Hong Kong J Psychiatry 2000;10(2):2-7
ORIGINAL ARTICLE
Psychosocial risk factors for Alzheimer's disease
YL He, XK Zhang, MY Zhang
ABSTRACT
This study aims to explore the relationship between psychosocial factors and risk for Alzheimer’s disease and to identify specific psychosocial risk factors from hundreds of potential factors among the Chinese population. A community-based prospective cohort study of dementia in the elderly population performed in Shanghai enrolled 6634 patients older than 55 years from Jing An District by an age-stratified cluster method. Patients were screened by the Mini-Mental State Examination and followed up for 10 years with assessment at 5-yearly intervals. The data reported here identify some psychosocial factors for Alzheimer’s disease from 5- and 10-year follow-up studies. 5055, 3024, and 1203 people completed the base line survey and 5- and 10-year follow-up studies, respectively. The psychosocial risk factors found in both follow-up studies were low educational level, low cognitive function, low occupational status, lack of social interaction and leisure activities, and poor well being. Mini-Mental State Examination score and Activities of Daily Living score had a predictive effect on the onset of Alzheimer’s disease. The conclusion generated from the study was that psychosocial risk factors did impact on the onset and development of Alzheimer’s disease. The emergence of some intervention- susceptible risk factors such as educational level and involvement in leisure activities provides the basis for future intervention study.
Key words: Alzheimer’s Disease; Dementia; Elderly; Psychosocial Risk Factor; Relative Risk
INTRODUCTION
Geriatric mental health problems are gradually emerging since the proportion of elderly people among the general population is continually increasing. Dementia, especially Alzheimer’s disease (AD), is one of the most common and severe mental health problems to afflict elderly people. A community-based study from Shanghai showed that the prevalence of dementia was approximately 4 to 5% for people aged more than 65 years, with nearly two-thirds of them suffering from AD.1 Dementia is now the fourth most common cause of death, after coronary heart disease, cerebral vascular disease, and malignant tumour.
Although pathological features of AD were described 100 years ago, the aetiology of AD remains unclear. Therefore, the exploration of risk factors for AD is an important research question.
During the past decade, research for risk factors for AD focused on molecular genetics.2-6 The amyloid precursor protein (APP) genes of chromosome 21, the presenilin-1 gene of chromosome 14, and the presenilin-2 gene of chromosome 1 have been identified. Mutation or polymorphism of alleles in these genes was associated with the occurrence of AD, especially the early-onset type of familial AD. For sporadic late-onset AD, which accounts for 90% of all AD, it was found that the Apo E4 allele was involved. For example, in Shanghai, gene frequency of Apo E4 was 0.105 among healthy elderly people.7 The frequency is lower than that for western countries but similar to the frequency in other Asian countries. On the other hand, Apo E4 gene frequency among people with late- onset AD was 0.262, 2.5-fold that of healthy elderly people. This higher relative risk (RR) is similar to reports from both western and Asian countries.
Although biological risk factors for AD have been intensely studied, factors such as family history and Apo E4 do not completely explain the occurrence of AD. No definite or specific biological causes have been found among most sporadic cases. The population attributable risk proportion (PARP) of biological risk factors is not high. However, there are risk factors other than biological factors for AD such as psychosocial considerations. While it is difficult to intervene in most of the biological factors, more attention could be directed to the study of psychosocial risk factors for AD.
More than 30 psychosocial risk factors have been found for the onset of dementia. They include education, occupation and socio-economic status, life style and life events, and mental health. But there is also controversy and most of the previous studies were hospital-based, retrospective case-control studies, with only single or few factors analysed.
One of the largest studies was performed by the European Studies of Dementia (EURODEM ) group in 11 countries and regions (seven hospital-based and four community-based).8 This case-control study included 1,397 patients with AD and 1,756 age- and gender-matched controls. The results suggested that the main risk factors for AD were positive family history of dementia, history of psychosis in first degree relatives, family history of Parkinson’s disease, exposure to a harmful environment, aluminium intake, left handedness or ambidexterity, poor economic status, lack of interesting life events, and occurrence of major negative life events. Other possible risk factors for AD were female gender, previous head injury, low educational level, allergy, meningitis, epilepsy, and alcohol intake. Risk factors such as thyroid disease, depression, maternal age at birth, viral infections, visual and hearing disorders, hypoactivity, and low socio-economic status remain to be confirmed.
