Hong Kong Journal of Psychiatry (1997) 7 (2) 19-25
SPECIAL TOPIC: SCHIZOPHRENIA
Summary
The study examined the functioning of families with a schizophrenic member along the six dimensions proposed in the McMaster model of family functioning. It also investigated whether social support to families is related to healthy family functioning. The sample include 61 families with an unremitting schizophrenic member, 59 families with a remitting member, a non-clinical control group of 89 subjects. The Family Assessment Device is the major measurement used to evaluate family functioning. The study found that families with remitting members had family functioning similar to the non-clinical control whereas those with unremitting members functioned poorly. Social support was strongly related to various dimensions of family functioning. Satisfaction with relatives' support was the most significant factor. This underscores the importance of a family perspective in providing treatment and the significance of social support in strengthening the families.
Keywords:Schizophrenia, family functioning, McMaster model, social support
INTRODUCTION
Schizophrenia is a serious and disabling illness which is characterized by abnormalities of thinking, feeling and behavior. Almost 1% of people worldwide develop this illness during their lifetime, and in the United States, about 2 million persons are affected (Tomb, 1995). Most schizophrenics spend many years in a residual phase when they may be withdrawn and isolated, suffer from peculiar, unsatisfactory social skills, living skills and social performance, and display minor features of the illness (Gerhart, 1990; Hegarty et al., 1994; Straube & Hahlweg, 1990). In Hong Kong, it is estimated that some 13,000 people are suffering from the disorder (Hong Kong Government, 1996). Just like the situation elsewhere, some 30% of expatients may still be symptomatic at their follow-up assessments, and their work experience and heterosexual relationships are far from satisfactory (Lee et al., 1991).
Thanks to the innovation of new treatment techniques and the deinstitutionalization movement, most of the schizophrenics are able to return to their family after only a brief stay in a mental hospital (Goldman, 1982; Lamb & Oliphant, 1978). The family has thus become an important agent affecting the patients' mental conditions and the course of recovery. Conversely, the patients also create enormous hardship for their family. Identifying aspects of family functioning contributing to the rehabilitation or relapse of the patients and the support required to strengthen the families is therefore of great concern to mental health practitioners.
THE ROLE OF THE FAMILY AND THE McMASTER MODEL
In the last two decades, increasing research studies have been conducted on the role of the family in the course of schizophrenia. Though the family as a causal factor of schizophrenia has been disputed (Hatfield, 1987), researchers still recognize the importance of the family environment as a contributing factor to the relapse or rehabilitation of the patient. The major concern has been shifted to the post-hospital adjustment of discharged patients and the role of the family as a rehabilitation agent for schizophrenia. In particular, the concept of expressed emotion (EE), which refers to the attitudes of the family members towards the patient (critical comments, hostility, emotional over-involvement, warmth and positive remarks) are found to significantly and reliably predict the relapse of schizophrenics (Leff & Vaughn, 1985). This concept has laid the ground for the family interventions aiming at reducing the negative impacts of the relatives on the patients' further rehabilitation and recovery (e.g., Leff, Kuipers, Berkowitz, & Sturgeon, 1982; Tarrier et al., 1988).
However, the concept of EE is not without its problem. Hardesty and McGill (1985) commented that EE studies seem to emphasize too much on the prevention of the patients' relapse and do not pay enough attention to helping the family as a whole to function healthily. Hatfield (1987) criticized the EE concept in that it draws professionals' attention to the negative characteristics of the families but fails to provide a more comprehensive and empathic understanding of the family members. Furthermore, categorizing the families of schizophrenic patients into high-EE and low-EE may just be another attempt to label the families and evade an understanding of the complex human interactions involved (Hatfield, Spaniol & Zipple, 1987).
Instead of focusing on a single dimension, an approach which embraces a broader view of family functioning would appear more useful. The McMaster Model of family functioning (Epstein, Baldwin & Bishop, 1983) provides an important conceptual tool for this purpose. The model is based on the holistic principles of the general systems perspective. It assumes that family structure and organization are important in determining the behaviors of the family members, and transactional patterns in the family system are involved in shaping the behavior of the family members.
