Hong Kong J Psychiatry 2002;12(4):6-13
ORIGINAL ARTICLE
RMK Ng
Acknowledgement: Thanks to my research assistant, Mr Paul Kong, for his hard work in collecting the data.
Dr Roger MK Ng, MBChB, MRCPsych (UK), FHKAM (Psych), Senior Medical Officer, Kowloon Hospital, Kowloon, Hong Kong, China.
Address for correspondence: Dr Roger MK Ng, Senior Medical Officer, Kowloon Hospital, Kowloon, Hong Kong, China. E-mail: rmkng@netvigator.com
Submitted: 24 June 2002; Accepted: 24 August 2002
Abstract
Objective: The continuous performance test reveals deficits in patients with schizophrenia compared with normal subjects. The 3-7 continuous performance test and degraded continuous performance test are ‘high-load’ versions that appear to indicate vulnerability to schizophrenia in high-risk individuals independently of the psychotic state (degraded continuous performance test) and in association with acute episodes (3-7 continuous performance test). This study evaluated the degraded and 3-7 continuous performance tests, and their correlation with psychosis-proneness as measured by Chinese versions of the Oxford-Liverpool Inventory of Feelings and Experiences and the Schizotypal Personality Scale, in Hong Kong Chinese subjects.
Methods: The 3-7 and degraded continuous performance test versions were administered to 25 schizophrenic patients and 25 age- and sex-matched controls. In the second part of the study, 85 university students (aged 17 to 21 years) without a psychiatric history were tested using the 2 versions of the continuous performance test and the Oxford-Liverpool Inventory of Feelings and Experiences, and the Schizotypal Personality Scale.
Results: Schizophrenic patients performed significantly worse than normal subjects in degraded and 3-7 continuous performance tests (p < 0.05, both versions). Forty five students completed the psychosis-proneness and continuous performance test evaluations. In the student sample, significant gender differences were evident for the Oxford-Liverpool Inventory of Feelings and Experiences items (p < 0.0001 to p = 0.002) and the Schizotypal Personality Scale (p = 0.001). Chinese versions of the Oxford-Liverpool Inventory of Feelings and Experiences and the Schizotypal Personality Scale proved to be valid and reliable. There was a modest, significant correlation between degraded continuous performance test performance and cognitive disorganisation subscales of the Oxford-Liverpool Inventory of Feelings and Experiences and the Schizotypal Personality Scale (p < 0.05), but no similar effect for the 3-7 continuous performance test.
Conclusion: There are modest, significant inverse correlations between psychosis-proneness and degraded continuous performance test performance, suggesting that early perceptual deficit may account for non-clinical, mild schizotypal symptoms in the normal population.
Key words: Personality tests, Psychiatric status rating scales, Schizophrenia
Introduction
Chapman believed that the initial prodrome of psychosis consists of disturbances of selective attention, intermittent disturbances of perception (abnormalities of brightness, colour, size and shape, and inability to see the overall Gestalt of the image), and sudden disruption in attention and thought, as well as disturbances in speech and motor function.1 Anscombe argued that the schizophrenic ex- perience was an inability to sustain an intentional focus to attention.2 Attention was captured by incidental details in the environment, leading to a false sense of significance. These findings suggest that vigilance/attentional and per- ceptual deficits may play an important role in the genesis of psychotic symptoms.
