive acceptance of the symptoms that remained largely untreated during the subsequent 6 months. Untreated depression has been identified as a major burden to the individual and to society,48 leading to impaired physical, mental and social well-being, decreased productivity, and increased mortality.2-4,9,10 Our findings highlight the need for vigorous detection and treatment of MDD in Chinese Americans.
Finally, cultural beliefs about mental illness appear to be the main impediment to mental health service utilisation among the Chinese Americans in this study. There was little evidence that alternative treatments or actual barriers to care prohibit the use of mainstream mental heath services. As the majority of study subjects were traditionally Chinese in their cultural orientation, it could not be determined whether acculturation to Western beliefs about mental illness would improve the detection and treatment of MDD. This is an issue that future studies must explore. Unfortunately, many Chinese immigrants to the USA may still find the diagnosis of depression "morally unacceptable and experientially meaningless".44
Acknowledgements
This research was supported by a grant from the New England Medical Center Research Foundation and the General Clinical Research Center at Tufts-New England Medical Center under NIH grant M01 RR00054.
The authors would like to thank the following primary care physicians for their collaboration in the study and the support and assistance of their office staff: Dr Wing Ar Moy, Dr Stephen Louie, Dr Matthew Siu, Dr Lei Wang, Dr Yun Lam, Dr Robert Wu, Dr Barbara Edwards, Dr Joseph Lau, and Dr Eileen Hession.
References
- Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003;289:3095-3105.
- Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disabil- ity days, and days lost from work in a prospective epidemiologic survey. JAMA 1990;264:2524-2528.
- Covinsky KE, Fortinsky RH, Palmer RM, Kresevic DM, Landefeld CS. Relation between symptoms of depression and health status out- comes in acutely ill hospitalized older persons. Ann Intern Med 1997; 126:417-425.
- Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K. Function- ing and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry 1995;52:11-19.
- Johnson J, Weissman MM, Klerman GL. Service utilization and social morbidity associated with depressive symptoms in the community. JAMA 1992;267:1478-1483.
- Murray CJ, Lopez AD. Evidence-based health policy - lessons from the Global Burden of Disease Study. Science 1996;274:740-743.
- Ormel J, Vonkorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Com- mon mental disorders and disability across cultures. Results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA 1994;272:1741-1748.
- Simon GE, VonKorff M. Recognition, management, and outcomes of depression in primary care. Arch Fam Med 1995;4:99-105.
- Wholley MA, Browner WS. Association of depression symptom and mortality in older women. Arch Intern Med 1998;158:2129-2135.
- Hirschfeld RM, Keller MB, Panico S, et al. The National Depressive and Manic Depressive Association consensus statement on the undertreatment of depression. JAMA 1997;277:333-340.
- Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA 2003; 289:3135-3144.
- US Census 2000. United States Census Bureau, 2000. Available from: www.census.gov
- President's Commission on Mental Health. Task Force Reports: The Nature and Scope of the Problem. Vol 2. Washington DC, US Govern- ment Printing Office; 1978.
- Rogler LH, Malgady RG, Rodriguez O. Hispanics and mental health: A framework for research. Malabar, Florida. Robert E. Krieger Pub- lishing Company, 1989.
- Sue S, Fujino DC, Hu L, Takeuchi D, Zane N. Community mental health services for ethnic minority groups: a test of the cultural respon- siveness hypothesis. J Consult Clin Psychol 1991;59:533-540.
- Snowden LR, Cheung FK. Use of inpatient mental health services by members of ethnic minority groups. Am Psychol 1990;45:347-355.
- Hsu LK, Wan YM, Tsang W, Rand W, Choi E. Depression in Chinese primary care patients. Proceedings of the American Psychiat- ric Association Annual Meeting, 2001, New Orleans. Scientific and Clinical Report, Number 68.
- Bentelspacher CE, Chitran S, binte Abdul Rahman M. Coping and ad- aptation patterns among Chinese, Indian, and Malay families caring for a mentally ill relative. Families in Society 1994;75:87-294.
- Chou KL, Mak, KY. Attitudes to mental patients among Hong Kong Chinese. Int J Social Psychiatry 1998;44:215-224.
- Fan C. A comparison of attitudes towards mental illness and know- ledge of mental health services between Australian and Asian Students. Community Ment Health J 1999;35:47-57.
- Pearson V, Phillips M. Psychiatric social work and socialism: prob- lems and potential in China. Soc Work 1994;39:280-287.