This model proposes that families can be understood along six dimensions: (a) problem solving, which concerns the family's ability to proceed through seven steps from problem identification to problem resolution in both instrumental and affective areas; (b) communication, which refers to the effectiveness and extent of the family's style of communication, and effective communication is considered as the transmission of clear and directive verbal messages; (c) roles, which are the recurrent patterns of behavior necessary to fulfill the instrumental and affective needs of family members; (d) affective responsiveness, which measures the capacity of family members in giving response with the appropriate quality and quantity of feelings to a wide range of stimuli, e.g. love, happiness, anger and sadness; (e) affective involvement, which refers to the amount of interest, care and concern family members invest in one another; and (f) behavioral control, which defines the family's style of maintaining discipline and standards of behavior, e.g. flexible or rigid.
The McMaster Family Assessment Device (FAD) is the instrument developed out of this model to assess the different dimensions of family functioning. A number of studies found that FAD is a reliable and valid assessment of a wide range of families in non-clinical, psychiatric, and medical samples (Epstein, Baldwin & Bishop, 1983; Miller, Epstein, Bishop & Keitner, 1985; Kabacoff, Miller, Bishop, Epstein & Keitner, 1990). It is also a useful tool for practitioners to identify families at risk (Akister & Stevenson-Hinde, 1991). Despite its popularity in western societies, FAD and the McMaster model have not been applied in Hong Kong. Whether families with schizophrenic patients are deficient in certain dimensions of functioning is still an unanswered question.
SOCIAL SUPPORT TO FAMILIES
As mentioned earlier, families with an ex-mentally ill person are under great stress. The family members may encounter problems such as the impairment of health or well-being, restriction of social activities, worry about patient's situation and relapse, financial impairment, familial conflict, and disturbance of domestic routines (Chan, 1995; Lieh-Mak & Pan, 1987; Wu, 1995). An important issue is to identify means that may enable these families to function well. The notion of 20 social support has been considered an important factor in this regard (Cobb, 1976; Cohen & Mckay, 1984; Heller & Swindle, 1983; Thoits, 1982). Numerous studies have indicated that social support functions as a rotection against pathology" by (a) helping people mobilize their psychological resources in order to deal with emotional problems, (b) sharing people tasks, and (c) providing individual with money, materials, tools, skills, information and advice to deal with particular stressful situations (Antonucci & Israel, 1986; Caplan, 1974; Cohen & Mckay, 1984; Krahn, 1993). Research has gathered evidence that family with a schizophrenic patient suffers from network contraction and condensation (Upton et al., 1981). This will increase the vulnerability of the family to stressors due to the resulting lack of social support. At present, programmes have been carried out in Hong Kong by agencies to help families of the mentally ill, but research in relevant areas are still scant (see Ma, 1992 for a review). How the types and sources of social support would be related to family functioning is an under-explored area.
The present study evaluates the relevance of the different dimensions of family functioning to the recovery of a schizophrenic member. Specifically, we examined how the family functioning dimensions differ in the remitting patients and the unremitting patients who still manifest a considerable number of symptoms. Furthermore, we investigated how the types and sources of social support relate to the different dimensions of family functioning. By identifying the useful social support dimensions, positive measures can be implemented to strengthen the functioning of the families, which in turn prevent the schizophrenics from relapse.
METHOD
RESPONDENTS
The present sample includes a clinical group and a nonclinical control group. The clinical sample consists of 120 subjects who lived with a schizophrenic family member and were the principal caregivers. The schizophrenic family members were all adults. All of them had the experience of hospitalization but were then receiving services from day activity centres, sheltered workshops or psychiatric out-patients clinics in Hong Kong. Only the service units of three major nongovernmental organizations and two out-patient clinics were included in the study.1 A random sample of schizophrenics were drawn from the lists of schizophrenic patients provided by the service units, and the principal caregivers of these people were invited to participate in the present study. Those who indicated their consent constituted 22.4% of the letters sent, and they were then approached for interviews.
Among the respondents in the clinical group, there were 39 males (32.5%) and 81 females (67.5%). The age ranged from 20 to 88 with a mean age of 54.0. Fitty-seven (47.5%) were over 60 years old. Fifty-nine (49.2%) respondents were married, and 37 (30.8%) respondents' spouses deceased. There were 23 singletons and one was divorced.
The non-clinical control consisted of 89 subjects who were first year Diploma in Social Work students of the City University of Hong Kong. Among the respondents in this group, 22.5% were male and 77.5% were female, with an average age of 22.0 years (SD = 3.91). Most of the respondents (93.3%) in this group were single, while the remaining 6.7% were married. The respondents indicated an absence of any mentally ill patients in their families.