Little research related to psychosocial risk factors has been performed in China. To our knowledge, the only study that has been reported was the retrospective case-control study by Shen et al.9 Lack of interest and occurrence of major negative life events wer e found to have a significant relationship with AD. The purpose of our study was to explore the relationship between psychosocial factors and risk for AD. We have tried to identify specific psychosocial risk factors for AD that may respond to intervention. In order to obtain more informative data, the research was designed as a community-based prospective cohort study and was a continuation of the Shanghai epidemiological survey of dementia and AD.1,10 The data reported here consist of the results of the effect of psychosocial factors on AD at 5 and 10 years.
METHODS
STUDY DESIGN
Jing An district is one of 15 districts in the City of Shanghai. At the time of the survey, the district had a population of approximately half a million, with 21% of the population aged 55 years or older and 8% aged 65 years or older. A probability sample of multifamily neighbourhood groups was drawn up by means of a variation of the random single-stage cluster sampling method.11-13 In a randomly selected neighbourhood, all households were targeted for interviews if they included a family member in the age criterion.
A two-stage procedure was administered to identify dementia and AD. In Phase I, a survey of the sample population was performed to identify people with cognitive changes suggestive of dementia. In Phase II, a detailed clinical and cognitive evaluation of the people identified in Phase I, together with a 5% sample of the remaining population, was performed to identify persons with dementia. Details of the sampling methodology are described in a previous report.14
The first survey for baseline data was performed in 1987. A similar procedure was repeated in 1992 and 1997 for the same sample population. All interviews were completed during home visits, both for the respondents and their key relatives, by trained interviewers who were either psychiatrists or psychiatric nurses.
SUBJECTS
From a probability sample of 6634 people (aged 55 years and older) in the baseline survey, a total of 5271 (79.5%) completed the interview for screening for dementia. 96% of the respondents (5055 people) were able to complete the Chinese version of the Mini-Mental State Examination (CMMSE). 159 people with dementia were identified, including 98 patients with AD.
People who were free from dementia in the baseline survey were included in both the 5- and 10-year follow-up surveys (1992 and 1997, respectively) by a similar two-stage procedure.15 Among the 3024 patients re-surveyed in 1992, 141 new patients with dementia, including 92 patients with AD, were identified. In 1997, there were 124 new patients with dementia including 81 patients with AD, identified from 1203 people who completed the interview. The main reasons for loss to follow-up were death and moving away from the sampling area.
INSTRUMENTS
Diagnoses were based upon the following criteria:
(1) the culturally adapted Chinese version of the Folstein Mini-Mental State Examination (MMSE)16 and the Blessed Information-Memory-Concentration test17,18
(2) neuropsychological tests
(3) a psychiatric interview and physical and neurological examination by research psychiatrists
(4) a dementia history questionnaire
(5) the Pfeffer Functional Activities Questionnaire (FAQ) and the Activities of Daily Living (ADL) scale.
The Diagnostic and Statistical Manual for Mental Disorders (DSM)-III criteria were used to diagnose dementia.19 Alzheimer’s disease was diagnosed on the basis of the National Institute of Neurological and Communicative Disorders and Stroke- Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) criteria.20
Most patients identified from the clinical evaluation were further verified by computerised tomography (CT) scan and laboratory tests recommended by the Alzheimer’s Disease Research Center (ADRC) at the University of California, San Diego, USA.
A structured questionnaire consisting of approximately 100 items addressing psychosocial factors, including living patterns, health habits, leisure time activities and attitudes, social network, and family relationships, which may relate to dementia (according to previous empirical studies) was completed by both the respondents and key family members during the baseline survey in 1987.21
STATISTICAL ANALYSIS
In addition to standard descriptive statistics, logistic regression analysis was used to determine whether these psychosocial factors were independent risk factors for dementia. The RR, 95% confidence interval (95% CI) and population attributable risk proportion were calculated for exposure factors. Sex and age were controlled in the analysis. The data analysis was generated using the Statistical Package for Social Science (SPSS).
