Hong Kong Journal of Psychiatry (1999) 9 (2) 6-12
REVIEW
Summary
Electroconvulsive therapy is still one of the most efficient and safe therapeutic interventions in psychiatry that is widely used all over the world. In addition to its steady popularity in clinical practice, electroconvulsive therapy has been the focus of intensive research efforts. As a consequence, electroconvulsive therapy is becoming more sophisticated and safe without loosing efficacy. One of the more innovative applications is continuation and maintenance electroconvulsive therapy, which has received increasing attention in the British and American psychiatric literature during the past decade. In this review, the current literature on continuation and maintenance electroconvulsive therapy will be summarised with special reference to the methodology, indications, standard of practice, and efficacy. This review is selective because it is based exclusively on English language papers accessed through electronic databases (MEDLINE, EMBASE, PsycINFO) and by cross-referencing publications acquired during the literature search.
Key words: Affective Disorders; Continuation and Maintenance Treatment; Electroconvulsive Therapy; Schizophrenia
INTRODUCTION
Electroconvulsive therapy (ECT) is still one of the most efficient and safe therapeutic interventions in psychiatric practice (Abrams, 1992). Since its inception more than 50 years ago, hundreds of scientifically sound studies have proven its efficacy in the treatment of several major psychiatric disorders. Despite its fearful reputation as a brutal and inhumane method, spread by its opponents who are driven by ideological and not scientific principles (Fink, 1991), ECT is widely used all over the world. In addition to its growing popularity in clinical practice, ECT has been the focus of intensive research efforts in the past two decades. As a consequence, the method for conducting ECT is becoming more sophisticated and safe without loosing its efficacy. An innovative application of ECT is continuation and maintenance ECT (ECT-C and ECT-M, respectively), which has received increasing attention in the British and American psychiatric literature during the past decade. The rationale for extending ECT is simplealthough some psychiatric conditions, particularly depression, respond well to a course of ECT, relapse may occur within months, even with prophylactic drug treatment. ECT-C or ECT-M may reduce the relapse rate in such cases.
The aim of this paper is to review the most recent literature on ECT-C and ECT-M with special reference to the methodology, indications, standard of practice, and efficacy. To the best of our knowledge, ECT-C and ECT-M are not practised in Hong Kong on a regular basis. In order to stimulate interest and possibly research in this area in Hong Kong, this review will focus on the usefulness and applicability of ECT-C and ECT-M in clinical practice.
Available electronic databases (MEDLINE, 1966-1998; EMBASE, 1989-1998; PsycINFO, 1967-1998) were screened for English language publications on ECT-C and ECT-M, supplemented by cross-referencing papers obtained during the literature search. Since there have been relatively few reports with sound methodology, textbooks, review papers, case series and single case reports have also been taken into consideration when summarising the literature.
This literature review is selective in the sense that it included only English language papers and the main focus was the practical implications of ECT-C and ECT-M. For a more comprehensive, although in some aspects now outdated, review of this topic other sources are available (Monroe, 1991; Stephens et al. 1993).
DEFINITIONS
To enhance communication between clinicians, the following definitions concerning ECT-C and ECT-M have been agreed upon and are fairly consistently used in the literature :
- Index-episode ECT refers to the ECT course used to treat the acute stage of an illness (Stephens et al., 1993).
- Relapse is "the exacerbation of an ongoing episode after an initial suppression of sym" (Consensus Development Panel, 1985)
- Recrrence is "a new episode following a complete recovery that has lasted at least several mon" (Consensus Development Panel, 1985)
- Continuation ECT (ECT-C), also called consolidation ECT, refers to ECT given immediately after an indexepisode ECT course to prevent relapse of the depressive episode (Stephens et al. 1993). The American Psychiatric Association (APA) Task Force on Electroconvulsive Therapy (1990) recommended that ECT-C should begin immediately after an index-episode ECT course and continue for at least 6 months.
- Maintenance ECT (ECT-M), sometimes called prophylactic ECT, is defined as ECT given at least 6 months after the index-episode ECT course and follows ECT-C in order to prevent recurrence of the depressive illness (APA, 1990).