MEASURES
Symptoms Observed in the Schizophrenic Patient
A symptom list originally developed by Wong (1991) to assess the burden experienced by the family caregivers was used in this study to determine symptom remission of the schizophrenic family member. The family caregivers indicated on a four-point scale, from (1) never, (2) seldom, (3) sometimes, to (4) frequently, to represent how frequently the schizophrenic family member had manifested the symptoms, including drug non--compliance, bizarre behavior, eccentric thoughts, emotional agitation, unreasonable behaviors, suicidal thought, apathy, unwillingness to participate in activities, negligence of personal hygiene, gambling, excessive spending etc. The scale has a high internal consistency of 0.89. The possible score ranges from 25 to 100, and a cut-off point of 50 was adopted to differentiate the remitting schizophrenics from those unremitting ones who still manifested a considerable number of negative and active symptoms.
Family Assessment Device (FAD)2
The FAD is a self-reported questionnaire which measures subjects' family functioning along seven dimensions, namely, problem solving, communication, roles, affective responsiveness, affective involvement, behavioral control, and general functioning {Epstein, Baldwin, & Bishop, 1983; Kabacoff et al. 1990; Miller et al., 1985). The FAD sub-scales have been found to demonstrate adequate internal consistency (Cronbach alpha from 0.72 to 0.92), test-retest reliability (from 0.66 to 0.76), and minimal social desirability effects (from O.06 to O.19) (Keitner et al., 1990). The FAD consists of 60 items, to which the respondents indicate their extent of agreement from (1) strongly disagree, (2) disagree, (3) agree, to (4) strongly agree. The Chinese version of FAD was developed by the first author. An expert in translation first translated the FAD into Chinese, and three experts (two psychologists and the second author) were then invited to read word by word and comment on the accuracy and relevance to the Chinese culture. Some amendments were made and the version was further commented by two experts in translation and who were proficient in both English and Chinese. Some minor amendments were made and the final version was completed. The sub-scales demonstrated adequate internal consistency, Cronbach alphas range from 0.68 in behavior control to 0.92 2 The Chinese version of the questionnaire is available with the first author upon written request. in the general functioning sub-scale. High internal consistency is obtained for the overall scale, Cronbach's alpha being 0.97. The scale is scored in the direction of dysfunction; a higher score reflects poorer functioning of the family.
Satisfaction with Types of Social Support Received
The scale was constructed for the purpose of this study. It is composed of 15 items divided into three sub-scales, namely, socio-emotional social support, instrumental social support, and informational social support received by the principal caregivers of the schizophrenics. There are five items in each sub-scale. The principal caregivers of the schizophrenics were asked to rate their satisfaction with the different types of support received along a four point scale, from very dissatisfied to very satisfied. Cronbac's alphas for the socio-emotional, informational, and instrumental social support are 0.93, 0.90, and 0.79 respectively.
class="jnlSubHead">Satisfaction with Support Received from Different Sources
The principal caregivers of the schizophrenics were asked to name the extra-familial members who provided social support to them. They were then asked to rate their satisfaction with the support received along a four point scale, from very dissatisfied to very satisfied .
The data from the clinical group were collected by means of structured interviews, conducted by trained interviewers and the first author. To ensure consistent interpretation of the questionnaire, an intensive training was provided to the interviewers. On the other hand, the data from the normal population were obtained by self-administered questionnaires.
RESULTS
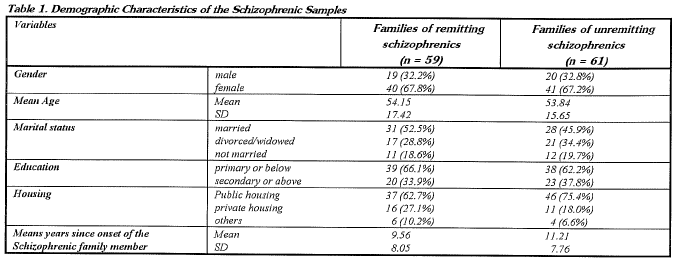
Most of the respondents in the clinical group were parents (64.2%), siblings (15.0%) or spouses (10.8%) of the schizophrenic members. Among the clinical group, 59 were classified as the remitting group, in which the schizophrenic members scored below the cut-off point of 50 in the symptom scale. Sixty one scored above the cut-off point and were classified as the unremitting group. The groups did not differ in the distribution of gender, X,2 (1) = 0.00, age, t(118) = 0.10, marital status, X,2 (2) = 0.58, education level, x2 (1) = 0.18, and housing condition, X,2 (2) = 2.27, all ns. There was no difference between the mean years since onset of the schizophrenic members, t = 1.15, ns (see Table 1). As to the comparison between the non--clinical and the clinical group, the gender distribution was marginally similar, X,2 (1) = 4.17, p < 0.1. However, obviously the non--clinical group was on average younger than the clinical group, and the marital status was quite different. Such differences should be noted, but as we shall argue in our discussion, this would not be a great problem for the interpretation of the data.