- Yen S, Robins CJ, Nan L. A cross cultural comparison of depressive symptoms manifestation. J Consult Clin Psychol 2000;68:993-999.
- Hsu LK, Folstein M.F. Somatoform disorders in Caucasian and Chinese Americans. J Nerv Ment Dis 1997;185:382-387.
- Kleinman A. Neurasthenia and depression: a study of somatization and culture in China. Cult Med Psychiatry 1982;9:117-190.
- Coyne JC, Fechner-Bates S, Schwenk TL. Prevalence, nature and comorbidity of depressive disorders in primary care. Gen Hosp Psy- 37. Sartorius N, Janca A. Psychiatric assessment instruments developed chiatry 1994;16:267-276. by the World Health Organization. Soc Psychiatry Psychiatr Epidemiol
- Lin TY, Lin MC. Service delivery issues in Asian North-American communities. Am J Psychiatry 1978;135:454-456.
- Schulberg HC, Katon W, Simon GE, Rush AJ. Treating major depres- sion in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry 1998; 55:1121-1127.
- Wholley MA, Simon GE. Managing depression in medical outpatients. N Engl J Med 2000;343:1942-1950.
- Yeung A, Howarth S, Chan R, Sonawalla S, Nierenberg AA, Fava M. Use of the Chinese version of the Beck Depression Inventory for screen- ing depression in primary care. J Nerv Ment Dis 2002;190:94-99.
- Yeung A, Gresham RL, Mishonlon D, et al. Illness beliefs of depressed Chinese in primary care. Proceedings of the American Psychiatric As- sociation Annual Meeting. New Orleans: Scientific and Clinical Report, Number 69; 2001.
- WHO World Mental Health Survey Consortium. Prevalence, seve- rity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 2004;291: 2581-2590.
- Phillips MR. Suicide and attempted suicide — China, 1990-2002. Avail- able from: www.cdc.gov/mmwr/preview
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Barsky AJ, Weinstein M.C. Performance of a five-item mental health screening test. Med Care 1991;29:169-176. Available from: http://www.cdc.gov/mmwr/ preview
- Rogers WH, Wilson IR, Bungay KM, Cynn DJ, Adler DA. Assessing the performance of a new depression screener for primary care. J Clin Epidemiol 2002;55,164-175.
- Ware JE, Snow KK, Kosinski M, et al. SF-36 Health Survey: Manual and interpretation guide. Boston, Massachusetts Health Institute, New England Medical Center, 1993.
- Kessler RC, Andrews G, Mroczek D, Ustun TB, Wittchen H-U. The World Health Organization's Composite Instrument Diagnostic Inter- national Short Form (CIDI-SF). Int J Methods Psychiatr Res 1998;7: 172-188. 1996;31:55-69.
- Spitzer RL, Williams JBW, Gibbon M, First MB. Instruction manual for the Structured Clinical Interview for DSM-III-R. New York: New York State Psychiatric Institute, Biometrics Research Department; 1988. Translated by National Cheng Kung University Medical College, De- partment of Psychiatry, 1991.
- Suinn RM, Rickard-Figueroa K, Lew S, Vigil P. The Suinn-Lew Asian Self-identity Acculturation Scale: an initial report. Educ Psychol Meas 1987;47:401-407.
- Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry 1992;14:237-247.
- Zimmerman M, Farber NJ, Hartung, J, Lush DT, Kuzma MA. Screen- ing for psychiatric disorders in medical patients: a feasibility and pa- tient acceptance study. Med Care 1994;32:603-608.
- Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51:8-19.
- Takeuchi DT, Chung RC, Lin KM, et al. Lifetime and twelve-month prevalence rates of major depressive epidsodes and dysthymia among Chinese Americans in Los Angeles. Am J Psychiatry 1998;155: 1407-1414.
- Kleinman A. Culture and depression. N Engl J Med 2004;351: 951-953.
- Leff J. Psychiatry around the globe. 2nd ed. Royal College of Psychiatrists, London, 1988.
- Mulrow CD, Williams JW, Gerety MB, Ramirez O, Montiel OM, Kerber
- Case-finding instruments for depression in primary care. Ann Intern Med 1995;122:913-921.
- Wholley MA, Avins AL, Miranda L, Browner W.S. Case finding instruments for depression: 2 questions are as good as many. J Gen Intern Med 1997;12:439-445.
- World Health Organization. World Health Report 1999, World Health Organization, Geneva, Switzerland, 1999. Available from: http://www. cdc.gov/mmwr/preview