As the time frame of 6 months constitutes a somewhat artificial boundary between ECT-C and ECT-M, the term follow-up ECT (ECT-F) is also employed, referring to both ECT-C and ECT-M (Stephens et al., 1993). In accordance with existing conventions, we will be using these definitions throughout this paper.
OVERVIEW OF THE HISTORY OF FOLLOW-UP ELECTROCONVULSIVE THERAPY
Favourable clinical experiences with ECT-M in depression and schizophrenia (Moore, 1943; Kalinowsky, 1943) were published just five years after Cerletti and Bini (1938) reported the first therapeutically successful ECT. A few years later, Stephenson and Geoghegan (1951) published the first controlled trial with similarly encouraging results. In the 1940s and 1950s, ECT-F was widely used for a range of functional and organic psychiatric disorders; however, there was no differentiation between the continuation and maintenance phases of treatment until the late 1980s (Decina et al., 1987). From the early 1960s, ECT-F fell into disrepute, although it did not completely disappear from clinical practice (Asnis & Gabriel, 1976). Despite the availability of efficacious anti- depressant and antipsychotic drugs, the practice of ECT-F continued, particularly in private settings as attested to by representative surveys from the USA (Kramer, 1987; APA ECT Task Force Report, 1978) and the UK (Pippard & Ellam, 1981). During the past decade, ECT-F has attracted considerable interest and has now been included in recent practice guidelines (APA, 1990; Royal College of Psychiatrists, 1995).
CURRENT USE OF FOLLOW-UP ELECTROCONVULSIVE THERAPY
Currently, ECT-F is increasingly used in unipolar and bipolar depression, mania, schizo-affective disorder, schizophrenia, catatonic syndromes of various aetiologies, obsessivecompulsive disorder, and even in Parkinson 's disease (Aarsland et al., 1997). However, as depressive disorder has been the main indication, this review will discuss the role of ECT-F in the long-term treatment of depression, unless otherwise specified.
Latey and Fahy (1985) found that 25% of Irish and British psychiatrists used ECT-M. Kramer (1987) reported that 60% of the American psychiatrists responding to his survey used ECT-F. Although a sizeable proportion of psychiatrists use ECT-F, particularly in geriatric psychiatry (Loo et al., 1991), its current practice is still based on clinical wisdom rather than controlled prospective studies comparing ECT-F with maintenance pharmacotherapy. ECT-F is administered with varying treatment frequencies and different electrode placements and waveforms, with or without ongoing pharmacotherapy.
Nowadays, ECT-F is usually delivered on an outpatient basis {proposed first by Kerman as early as 1947), which has been made possible by several technical developments, including the use of brief-pulse wave machines, unilateral electrode placement, exact measurement of the energy delivered, and the utilisation of seizure threshold in choosing stimulus parameters. An implantable venous device placed in the forearm that can be used for more than 30 treatments is another recent technical advance (Mackenzie et al., 1996).
THE RATIONALE FOR FOLLOW-UP ELECTROCONVULSIVE THERAPY
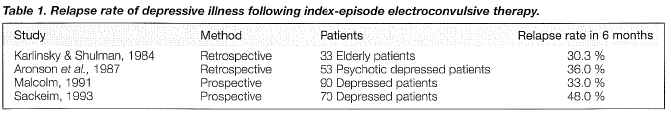
Early studies administering placebo after a successful course of ECT reported a relapse rate of approximately 50% within 6 months following the index course of treatment. Currently, antidepressant medication is the common choice for continuation therapy after an effective index-episode ECT course. Earlier investigations showed that continuation pharmacotherapy reduced the post-ECT relapse rate to 20% (Seager & Bird, 1962; Imlah et al., 1965; Kay et al., 1970). However, more recent studies demonstrated a considerably higher relapse rate after index-episode ECT as summarised in Table,1.
The relapse rate becomes significantly higher with a longer follow-up period. Aronson et al. (1987) found that 72% of depressed subjects relapsed within one to four years following an index-course of ECT despite antidepressant and lithium maintenance treatment. Similarly, 32 of 37 delusional depressed patients responded to ECT in another series although 50% relapsed after one-year (Spiker et al., 1985).