Table 2 shows the sub-scale means of the FAD by the three groups. MANOVA found that significant differences existed among the means of the sub-scale scores and the total scale score, Wilks' criterion F(14, 390) = 15.98, p < .001.

Univariate ANOVA followed by multiple comparisons using Bonferroni protected t tests were then performed to examine the differences of individual scale scores. Inspection of Table 2 reveals significant differences among the dimensions of general functioning, problem solving, communication, role, affective involvement, and affective responsiveness of the three groups. The three groups did not differ in the dimension of behavioral control. Except for this sub-scale, the families of the unremitting schizophrenics showed the weakest levels of functioning in the other dimensions. On the other hand, the families of the remitting schizophrenics showed similar levels of functioning with the non-clinical controls.
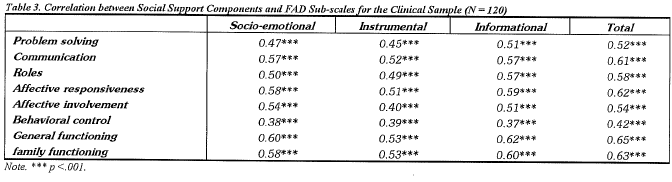
Table 3 presents the correlations among the satisfaction of social support received by the families schizophrenics and the FAD sub-scales scores. All types of social support moderately correlated (ranging from 0.37 to 0.62) with the sub-scales of FAD. The overall correlation between social support and family functioning is 0.63. This provides support to the notion that social support is conducive to family functioning; that is, the higher the social support perceived, the better the family functioning will be, regardless of the symptom levels of the schizophrenics.
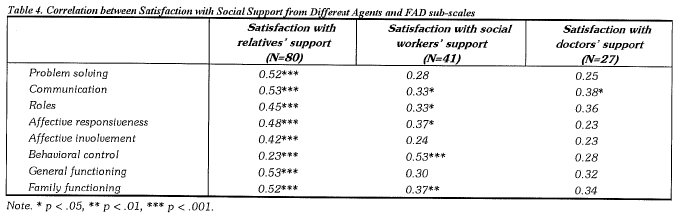
The family members of schizophrenics indicated that they received social support from different parties. Relatives, social workers, and medical doctors were the principal sources of support. The correlations between their degrees of satisfaction with the support obtained and the FAD sub-scale scores are shown in Table 4. Significant correlations were found between the satisfaction with the relatives' support and the FAD subscales. As predicted, the more satisfied the principal caregivers felt, the better the family functioned at all dimensions. However, for the satisfaction of support provided by social workers, significant correlations were found with four dimensions only. A noticeable association was found between the satisfaction with the social workers' support and the behavioral control dimensions of the family functioning. The satisfaction with the doctor support was not quite associated with the family functioning dimensions, with the exception of the family communication.
DISCUSSION
The study investigated the family functioning of the remitting schizophrenics and the unremitting schizophrenics, and compared the different dimensions with the normal controls. We found that the family functioning of the remitting schizophrenics came close to those of the normal controls, while those of the unremitting schizophrenics had poorer family functioning along most dimensions. It is admitted that the non-clinical control group differs in many ways from the clinical group: the respondents were on average younger, received higher education, and were predominantly single. However, the findings that family functioning of the remitting group resembles (rather than falls behind) that of the non-clinical group in many dimensions relieve us of the doubt which may arise out of the non-equivalence. It suggests that families with remitting members indeed were at the "normal" range of functioning.