RESULTS
INCIDENCE AND DEMOGRAPHY OF ALZHEIMER’S DISEASE
The sex, age, and education distributions of incident demented patients are shown in Table 1. For patients with newly developed AD, males accounted for only 33.7% and 23.5%, respectively, in the two follow-up studies. Alzheim- er’s disease accounted for about two-thirds of all new dementia patients. The proportions of new AD was higher in females than in males in both studies and the proportions increased with age and decreased with higher educational levels.
The weighted annual incident rate of AD for people aged 65 years and older were 0.89% and 0.95%, respectively, in the 5- and 10-year follow-up studies, according to the equations: i=[1-(1-i5/100)1/5] x 100% and i=[1-(1-i10)1/10] x100% used for the 5- and 10-year calculations, respectively. ‘i’ represents the annual incidence, ‘i ’ is the 5-year incidence, and ‘i’ represents the 10-year incidence.
PSYCHOSOCIAL RISK FACTORS FOR ALZHEIMER’S DISEASE IDENTIFIED
The operational definition for more than 70 items of psychosocial factors were applied to exposure and non-exposure conditions for patients with AD and healthy elderly people. These included blue collar occupation versus non-blue collar (including white collar and no formal job) and no work during the previous year versus employment. By way of logistic regression, the RR and 95% CI of the psychosocial factors and the PARP of the risk factors were calculated.
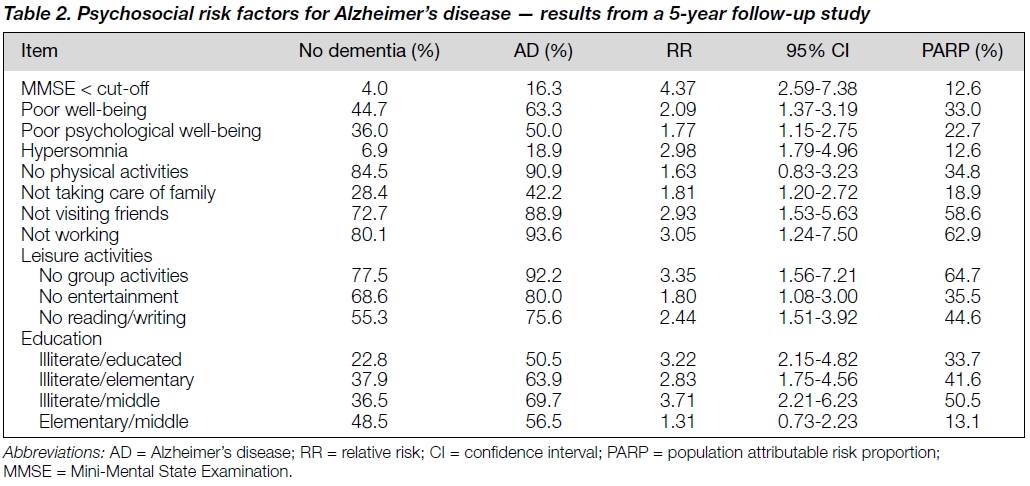
FOLLOW-UP RESULTS AT 5 YEARS
All the items listed in Table 2 showed a relative risk greater than 1. Premorbid cognitive function deficit (low MMSE) showed a significant impact on the onset of AD with the highest relative risk of all the psychosocial factors. Illiterate patients and those not involved in group activities had a more than three-fold higher risk for AD than educated patients involved in group activities. Unemployment, too much sleep, not visiting friends, not reading, and self-rated poor well-being resulted in a RR greater than 2 compared with employment, limited sleep, visiting friends, reading, and positive well-being.
The PARP represents the extent to which the patients in the target population could be contributing to specific factors. For example, no group activity at leisure time showed a PARP of 64.7% (Table 2), indicating that 64.7% of all AD in the group aged 60 years or more living in the community could be attributed to not participating in group activities. In other words, if people participated in group activities, AD onset may have been prevented for 64.7% of people. The other factors with a PARP of greater than 50% were unemployment and illiteracy compared with middle school education. No reading, no education compared with good education, no entertainment, no physical activities, and poor well-being had a PARP score of more than 30%.