Sackeim et a l. (1990) found that the relapse rate of major depressive episodes following index-episode ECT was significantly higher among medication-resistant patients despite adequate post-ECT pharmacotherapy. Sackeim (1994) cautioned against giving the same class of antidepressant medication for continuation therapy which had been ineffective before the index-course ECT.
INDICATIONS FOR FOLLOW-UP ELECTROCONVULSIVE THERAPY
According to recent guidelines (APA, 1990; Royal College of Psychiatrists, 1995) ECT-F could be considered in the extended treatment of depressive disorders under the following circumstances: (1) severe and frequently recurring episodes of depressive illness that have been treated successfully with an index-episode ECT course; (2) proven resistance to antidepressant medication, intolerable side effects, or lack of treatment adherence with medication regimens; and (3) the patient's acceptance of ECT-F and his/her willingness and ability to give informed consent. Schwarz et a l. (1995) suggested further refinement of indications for ECT-F, including repeated hospitalisation (on average 7 times) and multiple trials with various psychotropic agents (at least 5). Previous history of suicide attempts by drug overdose may constitute an additional indication when considering ECT-F (Hay & Bernadt, 1998). Old-age or physical frailty do not seem to be a contraindication to ECT-F as attested by several old and recent case reports and case series (Wolff , 1957; Dubin et al., 1989; Frances et al., 1989).
Although these guidelines focus almost exclusively on depressive illness, there have been several reports on the use of ECT-F in schizophrenia, schizo-affective and bipolar affective disorders and Parkinson's disease (Moore, 1943; Kalinowsky, 1943; Hoflich et al., 1995; Schwarz et al., 1995; Stiebel, 1995). In these instances, ECT-F was guided by the close monitoring of the patients and clinical wisdom.
Abrams (1992) recommends seeking a second opinion "before continuing maintenance ECT for more than 1 year or 12 treatments" in order to avoid idiosyncratic practice or abuse of ECT-F. In view of the uncertainties surrounding ECT-F, the authors of this paper feel that a second opinion by an experienced consultant psychiatrist must be sought in every case before commencing ECT-F.
EVIDENCE FOR THE EFFICACY OF FOLLOW-UP ELECTROCONVULSIVE THERAPY
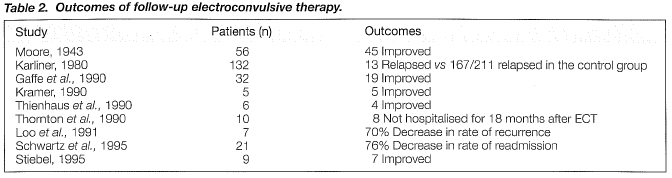
The literature on ECT-F is comprised of case reports and small case series only and is fraught with methodological shortcomings. A review of 14 studies published between 1949 and 1990 on the efficacy of ECT-F found only three controlled trials, with only one of them having matched controls (Monroe, 1991). In none of the studies was the outcome assessed blindly. The total number of patients in the 14 studies was 807 of whom only 325 had unequivocal major depressive illness. Of the 325 patients, 121 presented with psychotic features and another 85 were diagnosed with bipolar depression. Most studies did not differentiate between ECT-C and ECT-M. ECT dosing schedules and concurrent use of psychotropic medication were not standardised or controlled. The duration of ECT-F course ranged from one month to six years (mean 33.4 months). The majority of researchers favoured individual titration of ECT, when the interval between each ECT-F is gradually increased until the patient shows early signs of relapse or recurrence, in order to determine the lowest frequency of ECT-F required to keep the patient in remission. It is encouraging to note that every study yielded positive results, that is, ECT-F was shown to reduce the relapse or recurrence rate. ECT-F seemed to be particularly effective i n t he elderly and those with frequently recurring or psychotic depression. In view of the methodological their suffering, particularly if the long-term side effects of ECT are likely to be mild and mostly preventable. During the past four decades, thousands of patients have undergone ECT-F and greatly benefited in terms of reduced risk of relapse and hospital re-admission without lasting damage to their mental or somatic condition (Monroe, 1991; Stephens et al., 1993). In a double-blind, controlled trial comparing ECT-C with imipramine, ECT-C was found to be both safer and more effective (Gandaghar et al., 1982). In the same study, serial electroencephalogram revealed no evidence of brain dysfunction attributable to ECT-C.