Specifically, the study shows that family members of the unremitting schizophrenics are less able to show interest and care to one another (affective involvement), have poorer problem solving ability (problem solving), are less able to perform behaviors to fulfill the instrumental and affective needs of the family members (roles), are less able to transmit clear and directive verbal messages (communication), and are less able to give affective responses with appropriate quality and quantity of feelings (affective responsiveness). The design of the study precludes the possibility of inferring causal sequence. On one hand, it can be the case that healthy family functioning is conducive to the rehabilitation of the schizophrenics, while a dysfunctional family pattern may exacerbate the problems of the patient. An alternative interpretation is that as the symptoms of the schizophrenic member remitted, the family functioning was restored. This issue can only be unraveled with the use of more rigorous designs. Anyhow, our findings are in line with the literature on family expressed emotion (Vaughn & Leff, 1976) and communication deviance (Liem, 1980; Singer et al. 1978). In addition, the McMaster model provides a broader picture of the family functioning on the top of the communication dimension emphasized by these specific concepts.
Social support was found to be strongly associated with the functioning of the schizophrenics' families. Socio-emotional support, instrumental support, and informational support are all essential to healthy family functioning. As mentioned, a family with a schizophrenic member is at risk of network contraction and condensation. The family members are often dissatisfied with the social support obtained {Sun, 1994). Thus, active measures must be done to establish supportive network for the families of the schizophrenics. This study shows that among the different sources of social support, those provided by the relatives are most strongly related to family functioning. The roles played by the professionals are also of some importance, particularly the social workers. Thus, to strengthen the functioning of the family of the schizophrenics, one focus will be on the development of informal supportive networks for the families.
The findings of the study have important practice implications. In view of the significance of the family in the course of rehabilitation of the schizophrenics, helping professionals should not just provide individual-focused treatments to the patients but should adopt a family perspective in providing after-care service.
Actually, several models of working with families are available and they address different facets of family functioning. For example, the family members groups organized by Leff, Kuipers, Berkowitz, and Sturgeon (1986) and the behavioral intervention model by Tarrier et al. (1988, 1989) work towards lowering the level of expressed emotion in the families. The dimensions of problem-solving and communication are addressed in the behavioral family management model developed Falloon et al. (1984, 1985). On the other hand, the
psychoeducational approach developed by Hogarty and Anderson (Hogarty et al., 1986, 1991) focuses more on the family management strategies for stress reduction and on the establishment of family structure and routines. From the perspective of the McMaster model, these are all important areas in comprehensive family interventions. In addition, fostering mutual care and concern among the family members is another area that should not be neglected.
This calls for a team work approach in which the medical professionals and those from the other disciplines come together to plan and render more holistic services. In addition to direct treatment by the psychiatric professionals, social workers can have roles to play in involving the families. However, as the findings of the present study show, families with schizophrenic members also need support in order to function adequately. In this regard, the support provided by formal sources is of limited functions, whereas those provided by relatives and informal sources can be extremely valuable. One emphasis of intervention is therefore to expand the natural social networks of the families of the schizophrenics. The supportive model of multiple family group therapy (McFarlane, 1995) is a possible mode of intervention. Several families including the patients are involved in discussions of wide-range issues such as practical issues of living, family rules, management of schizophrenia, or expanding social networks. It provides an opportunity for families with similar problems to meet together and develop mutual support. The self-help organizations for relatives of the mentally disturbed operated by some agencies in Hong Kong carries these features (e.g., the Baptist Oi Kwan Social Service, see Leung, Wong, & Siu, 1993), and it appears to be a promising approach that deserves further attention in the future.
The present study does have its limitations. First, the symptoms of the patients are not evaluated by the psychiatric professionals. Doubts can be raised on the validity of the assessment. This is inevitable in view of the resource limitations. Furthermore, owing to various constraints, data on the initial symptom level of the schizophrenic members and their period of discharge from hospitals are absent, and some variations of the patients' course of the illness may exist. Future research needs to address these issues and examine the relevance of the family functioning by means of a more rigorous design. Nonetheless, the present study serves as a good starting point which employs a wider perspective on the family of the schizophrenics and suggests promising direction for future research and interventions to help the families.
REFERENCE
Akister, J., & Stevenson-Hinde, J. (1991) Identifying families at risk: exploring the potential of the McMaster Family Assessment Device. Journal of Family Therapy, 13: 411-421.
Anderson, C.M., Hogarty, G., & Reiss, D. (1980) Family treatment of adult schizophrenic patients: A psychoeducational approach. Schizophrenia Bulletin, 6: 490-505.
Antonucci, T.C., & Israel, B.A. (1986) Veridicality of social support: A comparison of principal and network members' responses. Journal of Consulting and Clinical Psychology, 54: 432-437.