The continuous performance test (CPT) is a well- established cognitive task measuring vigilance/sustained attention. The original version of the CPT was developed by Rosvold et al.3 The various versions of CPT typically involve tachistoscopic presentations (40 to 200 ms) of a quasi-random series of letter or numeral stimuli at a rapid, fixed rate for 5 to 15 minutes, with instructions to respond to a predesignated letter or number or sequence of letters or numbers each time it appears. Some versions aim to increase the processing load and place particular burden on certain aspects of information processing. ‘High-load’ versions of the CPT include degraded CPT, which uses blurred visual stimuli to burden the initial visual encoding and analysis processes, and ‘3-7’ CPT, which places increased demand on active working memory. 4
Multiple studies have found that chronic schizophrenic patients have lower hit rates and higher false-alarm rates in CPT compared with normal and psychiatric controls.5 CPT performance has also been demonstrated to be impaired in remitted schizophrenic patients.6 In a cross-sectional study comparing acutely psychotic schizophrenic patients and relatively remitted schizophrenic patients, Asarnow and MacCrimmon demonstrated lower hit rates and higher false- alarm rates in both groups of schizophrenic patients than in normal controls. 7 Steinhauer et al showed that stabilised schizophrenic outpatients have a lower sensitivity index in the degraded stimulus CPT version compared with normal controls.8
The CPT performances of high-risk subjects (siblings and children of schizophrenic patients) have also been investigated. In general, if the CPT task is relatively easy, there tends to be little difference in performance.5 However, high-risk subjects show poorer performances when the CPT is made more difficult by the addition of a short-term memory load9 or by visually degrading the stimuli.10 If the version is not at least moderately difficult, this difference may not be obvious, as demonstrated in the lack of difference between high-risk children and children of normal parents.11 These findings suggest that versions of CPT that are moderately difficult indicate vulnerability to schizophrenia.
The boundaries of psychosis are not clear and schizo- phrenia may represent only the extreme end of a continuum that spans from mild to severe disease, as suggested by Bentall et al.12 Surveys have demonstrated that mild anomalies in experience, thinking, and belief that have a resemblance to psychotic symptoms occur in a substantial proportion of the normal population (approximately 15% to 20%), as well as people with frank psychotic disorder.13, 14 The milder expressions of the disease continuum may include individuals who are unmedicated, fully functioning, and have no psychotic symptoms.
High schizotypic subjects have poorer performance on the CPT, adding support to its role as an indicator of vulnerability.15 People with high scores in psychosis- proneness measures have also been found in longitudinal studies to have an increased risk of psychosis.13 Further studies have consistently supported a poorer performance in CPT with high processing demand by SPD subjects compared with normal subjects16 or those with other personality disorders.17,18
So far, there has been no direct study examining the performance of the 3-7 CPT in schizotypal subjects.
Objectives
This study aimed to test the following hypotheses:
- the Oxford-Liverpool Inventory of Feelings and Experiences (O-LIFE)19 and Schizotypal Personality Scale (STA)20 are both valid and reliable instruments for the measurement of psychosis-proneness in Chinese populations
- degraded CPT and 3-7 CPT are reliable and valid instru- ments for the measurement of vigilance/sustained attention
- performance on degraded CPT, but not 3-7 CPT, correlates negatively with the level of psychosis-proneness as measured by the O-LIFE and STA.
Methods
Validation of Degraded and 3-7 Continuous Performance Tests
The first part of the study included 25 hospital staff matched for age and sex with 25 schizophrenic patients (11 male and 14 female). Baseline sociodemographic data, including years of education, were also collected. Psychiatric data included duration of illness and medication use. Matching of age, sex, and years of education is required because data in the Chinese population has shown that males had a higher hit rate and overall sensitivity than females, while older age was associated with decreasing hit rate and overall sensitivity.21
Schizophrenic patients were identified according to DSM-IV criteria. Comorbid diagnoses of substance abuse, mental retardation, and organic psychotic disorders were excluded. Schizophrenic patients who were actively psych- otic were also excluded. Recruiting of hospital staff involved use of a screening questionnaire with exclusion criteria for history of psychiatric problems, family history of psychiatric disorders, and current use of psychotropic medication or illicit drugs.
Separate samples of schizophrenic patients (n = 11) and normal subjects (n = 11) with similar inclusion and exclusion criteria were used for test-retest reliability purposes, except that the subjects were not matched for age and sex. The schizophrenic patients were in a stable mental state and received no change in medication during the 1-month follow- up period.
Patients and controls were administered the degraded and 3-7 versions of CPT.4 Both groups were screened for visual acuity before the test was conducted. The tests were administered under conditions specified by the University of California (UCLA) group in terms of computer monitor type, level of illumination of the computer screen, and the laboratory environment, to ensure comparability with the work of the latter group.4 All subjects were tested by an experienced research assistant, who was not aware of the study hypothesis. The author supervised 30% of the sessions, selected at random, to ensure proper execution of the study procedures. The order in which the 2 versions of CPT were administered was determined by tossing a coin.