Exposure to repeated anaesthesia is a potential source of side effects. However, with caref ul pre-ECT medical screening and the involvement of an experienced anaesthetist, the risks of repeated anaesthesia are negligible. Post-ECT confusion is a rare adverse event and can be effectively dealt with by decreasing the frequency of consecutive ECTs (Sackeim et al., 1986).
COGNITIVE SIDE EFFECTS
There have been no systematic studies addressing the issue of permanent cognitive defects following ECT-M. Anecdotal evidence suggests that cognitive side effects are, if not negligible, probably not serious. Wolff (1957) treated 268 elderly patients with various organic psychiatric disorders and found no clinically significant cognitive impairment. Hastings (1961) reported the case of a 56-year-old man with severe bipolar illness who underwent 147 ECT seizures during 20 years without adverse effects on his cognitive functions. In a retrospective chart review, Thornton et al. (1990) found 10 patients who had been given ECT-M between 1981 and 1987. The three patients, who were thorougly tested neuropsychologically before and after ECT-M, showed no deterioration in their cognitive functions. Grunhaus et a l. (1990) examined the clinical course of 10 patients undergoing ECT-M and found that short-term memory was slightly impaired by the treatment, but the mild memory disturbances lasted only a few months following the termination of ECT-M. Thienhaus et a l (1990) followed six elderly patients receiving ECT-M for a period of six months to five years. Repeated Mini-Mental State Examinations (MMSE) failed to demonstrate significant changes in their cognitive functions, although MMSE may not be a sufficiently sensitive tool to measure subtle changes in cognitive functioning. Barnes et al. (1997) reported a 74-year-old woman who received more than 400 treatments of ECT-M over a six-year period. These investigators found no evidence of progressive cognitive deterioration. However, there was no baseline cognitive assessment and the patient had a life-long low IQ thus a 'floor effect' might have concealed significant deterioration.
To sum up, preliminary evidence suggests that ECT-M does not cause lasting, progressive cognitive impairment. The APA Taskforce on ECT (1990) recommends cognitive assessment following every third treatment in the course of ECT-F. Stephens et al. (1993) consider the evaluation of 10 orientation, short- and long-term memory, and subjective memory complaints as minimal requirements for cognitive tests accompanying ECT-F, while standardised tests including the MMSE and the Wechsler Memory Scale are regarded as optional but more accurate approximations of changes in cognitive functions due to ECT-F.
ETHICAL CONSIDERATIONS
ECT-F is still practised on the basis of clinical lore, uncontrolled studies, and anecdotal observations. Since its potential for permanent harmful effects, although unlikely, cannot completely be ruled out, extra caution should be exercised with its application. It is essential to document in detail the need for ECT-F and, as mentioned before, seek a second opinion prior to embarking on a course of treatment. Informed consent for ECT-F is another sensitive issue. Most patients who are candidates for ECT-F are severely incapacitated and may not be able to give informed consent. In such cases the involvement of the family is crucial, as is the clarification of the proper legal framework within which the treatment can be carried out. Most authors and official guidelines (APA, 1990; Stephens et al., 1993) require the signing of a separate consent before starting ECT-F because the consent for the index-course ECT becomes invalid. Renewal of the consent for ECT-F should be sought at six-month intervals (APA, 1990) or after every third ECT (Stephens et al., 1993).
FUTURE RESEARCH DIRECTIONS
Scientifically sound evidence for the efficacy and costeffectiveness of ECT-F is still lacking. In terms of clinical practice, the development of detailed treatment guidelines for ECT-F is urgently needed. In Sackeim's opinion, future studies will have to pay attention to two aspects of ECT-F (Sackeim, 1994). The first is the target population. The most relevant population should consist of patients who repeatedly relapse on adequate continuation of pharmacotherapy. It would also be desirable to study the outcome of ECT-F as a first choice continuation therapy, but this approach may be hindered by high refusal and drop-out rates. The second issue is the comparison of ECT-F with other forms of continuation/maintenance treatment. It is evident that comparison of ECT-F with adequate pharmacotherapy is the most reasonable approach.