Berkowitz, R. (1984) Therapeutic intervention with schizophrenic patients and their families: a description of a clinical research project. Journal of Family Therapy, 6: 211-233.
Caplan, G. (1974) Support Systems and Community Mental Health. Behavioral Publications. New York.
Chan, K.F. (1995) The impact of schizophrenia on Hong Kong Chinese families. Hong Kong Journal of Social Work, 29: 21-34.
Cobb, S. (1976) Social support as a moderator of life stress. Psychosomatic Medicine, 38: 300-314.
Cohen, S., & McKay, G. (1984) Social support, stress and buffering hypothesis: A theoretical analysis. In A. Baum, J.E. Singer &
S.E. Taylor (Eds.) Handbook of Psychology and Health. (Vol. 4) (pp. 253-268). Erlbaum. Hillsdale, NJ.
Epstein, N.B., Baldwin, L., & Bishop, D.A. (1983) The McMaster Family Assessment Device. Journal of Marriage and Family Therapy, 9: 171-180.
Falloon, !.R.H., Boyd, J.L., McGill, C.W., Williamson, M., Razani,
J., Moss, H.B., Gilderman, A.M., & Simpson, G.M. (1985) Family management in the prevention of morbidity of schizophrenia. Archives of General Psychiatry, 42: 887- 896.
Falloon, !.R.H., Hardesty, J.P., & McGill, C.W. (1985) Adjustment of the family unit. In !.R.H. Falloon (Ed.) Family Management of Schizophrenia (pp. 102-114). The John Hopkins University Press.
Gerhart, U.C. (1990) Caring for the Chronic Mentally Ill. F.E. Peacock Publishers Inc. Itasca, Ill.
Goldman, H. (1982) Mental illness and family burden: A public health perspective. Hospital and Community Psychiatry, 33: 557-560.
Goldstein, M.J., Rodnick, E.H., Evans, J.R., May, P.R.A. and Steinberg, M.R. (1978) Drug and family therapy in the aftercare treatment of acute schizophrenics. Archives of General Psychiatry, 35: 1169-1177.
Hatfield, A.B. (1987) Families as caregivers: A historical perspective. In A.B. Hatfield & H.P. Lefley (Eds.) Families of the Mentally Ill: Coping and Adaptation (pp. 3-29). Guilford Press. New York.
Hatfield, A.B., Spaniol, L. & Zipple, A.M. (1987) Expressed emotion: A family perspective. Schizophrenia Bulletin, 13(2): 221-226.
Hegarty, J.D., Baldessarini, R.J., Tohen, M., Waternaux, P.H.C., & Oepen, G. (1994) One hundred years of schizophrenia: a meta-analysis of the outcome literature. American Journal of Psychiatry, 151(10): 1409-1416.
Heller, K. & Swindle, R. W. (1983) Social networks, perceived social support, and coping with stress. In R.D. Feiner, L.A. Jason, J.N. Moritsugu & S.S. Farber (Eds.) Preventive Psychology: Theory, Research and Practice, (pp. 87-103). Pergamon. Elmsford, NY.
Hong Kong Government (1996) Hong Kong Review of Rehabilitation Programme Plan. Hong Kong: Government Publication.
Kabacoff , RO., Miller, I., Bishop, D.A., Epstein, N.B., & Keitner, G. (1990) A psychometric study of the McMaster family assessment device in psychiatric, medical and non-clinical samples. Journal of Family Psychology, 3(4): 431-439.
Keitner, G., Ryan, C., Miller, I., Epstein, N., Bishop, D. & Norman, W. (1990) Family functioning, social adjustment and recurrence of suicidality. Psychiatry, , 53: 17-30.
Krahn, R.L (1993) Conceptualizing social support In Families of children with special health needs. Family Process, 32: 325- 248.
Lamb, H. & Oliphant, E. (1978) Schizophrenia through the eyes of families. Hospital and Community Psychiatry, 29: 803- 806.
Lee, P.W.H., Lieh-Mak, F., Yu, KK & Spinks, J.A. (1991) 21st century schizophrenics: Better outcome? Lower costs? Journal of Hong Kong College of Psychiatrists, 1: 37-45.
Leff , J.P. & Vaughn, C. (1985) Expressed Emotion In Families. Guilford Press. New York.
Leff , J.P., Kuipers, L, Berkowitz, R., & Sturgeon, D. (1982) A controlled trial of social intervention in the families of schizophrenic patients. British Journal of Psychiatry, 141: 121-134.