Continuous Performance Test Protocol
Briefly, in a conventional CPT, the subject views a series of stimuli on a screen and is instructed to press a response button whenever a target stimulus appears. In the 3-7 version, the target is a sequence (a ‘3’ followed by a ‘7’). For a degraded version, the target is a single stimulus (a blurred ‘0’). The stimuli are presented briefly, for less than one- tenth of a second, and follow at a rate of about 1 per second. The test yields a measure of ‘sensitivity’, which is the ability to discriminate signal (targets) from noise (non-targets). The degraded version imposes a burden for initial perceptual discrimination, while the 3-7 version involves active, working memory (the mental representation of 1 stimulus needs to be maintained long enough to compare with a subsequent stimulus, and then the representation needs to be updated).
Psychosis-proneness Scales: Validation and Relationship to Continuous Performance Test
The second part of the study involved recruitment of 115 university students aged 17 to 21 years, and collection of data on their social demographics and personal and family history of psychiatric illness. The research assistant approached university students in the campus and ex- plained the purpose of the study before informed consent was obtained. Only subjects without a personal history of psychiatric illness were recruited to maintain the non- clinical and unmedicated nature of this sample. The CPT was administered in laboratory conditions as specified above.
Psychosis-proneness was measured using 2 scales: the Chinese version of the O-LIFE, containing 4 psychosis- proneness scales (unusual experiences, cognitive disorganis- ation, introvertive anhedonia, and impulsive non-conformity), and the Chinese version of the STA. The O-LIFE comprises forced-choice yes-no responses to 30 questions in unusual experiences, 24 questions in cognitive disorganisation, 27 questions in introvertive anhedonia, and 23 questions in impulsive non-conformity, resulting in a total of 104 questions. The total score can therefore range from 0 to 104.
The O-LIFE has shown a high internal consistency and high 3-month test-retest reliabilities,19 with a significant gender effect.19,20 The STA scale measures schizotypal experiences in normal subjects and comprises 36 questions. It has also been found to have high internal consistency, and high test-retest reliability.20 The STA is used to supple- ment the O-LIFE, as the latter scale has limited coverage of schizotypal experiences 19
A psychology graduate translated the inventory into Chinese and the author then back-translated it into English. Five experienced mental health professionals (2 psych- iarists, 1 psychologist and 2 occupational therapists) were invited to read the Chinese versions of the O-LIFE and STA. The professionals were asked to give a yes-no response to the question: “Is this question relevant to measuring the psychosis-proneness in a normal population?” against each of the 140 questions of the O-LIFE and STA.
Data Analysis
Three major indexes were used to analyse the performance of the degraded and 3-7 CPT versions:
- hits, the proportion of correct responses to target trials/correct detections
- false alarms, the proportion of responses to catch trials/commission errors
- sensitivity, a measure of discriminability, calculated from hits and false alarms.22
The differences in the mean levels of CPT performance data of the normal and schizophrenic patients were examined with 2-tailed Student’s t tests. Similar t-testing of statistical significance was used for comparison of patients treated with typical and atypical antipsychotics, the effect of treatment with anticholinergic agents, and other continuous socio- demographic data (age and years of education).The p value for statistical significance for all t tests was set at 0.05. For multiple comparisons, Bonferroni’s correction was applied.
For test-retest reliabilities of the psychosis-proneness scales and the CPT performances, Pearson product moment correlations were used to examine the associations between results of the 2 test periods. Pearson product moment was also used to explore the associations between the CPT performances and the psychosis-proneness subscales.
Results
Validation of Degraded and 3-7 Continuous Performance Tests
Test-retest reliability
The mean age of the schizophrenic patients was 45.6 years, compared with 35.3 years for the normal subjects (p < 0.0001). The mean duration of education was also sig- nificantly different between the normal subjects (15.6 years) and the schizophrenic patients (10.7 years) [p < 0.0001]. The schizophrenic patients were stable throughout the study period, as indicated by no change in medication or stable maintenance in an intensive rehabilitation ward.