CONCLUDING REMARKS: THE FUTURE OF FOLLOW-UP ELECTROCONVULSIVE THERAPY IN HONG KONG
The aim of this review was to provide the most recent essential information on ECT-F for psychiatrists practicing in Hong Kong. In our opinion, which is based on our clinical experience with ECT-F and also on the early results of an ongoing controlled trial with this treatment modality, the shortcomings listed above, these results, although promising, should be regarded as preliminary. Some of the most frequently cited studies are summarised in Table 2.
FREQUENCY AND DURATION OF FOLLOW-UP ELECTROCONVULSIVE THERAPY
Moore (1943) administered ECT-M monthly but, in line with contemporary practice, up to 7 seizures were induced within two to three days resembling the practice of the socalled multiple-monitored ECT in which several seizures are induced in a single treatment session (Maletzky, 1981). Some other earlier reports described weekly ECT-F extending over periods of five years or more (Hastings, 1961; Karliner & Wehrheim, 1965; Stevenson & Geoghegan, 1951). The APA Task Force on ECT (1990) identified the most prevalent ECT-F practice in the United States as follows: "treatments are started on a weekly basis, with the interval between treatments gradually extended to a month, depending on the patient's response".
With the lack of strict guidelines, the basic principle of administering ECT-F is still a flexible, individualised approach, depending on the patient's response and the clinician's experience (Fink, 1987; Stephens et al., 1993; Royal College of Psychiatrists, 1995; Hay & Bernadt, 1998). The treating clinician has to monitor the treatment response closely and decide whether to proceed with ECT-F before each session. Evaluating confusion and cognitive side effects is pivotal (Hay & Bernadt, 1998) and any newly arising psychopathological phenomenon warrants revision of the treatment schedule.
The frequency of ECT-F should be determined on the basis of the past history and particularly the course of the depressive illness. In the case of treatment-resistant, continuous depressive symptoms, ECT-F is used to suppress symptoms on an ongoing basis, therefore early detection of the recurring symptoms should guide the frequency and duration of ECT-F. Strictly speaking, this type of ECT-F is essentially a protracted treatment of a long-lasting depressive episode rather than a prophylactic intervention (Wolff , 1957; Kerman, 1957). On the other hand, if the depressive illness is characterised by an episodic course with frequent recurrences and symptom-free intervals, then the length of the previous episodes should govern the frequency of ECT-F (Mori, 1953). In both cases flexibility and a close working relationship with the patient and his/her family is of crucial importance.
The literature is conspicuously vague about the termination of ECT-F. Stephens et al. (1993) suggested that "monthly treatments are continued until the patient' s condition warrants the termination of ECT-F". Acknowledging that the situation "appears strange" , Fink (1987) states that "maintenance therapy is usually terminated when the patient has been asymptomatic for a period that both patient and therapist agree warrant further treatment unnecessary". Monroe (1991) admits "our ignorance and lack of
expertise" in deciding how to plan properly a course of ECT-F. Clearly, prospective, controlled studies should address this issue. A frequently used empirical strategy is to lengthen the interval between consecutive treatments while closely observing the patient for early signs of recurrence. After a symptom-free interval of longer than "several of the previous cycle lengths" of depressive episodes (Consensus Development Panel, 1985), discontinuation of ECT-F could be attempted.
CONCURRENT DRUG AND OTHER SOMATIC TREATMENT MODALITIES
In the first decade following its introduction, it was common practice to combine ECT-F with other forms of somatic treatment such as insulin coma or cardiazol-shock (Moore, 1943; Weisz & Creel, 1948). Continuing antidepressant and/or antipsychotic medication during the course of ECT-F is still a contentious issue. Before the era of modern antidepressants, hundreds of patients had been successfully treated with ECT-F as the sole therapeutic regimen (Moore, 1943; Gallinek, 1948). An early study (Seager & Bird, 1962) reported no advantage of combining antidepressants with ECT. However, in the majority of recent publications, patients given ECT-F were given concomitant antidepressant drugs (Decina et al., 1987; Jaffe et al., 1990; Thornton et a I., 1990) although there have been studies reporting good results with ECT-C alone (Gandaghar et al., 1982; Clarke et al., 1989). Gujavarty et al. (1987) suggested that combining antipsychotic drugs with ECT might be more effective than ECT alone for psychotic depression.