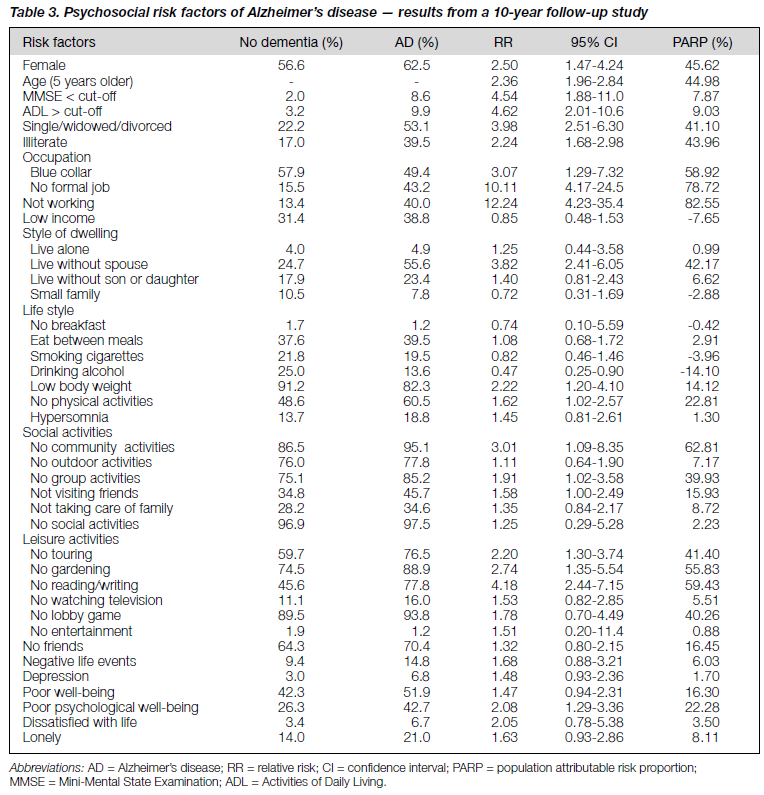
FOLLOW-UP RESULTS AT 10 YEARS
In the 10-year follow-up study, additional variables related to possible psychosocial factors such as living status and life style were analysed together with the previously analysed variables. Table 3 shows that female gender, increasing age, MMSE less than the cut-off point and ADL greater than the cut-off point were again verified to have a strong relationship to AD. 15 variables had a 95% CI of RR greater than 1 at its lower threshold. These were unemployment, not reading and writing, being single, widowed or divorced, not dwelling with spouse, blue collar occupation, no involvement in community activities, no gardening, low educational level, low body weight, not touring, poor psychological well-being, no involvement in group activities, not visiting friends, and no physical activities. The RR of having AD in those with lower educational levels was 2.24-fold those with higher education — the lower the educational level, the higher the risk of AD. Compared with the RR for those with blue collar jobs, people with no formal job had a much higher RR. In dwelling styles, it seemed that only those living without a spouse had a higher risk for AD.
Psychosocial factors related to not working, not having a formal job and being a blue-collar worker had the highest population attributable risk proportion. Not pursuing social and leisure activities such as community/group activities, reading and writing, gardening, touring, physical activities, and visiting friends also had a higher PARP.
Interestingly, alcohol drinking was the only factor with a RR of 0.47 (0.25-0.90) and negative PARP. Further study is needed to demonstrate whether alcohol, particularly yellow wine (a favourite rice wine for Shanghai residents), could offer protection from AD.
DISCUSSION
This study was designed as a community-based prospective cohort study with an incidence survey and both 5- and 10- year follow-up data. A comprehensive range of psychological factors covering marital status, educational level, occupation, working status, income, living status, life style, social and leisure activity, physical and mental well being, and other psychological and social situations were investigated. The model used in the study was the exposure or non-exposure to specific psychosocial factors. AD or no AD was identified for both the exposure or no exposure groups. The relationship between the onset of AD and exposure to the specific factors were described by the calculation of RR and the importance to the specific population was explained by PARP. Compared with case-control or cross-sectional studies, prospective cohort studies are more representative and the data generated are more reliable and convincing. In cross-sectional studies, it is often hard to determine if the positive psychosocial factors found are risk factors for AD or the consequences of AD. In this study, all possible psychosocial factors were investigated in the baseline survey, which was 5 or 10 years prior to the onset of dementia. The positively identified factors therefore are likely to be related to the cause, rather than the result, of dementia.