The degraded and 3-7 CPT versions were validated in separate samples of normal subjects (n = 11) and schizo- phrenic patients (n = 11). The 1-month test-retest reliabilities of degraded CPT in normal subjects were 0.826 for overall hit rate (p < 0.0001), 0.723 for overall false-alarm rate (p < 0.001), and 0.786 for overall sensitivity (p < 0.0001). For the 3-7 CPT, the test-retest reliabilities for overall hit rate, overall false-alarm rate, and overall sensitivity in normal individuals were all non-significant. This might have been because of the ceiling effect of the performance of the normal individuals. (K Nuechterlein, personal communication).
For the schizophrenic patients, the 1-month test-retest reliabilities of the 3-7 CPT were 0.971 for overall hit rate (p < 0.0001), 0.823 for overall alarm rate (p < 0.001), and 0.984 for overall sensitivity (p < 0.0001). The 1-month test-retest reliabilities of the degraded CPT for the schizo- phrenic patients were 0.918 for overall hit rate (p < 0.0001), 0.886 for overall alarm rate (p < 0.001), and 0.992 for over- all sensitivity (p < 0.0001). The results suggest that the degraded, but not the 3-7 version of CPT, is suitable for repeated measurement in normal individuals. However, both versions are suitable for repeated measurement in patients with schizophrenia.
Continuous performance test performance by normal subjects and schizophrenic patients
Both the schizophrenic group and the normal group comprised 10 males and 15 females. The mean age of the normal group was 35.5 years and that of the schizophrenic patients was 35.3 years (t test, p = 0.678). There was also no significant difference in years of education between the groups, with the normal subjects receiving an average of 11.2 years and the schizophrenic patients 10.3 years (t test, p = 0.528). Fifteen patients were receiving treatment with atypical antipsychotics, and 10 patients were receiving conventional antipsychotics, the latter at a mean dose of 485 mg chlorpromazine equivalents. Thirteen patients also received adjunctive anticholinergic treatment, and 2 patients were also receiving valproate.
There was no significant difference in 3-7 and degraded CPT performance between those receiving atypical and conventional antipsychotics or between those receiving and not receiving anticholinergic agents. There was no significant correlation between the dose of anticholinergic agents or conventional antipsychotics and CPT performance in those receiving conventional antipsychotics.
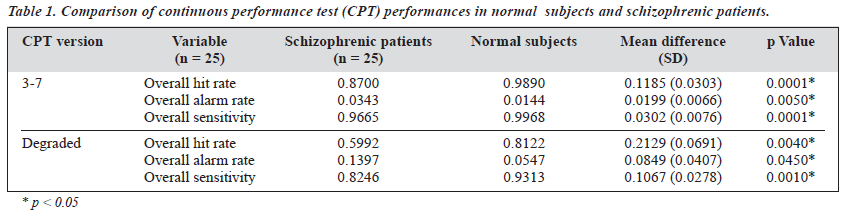
Schizophrenic patients performed significantly worse than the normal subjects in both the degraded and 3-7 CPT versions (Table 1). When non-parametric tests (Mann-Whitney U test) were used for comparison, the difference remained statistically significant (p < 0.05 for all comparisons).
Validation of Psychosis-proneness Scales
Of 115 university students recruited, 85 completed both the O-LIFE and the STA in full. The completers comprised 38 males and 47 females, with a mean age of 21.9 years and 22.6 years, respectively (t test, p = 0.455). Twelve of 85 subjects had a family history of psychiatric illness. There were no significant differences in O-LIFE and STA scores between those with and without a family history of psych- iatric illness. In the assessment of the relevance of the Chinese versions of the O-LIFE and STA by health profes- sionals, of the 140 questions, 103 attained 100% agreement by all 5 professionals, 28 attained 100% agreement by 4 profes- sionals, while 10 attained 100% agreement by 3 professionals.