Leung, M.T., Wong, J., & Siu, V. (1993) The emergence of a selfhelp association for relatives of the mentally disturbed in Hong Kong (Baptist Oi !-<:.wan Social Service). In Social Sciences Research Centre & Department of Social Work and Social Administration (ed.) Psychiatric Rehabilitation: The Asian Experience. University of Hong Kong.
Lieh-Mak, F., & Pan, P.C. (1987) Burden on Families of Schizophrenic Patients. Paper presented at First ASEAN Congress on Mental Health, Bangkok, Thailand.
Liem, J.H. (1980) Family studies of schizophrenia: An update and commentary. Schizophrenia Bulletin, 6: 429-455.
Lipton, F.R., Cohen, C.I., Fischer, E., & Katz, S.E. (1981) Schizophrenia: A network crisis. Schizophrenia Bulletin, 7: 144-151.
Ma, J.LC. (1992) Social support, mutual aid groups, the mentally ill and their families. Hong Kong Journal of Mental Health, 21: 16-27.
Mcfarlane, W.R. (Ed.) (1983) Family Therapy in Schizophrenia. Guilford. New York.
Mcfarlane, W.R., Lukens, E., Link, B., Dushay, R., Deakins, S.A., Newmark, M., Dunne, E.J., Horen, B., & Toran, J. (1995)
Multiple-family groups and psychoeduation in the treatment of schizophrenia. Archives of General Psychiatry, 52: 670- 687.
Miller, I., Epstein, N.B., Bishop, D.A., & Keitner, G. (1985) The McMaster Family Assessment Device: Reliability and Validity. Journal of Marital and Family Therapy, 11: 345-356.
Singer, M.T., Wynne, LC., & Toohey, M.C. (1978) Communication disorders and the families of schizophrenics. In LC. Wynne, R.L Cromwell, & S. Matthysse (Eds.), The Nature of Schizophrenia. Wiley. New York.
Straube, E.R., & Hahlweg, K (Eds.) (1990) Schizophrenia: Concept, Vulnerability and Intervention. Springer-Verlag. Berlin.
Sun, Y.K.S. (1994) A Study of the Family Functioning of Families with a Schizophrenic Patient. Unpublished MSW Thesis. Hong Kong: The Chinese University of Hong Kong.
Tarrier, N., Barrowclough, C., Vaughn, C., Bamrah, J., Porceddu, K , Watts, S., & Freeman, H. (1988) The community management of schizophrenia. A controlled trial of a behavioral intervention with families to reduce relapse. British Journal of Psychiatry, 153: 532-542.
Tarrier, N., Barrowclough, C., Vaughn, C., Samrah, J., Porceddu, K, Watts, S., & Freeman, H. (1989) The community management of schizophrenia. A two-year follow-up of a behavioral intervention with families. British Journal of Psychiatry, 154: 625-628.
Thoits, P.A. (1982) Conceptual, methodological, and theoretical problems in studying social support as a buffer against life stress. Journal of Health and Social Behavior, 23: 145-159.
Tomb, D.A. (1995) Psychiatry (5th Ed.). Williams & Wilkins. Baltimore.
Vaughn, C.E., & Leff , J.P. (1976) The Influence of family and social factors on the course of psychiatric illness. British Journal of Psychiatry, 129: 125-137.
Wong, F.K. (1991) The Study of Chronic Strains, Coping and Mental Health of Caregivers of the Mentally Ill. Unpublished MSW Thesis. Hong Kong: The Chinese University of Hong Kong.
Wu, A. C. C. (1995) Cross-cultural, cross-national study of family care-burden imposed by the mentally ill. Chinese Journal of Mental Health, 1: 36-52.
*Stephen Yu-kit Sun, BSW, MSW, Lecturer, Division of Social Studies, City University of Hong Kong<
Siu-kau CHEUNG ,B.Soc.Sc., Adv.Dip.SW (Mental Health), M.Soc.Sc., Ph.D. ,Principal Lecturer, Division of Social Studies, City University of Hong Kong.
* Correspondence: Mr. Stephen Sun, Lecturer, Division of Social Studies, City University of Hong Kong, Tat Chee Avenue, Kowloon Tong, Hong Kong.
1These organizations include New Life Psychiatric Rehabilitation Association, Richmond Fellowship (Hong Kong), and Steward Company. The two hospitals were the United Christian Hospital and Prince of Wales Hospital.