Another key feature of this study is the screening and definition of the variables. There were approximately 100 factors considered in the study. More than 70 items were screened and concluded as exposure situations according to previous reports. Exposure or no exposure were defined by a traditional method of psychiatric epidemiology, sociology, and preventive medicine in order to make the results comparable.
As reported in the literature, age and gender were again verified as significant risk factors for AD.1,9,10,22-27 The incidence of AD among people aged 65 years and older living in a community was 0.95% — 0.46% for male patients and 1.33% for females in the 10-year survey, a significant difference (Chi-square = 12.27, p < 0.001). The RR of AD for females was 2.5-fold that for males. The RR of having AD increases 2.36-fold every 5 years after the age of 55 years. MMSE and ADL were found to be effective not only for screening out cognitive and functional impair ments, but also for predicting AD.
Psychosocial risk factors identified from the 5- and 10- year follow-up studies were similar and consistent with reports from other countries.8,22-25 The concordant findings of psycho- social risk factors between the two surveys were low educational levels, particularly illiteracy, low basic cognitive function, low basic occupational status or no formal job, lack of social interaction such as visiting and group activity, lack of leisure activity such as reading, and poor feelings of well-being.
The potential connection between biological factors with psychosocial factors was interesting. Experiments show that when ageing mice are exposed to a stimuli-enriched environment, the cerebral cortex thickens and the weight and number of dendrites increase.28 Their general cognitive performance is better than that of mice exposed to a routine environment. Cognitive function reserves of elderly people could be improved by stimulus training.29 Adult education and intellectual activities can also help to compensate for the cognitive decline of normal ageing and could delay the onset of clinical symptoms of AD. Some authors thought that early education could directly increase the number of synapses or synaptic reserve and growth; lack of education and poverty of intellectual stimulus might result in poor development of synapses.27 It has been speculated that cognitive change associated with AD could imply cerebral cortex density changes. Therefore, reduced neural reserves would be associated with earlier and more severe expression of AD.27
We still believe that biological factors are the major cause of AD although the results of studies of psychosocial risk factors are important. In other words, psychosocial risk factors add fuel to the flames of biological factors. There are still uncertainties about the relationship between psychosocial risk factors and AD, as well as the known biological risk factors. Many psycho-social-environment factors remain unexplored and some of the results remain contradictory. In addition, the PARP of some risk factors for AD are not particularly high. Further study based on these results will be important for exploring the potentials for preventive intervention — a novel approach that requires further consideration.
REFERENCES
- Zhang MY, Katzman R, Salmon D, et al. The prevalence of dementia and Alzheimer’s disease in Shanghai, China: impact of age, gender, and education. Ann Neurol 1990;27:428-437.
- Bergener M,Finkel S. Treating alzheimer’s and other dementias. New York: Springer Publishing Company Inc; 1995.
- Levy-Lahad E, Wijsman EM, Nemens E, et al. A familial alzheimer’s disease locus on chromosome 1. Science 1995; 269: 970-972.
- Brousseu T, Legrain S, Berr C, et al. Comfirmation of the Apo E4 allele of the apolipoprotein E gene as a risk factor for late-onset Alzheimer’s disease. Neurology 1994;44:342-344.
- Goate A, Ckantier-Harlin M, Mullan M, et al. Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature 1991;349:704 -706.
- Higuchi S, Muramatsu T, Malsushita HA, et al. Presenilin-1 polymorphism and Alzheimer’s disease. Lancet 1996;347:1186.
- Jiang S, Feng GQ, Wu XD, et al. The analysis for the correlation of Alzheimer’s disease and Apo E4 [article in Chinese]. Chin J Psychiatry 1996;29:15-18.
- Van Duijn CM, Stunen T, Hofman A, et al. Risk factors for Alzheimer’s disease: overview of the EURODEM collaborative re-analysis of case control studies. Int J Epidemiol 1991;20 (Suppl.): 4-71.