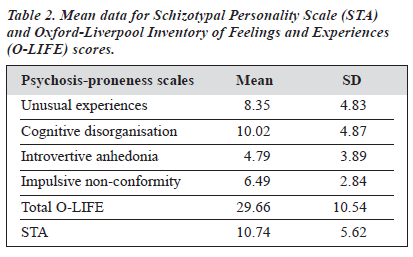
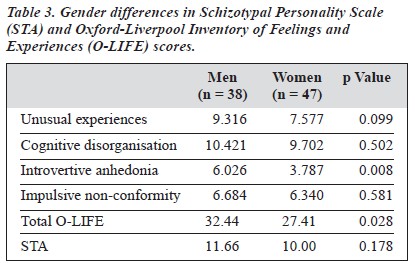
The O-LIFE and STA results are shown in Table 2. There were significant gender differences in the O-LIFE and STA results (Table 3) — females had significantly lower scores in introvertive anhedonia. This result was compatible with the findings of Mason et al,19 and Rawlings and Freeman.23
However, there was no significant difference in impulsive non-conformity, in contrast to the finding of Mason et al,19 but similar to the findings of Rawlings and Freeman.23
Internal consistency
The internal consistency (Cronbach’s alpha) of the Chinese version of O-LIFE in the sample of 85 university students was 0.801 for unusual experiences, 0.841 for cognitive disorganisation, 0.707 for introvertive anhedonia, and 0.70 for impulsive non-conformity.
Compared with the results of Rawlings and Freeman23 (0.88 for unusual experiences, 0.84 for cognitive dis- organisation, 0.70 for introvertive anhedonia, and 0.70 for impulsive non-conformity), the present results showed good agreement. For the Chinese version of the STA, the internal consistency of 0.70 was also compatible with the findings of Claridge and Broks.20
Three-month test-retest reliabilities
The 3-month test-retest reliabilities of a sub-sample (n = 23) were statistically significant for the items of unusual experience (r = 0.774, p < 0.0001), cognitive disorganisation (r = 0.853, p < 0.0001) introvertive anhedonia (r = 0.724, p < 0.0001) impulsive non-conformity (r = 0.607, p = 0.002) total O-LIFE (r = 0.749, p < 0.0001), and STA (r = 0.646, p = 0.001).
Convergent validity
The STA had significant correlations with unusual experience (r = 0.769, p = 0.0001), introvertive anhedonia (r = 0.254, p = 0.019), cognitive disorganisation (r = 0.629, p = 0.0001), impulsive non-conformity (r = 0.323, p = 0.003), and total O-LIFE score (r = 0.823, p = 0.0001).
Relationship Between Psychosis-proneness and Continuous Performance Tests
Of 85 subjects given the O-LIFE and STA tests, 45 completed both the degraded and 3-7 CPT versions. The other 40 subjects did not complete the CPT tests. Some refused the tests (n = 15), and others were noted to have poor motivation during the tests (n = 12) or gave up before completing the tests (n = 13). Only the results for the 45 subjects completing both CPT versions were available for examination of the correlation between CPT performance and psychosis-proneness.
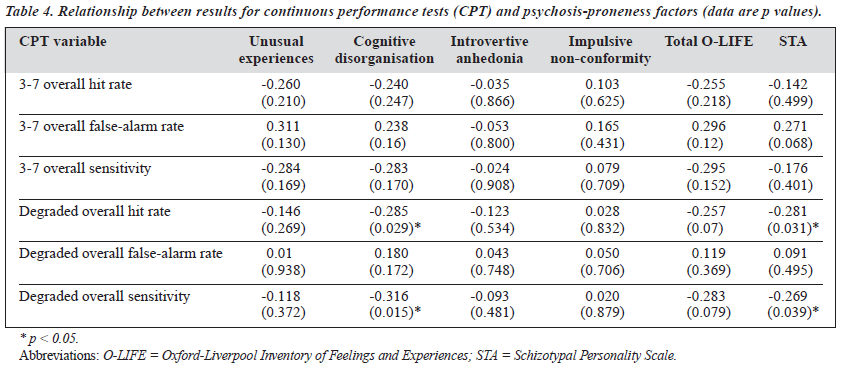
With the p value for significance set at 0.05, there was a statistically significant correlation between degraded CPT performance (overall hit rate and overall sensitivity) and the cognitive disorganisation subscale of the O-LIFE and STA (Table 4). There was little correlation between the 3-7 CPT indexes and psychosis-proneness scores. However, with the p value for significance set at 0.001 (Bonferroni’s correction for multiple comparisons, p < 0.0001), there was no signifi- cant correlation between even degraded CPT performance and psychosis-proneness scores.