From a clinical point of view, it certainly makes sense to use ECT-F without concomitant medication for three reasons. Firstly, to avoid the possible adverse interaction between ECT and medication. Secondly, co-administration of ECT-F with psychotropic drugs renders the evaluation of the efficacy of either treatment modality virtually impossible. Thirdly, most patients referred for ECT-F did not respond to medication or experienced intolerable side effects, therefore concomitant medication is not only useless but potentially harmful as well. Due to the lack of controlled studies comparing ECT-F with and without pharmacotherapy, only an individualised approach can be advocated based on the treatment response and side effects of previous pharmacotherapy.
ADVERSE EFFECTS OF FOLLOW-UP ELECTROCONVULSIVE THERAPY
When evaluating the side effects of ECT-F, we must bear in mind the clinical condition and the quality of life of the target population. This group of chronically ill, incapacitated individuals at high risk of suicide are resistant to pharmacotherapy and afflicted with either permanent low mood or recurrent bouts of disabling depression. Careful weighting of the risks and benefits of ECT-F for such patients would often indicate a long course of ECT rather than prolonging evidence to support its clinical usefulness and applicability, albeit preliminary, is sufficient enough to consider its introduction in local clinical practice. Offering ECT-F on an outpatient basis, as has been done in many overseas settings, could prove particularly convenient and useful f or both patients and psychiatric services by reducing the need for repeated admissions and, as a consequence, reducing the cost of psychiatric treatment.
While the Quality Assurance Subcommittee for Psychiatry of the Hospital Authority (Cheung, 1997) has commissioned and issued state-of-the-art cogent guidelines on the use of ECT, we are not aware of any scientifically sound survey of the public image of ECT in Hong Kong or the extent of its use in the local public or private psychiatric sector. The persistent stigma of mental illness coupled with occasional articles on ECT in the lay press would indicate that the acceptance of a protracted course of ECT might be very slim. Further steps aiming at the wider recognition and use of ECT-F would require public education, regular audits of the practice of ECT, and encouragement for local psychiatrists, particularly senior trainees, to conduct research in different aspects of ECT including ECT-F.
REFERENCES
Aarsland D, Larsen JP, Waage 0, Langeveld JH. Maintenance electroconvulsive therapy for Parkinson's disease. Convulsive Ther 1997;13:274-277.
Abrams R. Electroconvulsive therapy. 2nd ed. New York, Oxford: Oxford University Press, 1992.
American Psychiatric Association. Electroconvulsive therapy: report of the task force on electroconvulsive therapy of the American Psychiatric Association: APA Task Force Report No. 14., Washington DC, 1978.
American Psychiatric Association. The practice of electroconvulsive therapy: recommendations for treatment, training and privileging. Washington, DC: APA 1990.
Aronson TA, Shukla S, Hoff A. Continuation therapy after ECT for delusional depression: a naturalistic study of prophylactic treatments and relapse. Convulsive Ther 1987;3:251-259.
Asnis G, Gabriel AN. ECT as maintenance therapy in schizophrenia. Am J Psychiatry 1976;133:858-859.
Barnes RC, Hussein A, Anderson DN, Powell D. Maintenance electroconvulsive therapy and cognitive function. Br J Psychiatry 1997;170:285-287.
Cerletti V, Bini L. Un nuevo metodo di shockterapie "fettroshock". (The First Method of Shocktherapy "Electroshock"). Bull Acad Med Roma 1938;64:136-138.
Cheung HK. Administration of electro-convulsive therapy (ECT). Psychiatric Clinical Guidelines. The Quality Assurance Subcommitte of the Coordinating Committee in Psychiatry 1997;4-9.