- Shen YC, Li YT, Li R, et al. A case control study for risk factors of Alzheimer’s disease [article in Chinese]. Chin J Neurol Psychiatry 1992;25:284-287.
- Zhang MY, Katzman R, Yu E, et al. A preliminary analysis of incidence of dementia in Shanghai, China. Psychiatry Clin Neurosci 1998;52 (Suppl.):291-294.
- Levy P, Yu ESH, Liu WT, et al. Sample design of the Shanghai elderly survey: a variation of single stage cluster sampling. Int J Epidemiol 1989;17:931-933.
- Yu ESH, Liu WT, Levy P, et al. Cognitive impairment among the elderly in Shanghai, China. J Gerontol 1989;44 (Suppl.):97-106.
- 13. Qu GY, Ren FM, Yao CD, et al. Data collection in Shanghai survey of the Paper presented at the Asia-USA Conference on Social Services and Aging Policy. 1988 August 7-11. Pensacola, Florida, USA.
- Zhang MY, Qu GY, William Liu, et al. The study design and implement of the Shanghai (Jing An District) elderly survey [article in Chinese]. Arch Psychiatry 1989;7:101-104.
- 15. Zhang MY, Katzman R, Chen PJ, et al. The incidence study of dementia and Alzheimer’s disease: in relation to sex, age and education [article in Chinese]. Chin J Psychiatry 1998;31:195-198.
- 16. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinicians. J Psychiatr Res 1975;12:189-198.
- Blessed G, Tomlinson E, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral gray matter of elderly subjects. Br J Psychiatry 1968; 114:797-811.
- Jin H, Salmon D, Katzman R, et al. Cross-cultural studies of demen- tia: use of a Chinese version of the Blessed-Roth Information- Memory-Concentration test in a Shanghai dementia survey. Psychol Aging 1989;4:471-479.
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd edition (DSM-III). Washington: APA; 1980.
- McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Groups under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984;34:939-944.
- Zhang MY, Elena Yu, He YL. The instruments for epidemiological survey for dementia and its application [article in Chinese]. Arch Psychiatry 1995;7 (Suppl.):1-25.
- Evans DA, Hebert LE, Beckett LA, et al. Education and other measures of socioeconomic status and risk of incident Alzheimer’s disease in a defined population of older persons. Arch Neurol 1997;54:1399-1405.
- Callanhan CN, Hall KS, Hui SL, et al. Relationship of age, education, and occupation with dementia among a community- based sample of African Americans. Arch Neurol 1996;53: 134-140.
- Stern Y, Gurland B, Tatemichi TK, et al. Influence of education and occupation on the incidence of Alzheimer’s disease. J Am Med Assoc 1994;271:1004-1010.
- Fabrigoule C, Letenneur L, Dartigues JF, et al. Social and leisure activities and risk of dementia: a prospective longitudinal study. J Am Geriatr Soc 1995;43:485-490.
- Zhang XK, He YL, Zhang MY, et al. Exploring the psychosocial risk factors for dementia and Alzheimer’s disease in elderly [article in Chinese]. Arch Psychiatry 1998;10 (Suppl.):2-12.
- Katzman R. Education and the prevalence of dementia and Alzheimer’s disease. Neurology 1993;43:13-20.
- Swaab DF. Brain aging and Alzheimer’s disease. “Wear and tear” versus “use it or lose it”. Neurobiol Aging 1991;12:317-324.
- Yesavagev JA. Non-pharmacological treatments for memory loss with normal aging. Am J Psychiatry 1985;142:600-605.
Dr YL He, MD, Associate Professor, Shanghai Mental Health Center, Department of Psychiatry, Shanghai Second Medical University, Shanghai, China.
Dr XK Zhang, MD, Shanghai Mental Health Center, Department of Psychiatry, Shanghai Second Medical University, Shanghai, China.
Dr MY Zhang, MD, Professor, Shanghai Mental Health Center, Department of Psychiatry, Shanghai Second Medical University, Shanghai, China.
Address for correspondence: Dr Yanling He
Shanghai Mental Health Center 600 Wan Ping Nan Lu
Shanghai 200030, China.
E-mail address: heyl@public9.sta.net.cn