When the subjects were split into 2 groups corresponding to the 25th percentile (n = 11) and the 75th percentile (n = 12), respectively, of the O-LIFE results, the 2 groups were found to have only a marginally significant difference in degraded-stimulus (DS)-overall hit rate (Mann-Whitney test, p = 0.098). When the subjects were split into 2 groups corresponding to the 25th percentile (n = 12) and the 75th percentile (n = 12) of the STA results, respectively, the 2 groups were found to be significantly different in both the DS-overall hit rate (Mann-Whitney test, p = 0.03), and DS-overall sensitivity (Mann-Whitney test, p = 0.019).
Discussion
Continuous Performance Tests for Hong Kong Chinese People
This was the first study that attempted to validate 2 versions of CPT, namely the 3-7 and degraded CPT, in the Hong Kong Chinese population. Both versions appear to be reliable for repeated measurement in schizophrenic patients. Furthermore, schizophrenic patients performed worse than age- and sex-matched normal subjects in both versions, similar to the results of Nuechterlein et al.4 The poor performance in degraded CPT supports the presence of deficits of sustained attention and early perception in schizophrenic patients. There is also an additional active working memory deficit in schizophrenic patients, as supported by poor performance in 3-7 CPT in this study. Similar results on working memory were found in other studies with tasks relating to spatial working memory load.24
Patients with younger age and male gender have been found to have better degraded CPT performance (overall hit rate and sensitivity) in a large-scale community study in Taiwan, indicating that controlling for age and sex is important in CPT studies.21 Another confounding factor is level of education, as higher level of education is also associated with higher hit rate and sensitivity.21 In this study, the level of education in the schizophrenic patients was controlled for.
In addition, anticholinergic medication has been found to impair memory, especially verbal memory.25,26 Its effect on active working memory is unknown. In this study, the dose of anticholinergic medication was not correlated with CPT performance and there was no difference in performance between those with or without anticholinergic medication. However, the sample size of this study is too small to be conclusive in this regard, and further study is warranted. There was no difference in CPT performance between patients taking and not taking atypical and typical antipsychotics in this study. Clozapine has possible favour- able effects on verbal fluency and motor speed, but possible detrimental effects on visual memory and verbal working memory.27,28 Risperidone may have beneficial effects on verbal working memory.29 Therefore, bearing in mind that degraded CPT taps early perceptual deficits and 3-7 CPT puts an additional demand on working memory, atypical antipsychotics are unlikely to be of benefit. However, this is again a tentative conclusion in view of the small number of subjects in this study.
Psychosis-proneness Scale
This study has also validated 2 important instruments measuring psychosis-proneness — the STA and the O-LIFE. The local results (means, internal consistency, test-retest reliabilities) were highly comparable to those obtained in Western populations. Major limitations are the small sample size (n = 85) and the fact that sampling was done from a preselected population (university undergraduates). Further validation with a large community sample is warranted if these scales are to be applied to future research in high-risk individuals.
Degraded Continuous Performance Tests as a Vulnerability Marker of Psychosis
In the first longitudinal study of recent-onset schizophrenic patients, Nuechterlein et al administered both degraded and 3-7 CPT to a group of schizophrenic patients during both remitted and psychotic states.4 These investigators found a persistently high deficit in signal/noise discrimination (sensitivity index, d¢) in schizophrenic patients across both psychotic and remitted states compared with normal subjects tested at similar intervals. They also found that the sensitivity index was impaired among the schizophrenic patients (n = 17) on the memory-load version of CPT during both remitted and psychotic states, the impairment being much stronger during relapse. Degraded CPT can therefore be classified as a stable vulnerability indicator, as this impair- ment occurs during symptomatic and asymptomatic periods and does not vary significantly with the psychotic state. 3-7 CPT yields a pattern that suggests a potential mediating vulnerability indicator as this is abnormal across clinical states, but becomes more deviant during, or possibly before, psychotic episodes.4 The 3-7 CPT uses remembered context in which the present stimulus occurs as a cue of significance, suggesting that disturbances in use of active memory may be more closely linked to active psychotic periods in schizophrenia.22,30
The study by Nuechterlein et al provides further evidence that early perceptual analysis, tapped by degraded CPT, is a stable vulnerability marker across clinical states and varying degrees of psychotic symptoms.4 On the other hand, 3-7 CPT, with its demand on active working memory, may only become deficient in the face of active psychotic breakdown.