The Clarke TB, Coffey CE, Hoffman GW, et al. Continuation therapy for depression using outpatient electroconvulsive therapy. Convulsive Ther 1989;5:330-337.
Consensus Development Panel. Mood disorders: pharmacologic prevention of recurrences. Am J Psychiatry 1985;142:469-476.
Decina P, Guthrie EB, Sackeim HA, et al. Continuation ECT in the management of relapses of major affective episodes. Acta Psychiatr Scand 1987;75:559-562.
Dubin WR, Jaffe RL, Roemer RA, et al. Maintenance ECT in coexisting affective and neurological disorders. Convulsive Ther 1989;5:162-167.
Fink M. Maintenance ECT and affective disorders. Convulsive Ther 1987;3:249-250.
Fink M. Impact of the antipsychiatry movement on the revival of electroconvulsive therapy in the United States. Psychiatr Clin North Am 1991;14:793-801.
Frances A, Weiner RD, Coffey CE. ECT for an elderly man with psychotic depression and concurrent dementia. Hosp Community Psychiatry 1989;40:237-242.
Gallinek A. The nature of affective and paranoid disorders during the senium in the light of electric convulsive therapy. J Nerv Ment Dis 1948;108:293-303.
Gandaghar BN, Kapur RL. Comparison of electroconvulsive therapy with imipramine in endogenous depression: a double-blind study. Br J Psychiatry 1982;141:367-371.
Grunhaus L, Pande AC, Haskett RF. Full and abbreviated courses of maintenance electroconvulsive therapy. Convulsive Ther 1990;6: 130-138.
Gujavarty K, Greenberg LB, Fink M. Electroconvulsive therapy and neuroleptic medication in therapy-resistant positive-symptom psychosis. Convulsive Ther 1987;3:185-195.
Hastings OW. Circular manic-depressive reaction modified by "prophylactic electroshock." Am J Psychiatry 1961;118: 258-260.
Hay AG, Bernadt M. Electroconvulsive therapy and other treatments. In: Stein G Wilkinson G, eds. General adult psychiatry. London: Gaskell, 1998;220-242.
Hoflich G, Kasper S, Burghof KW, et a l. Maintenance ECT for treatment of therapy-resistant schizophrenia and Parkinson's disease. Biol Psychiatry 1995;37:892-894.
lmlah NW, Ryan E, Harrington JA. The influence of antidepressant drugs on the response to electroconvulsive therapy and on subsequent relapse rates. Neuropsychopharmacology 1965;4:438-442.
Jaffe R, Dubin W, Shoyer B, et al. Outpatient electroconvulsive therapy: efficacy and safety. Convulsive Ther 1990;6:231-238.
Kalinowsky LB. Electric convulsive therapy, with emphasis on importance of adequate treatment. Arch Neural Psychiatry 1943;50: 652-660.
Karliner W, Wehrheim HK. Maintenance convulsive treatments. Am J Psychiatry 1965;121:1113-1115.
Karliner W. Maintenance ECT. J Psychiatr Treatment Eva! 1980;2: 313-314.
Karlinsky H, Shulman KI. The clinical use of electroconvulsive therapy in old age. J Am Geriatr Soc 1984;32:183-186.
Kay OW, Fahy T, Garside RF. A 7-month double-blind trial of amitriptyline and diazepam in ECT-treated depressed patients. Br J Psychiatry 1970;117:667-671.
Kerman EF. The efficacy of electroshock therapy in preventing or shortening hospitalization. J Nerv Ment Dis 1947;106:1-10.
Kerman EF. Prevention of recurrence of mental illness with modified prophylactic electroshock therapy. Dis Nerv Syst 1957;18: 189-191.
Kramer BA. Maintenance ECT: a survey of practice (1986). Convulsive Ther 1987;3:260-268.
Kramer BA. Maintenance electroconvulsive therapy in clinical practice. Convulsive Ther 1990;6:279-286.
Kupfer DJ. Long-term treatment for depression. J Clin Psychiatry 1991;52 (Suppl.):28-34.
Latey RH, Fahy TJ. Electroconvulsive therapy in the Republic of Ireland 1982: a summary of findings. Br J Psychiatry 1985;147: 438-439.