CPT performance deficit is only apparent in high-risk subjects when high-demand versions are used. Why do high- risk subjects manifest performance deficits in high- processing–load CPT, but not in conventional CPT? The answer seems to lie in the demand on early perceptual analysis.5 At least some CPT deficits may rely on early sensory/perceptual processes.31 Because the CPT involves very brief presentations, the stimuli are relatively poor perceptual images. High-risk subjects are likely to have milder deficits in early perceptual analysis, which are only exposed when the CPT tasks have a high demand on early perceptual analysis.31 Results from backward masking32 and span of apprehension performance33 (both tests rely on early sensory/perceptual analysis), have provided further evidence that very early sensory/perceptual analysis may be associated with vulnerability to psychosis.
Nuechterlein et al have argued that CPT is a stable vulnerability marker because deficits were found in patients in symptomatic remission, individuals at high risk of schizophrenia, siblings or parents of schizophrenic patients, and in schizotypal patients.4 A high-processing-load version of CPT is usually required to detect the deficits in schizotypal patients — for example, the CPT-identical pair (CPT-IP) version, in which the subject has to identify targets as stimuli that appear in 2 successive trials.
One condition uses 4-digit numbers as stimuli and another uses a series of nonsense shapes. CPT-IP was used in a schizotypal study15 and 1-9 CPT with 25% degraded stimuli in a study in Taiwan by Chen et al.21 There was significant correlation between measures of psychosis- proneness and overall hit rate and sensitivity in high- processing versions of CPT. Chen et al demanded possibly even higher processing load as active working memory, sustained attention and early perceptual analysis were required in their CPT version.21
In the current study, the components of working memory and early perceptual analysis were studied separately with 3-7 CPT and degraded CPT, respectively. There were significant correlations between overall hit rate and overall sensitivity of degraded CPT with mild schizotypal symptoms (STA) and cognitive disorganisation (O-LIFE), suggesting that early perceptual deficits may underline non-clinical psychosis-proneness traits (schizotypal traits and mild thought disorders) in the general population. These significant differences in degraded CPT overall hit rate and overall sensitivity were confirmed when only the high schizotypal subjects (STA score greater than 75th percentile) were compared with low schizotypal subjects (STA score less than 25th percentile). Previous work supports a strong association between thought disorder in schizophrenia and poor performance in the high processing load version of CPT.34 The correlation was modest, emerged only when the patients were in remission, and was relatively specific for those types of thought disorders characteristic of schizophrenia.
The lack of correlation between 3-7 CPT performance and psychosis-proneness scales in this study suggest that 3-7 CPT might not be a sensitive enough test for active working memory, or that active working memory might not play a significant role in non-clinical, mild schizotypal symptoms. Nevertheless, active working memory may play a more important role in clinically established schizophrenia, as supported by the poor performance of schizophrenia across all performance indexes for 3-7 CPT.
In the study of Nuechterlein et al, the decline in 3-7 CPT performance across clinical states (remitted versus acute relapse) pointed to the possibility that working memory might actually deteriorate upon relapse.4 However, the significant results found in correlation analyses should be viewed as tentative, as the statistical significance was lost once Bonferroni’s correction was applied to allow for multiple analyses. Therefore, this study should be regarded as a pilot for further research involving a larger community sample.
The lack of statistical difference in CPT performance between those with family history and those without family history demands further explanation, as multiple studies have found that family members of schizophrenic patients have poorer CPT performance.9,11 This may be due to the relatively small number of subjects with family history (n = 8), and that family history of psychiatric illnesses may encompass many other possible diagnoses other than schizophrenia. Studies have shown that CPT performance deficit is relatively specific for schizophrenic patients11,35 and their relatives.8,10,11
Limitations
The major limitation of this study is the small sample size used for the validation of CPT and psychosis-proneness scales. Therefore, the results can only be regarded as tentative and further study evaluating a larger sample is necessary for confirmation.