Loo H, Galinowski A, De Carvalho W, et al. Use of maintenance ECT for elderly depressed patients. Am J Psychiatry 1991;148:810.
Mackenzie TB, Thurston J, Rogers L, Hunter OW. Placement of an implantable venous access device for use in maintenance ECT. Convulsive Ther 1996;12:122-126.
Malcolm K, Dean J, Rowlands P, Peet M. Antidepressant drug treatment in relation to the use of ECT. J Psychopharmacol 1991; 5:255-258.
Maletzky BM. Multiple-monitored electroconvulsive therapy. Boca Raton. CRC Press, 1981.
Monroe RE. Maintenance electroconvulsive therapy. Psychiatr Clin North Am 1991;14:947-960.
Moore NP. The maintenance treatment of chronic psychotics by electrically induced convulsions. J Ment Sci l943;89:257-269.
Mori J. Electric shock therapy as a preventive measure of periodical mental derangement. Folia Psychiatr Neural Jpn 1953;7 :209-213. Pippard J, Ellam L. Electroconvulsive treatment in Great Britain. Br J Psychiatry 1981;139:563-569.
Royal College of Psychiatrists. The ECT handbook. London: Royal College of Psychiatrists, 1995.
Sackeim HA, Portnoy S, Neeley P, et al. Cognitive consequences of low-dosage electroconvulsive therapy. Ann NY Acad Sci l986;462:326-340.
Sackeim HA, Prudic J, Devanand DP, et al. The impact of medication resistance and continuation pharmacotherapy on relapse following response to electroconvulsive therapy in major depression. J Clin Psychopharmacol 1990;10:96-104.
Sackeim HA, Prudic J, Devanand DP, et a l. Effects of stimulus intensity and electrode placement on the efficacy and cognitive effects of electroconvulsive therapy. N Engl J Med 1993;328: 839-846.
Sackeim HA. Continuation therapy following ECT: directions for future research. Psychopharmacol Bull 1994;30:501-521.
Schwarz T, Loewenstei n J, Isenberg KE. Maintenance ECT: indications and outcome. Convulsive Ther 1995;11:14-23.
Seager CP, Bird RL. lmipramine with electrical treatment in depression: a controlled trial. J Ment Sci 1962;108:704-707.
Spiker DG, Stein J, Rich CL. Delusional depression and electroconvulsive therapy: one year later. Convulsive Ther 1985;1: 167-172.
Stephens SM, Pettinati HM, Greenberg RM, Kelly CE. Continuation and maintenance therapy with outpatient ECT. In: Coffey ECE, ed. The clinical science of electroconvulsive therapy. Washington DC: Ame1ican Psychiatric Press, 1993;143-164.
Stevenson GH, Geoghegan JJ. Prophylactic electroshock: a five year study. Am J Psychiatry 1951;107:743-748.
Stiebel V. Maintenance electroconvulsive therapy for chronic mentally ill patients: a case series. Psychiatric Services 1995;46:265-268. Thienhaus OJ, Margletta S, Bennett JA. A study of the clinical efficacy of maintenance ECT. J Clin Psychiatry 1990;51:141-144.
Thornton JE, Benoit HM, Dealy R, et al. Retrospective study of maintenance electroconvulsive therapy in a university-based psychiatric practice. Convulsive Ther 1990;6:121-129.
Weisz S, Creel JN. Maintenance treatment in schizophrenia. Dis Nerv Syst 1948;9:10-14.
Wolff GE. Results of four years active therapy for chronic mental patients and the value of an individual maintenance dose of ECT. Am J Psychiatry 1957;114:453-456.
Dr WK Tang, MBBS, MRCPsych, Medical Officer, Department of Psychiatry, Prince of Wales Hospital, Hong Kong, China.
Dr GS Ungvari, MD, PhD, FHKAM(Psych), FRANZCP, FHKCPsych, MRCPsych, Associate Professor, Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong, China.
Address for Correspondence: Dr WK Tang
Department of Psychiatry 11/F, Prince of Wales Hospital Shatin, NT
Hong Kong, China.