Recruitment of university students for the exploration of the relationship between psychosis-proneness and CPT is a biased sample, preselected initially for university admission. Moreover, as the sample of university students was not obtained randomly, this is not a representative sample of university students in Hong Kong. However, it should be noted that academic ability does not preclude a liability for psychopathology.36 The population from which the sample was drawn was probably censored for early-onset variants of severe psychopathology, but liability for late- onset psychoses or schizophrenia-spectrum disorders was not diminished in this sample.
Conclusion
This study provides some preliminary evidence to suggest that early perceptual deficits, as measured by degraded CPT, may contribute to the development of non-clinical, mild schizotypal symptoms in the general population.
References
- Chapman J. The early symptoms of schizophrenia. Br J Psychiatry 1966;112:225-251.
- Anscombe R. The disorder of consciousness in schizophrenia. Schizophr Bull 1987;13:241-260.
- Rosvold HE, Mirsky A, Sarason I. A continuous performance test of brain damage. J Clin Psychol 1956;20:343-350.
- Nuechterlein KH, Dawson ME, Ventura J. Testing vulnerability models: stability of potential vulnerability indicators across clinical state. In: Hafner H, Gattaz WF, editors. Search for the causes of schizophrenia. Vol II. Heidelberg: Springer-Verlag Press 1991:177-191.
- Green MF. Neurocognitive indicators of vulnerability to schizophrenia. In: Green MF. Schizophrenia from a neurocognitive perspective. Probing the impenetrable darkness. Massachussetts: Allyn and Bacon 1997: 61-82
- Wohlberg GW, Kornetsky C. Sustained attention in remitted schizophrenics. Arch Gen Psychiatry 1973;28:533-537.
- Asarnow RF, MacCrimmon DJ. Residual performance deficit in clinically remitted schizophrenics: a marker of schizophrenia? J Abnorm
Psychol 1978;87:597-608.
- Steinhauer SR, Zubin J, Condray R. Electrophysiological and behavioural signs of attentional disturbance in schizophrenics and their siblings. In: Tamminga CA, Schulz SC, editors. Schizophrenia research: advances in neuropsychiatry and psychopharmacology. Vol 1. New York: Raven Press 1991:169-178.
- Cornblatt BA, Lenzenweger MF, Erlenmeyer-Kimling L. The continuous performance test, identical pairs. Version II. Contrasting attentional profiles in schizophrenic and depressed patients. Psychiatry Res 1989;29:65-68.
- Nuechterlein KH. Signal detection in vigilance tasks and behavioural attributes among offspring of schizophrenic mothers and among hyperactive children. J Abnorm Psychol 1983;92:4-28.
- Mirsky AF, Ingraham LJ, Kugelmass S. Neuropsychological assessment of attention and its pathology in the Israel cohort. Schizophr Bull 1995;21:193-204.
- Bentall RP, Jackson HF, Pilgrim D. Abandoning the concept of “schizophrenia”: some implications of validity arguments for psychological research into psychotic phenomena. Br J Clin Psychol 1988;27:303-324.
- 13. Chapman LJ, Chapman JP, Kwapil TR. Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol 1994;103:171-183.
- Romme MA, Escher S. Hearing voices. Schizophr Bull 1989;15: 209-216.
- Lenzenweger MF, Cornblatt BA, Putnick M. Schizotypy and sustained attention. J Abnorm Psychol 1991;100:84-89.
- Condray R, Steinhauer SR. Schizotypal personality disorders in individuals with and without schizophrenic relatives: similarities and contrasts in cognitive functioning. Schizophr Res 1992;7:33-41.
- Harvey PD, Keefe RS, Mitropoulou V, DuPre R, Lees Roitman SE, Mohs RC, et al. Attentional markers of vulnerability to schizophrenia: performance of patients with schizotypal and non-schizotypal personality disorders. Psychiatry Res 1996;60:49-56.
- Lees Roitman SE, Cornblatt BA, Bergman A, Obuchowski M, Mitropoulou V, Keefe R, et al. Attentional functioning in schizotypal personality disorder. Am J Psychiatry 1997;154:655-660.
- Mason O, Claridge GS, Jackson M. New scales for the assessment of schizotypy. Pers Individ Dif 1995;1:7-13.
- Claridge GS, Broks P. Schziotypy and hemisphere function. I: theoretical consideration and the measurement of schizotypy. Pers Individ Dif 1984;5:633-648.
- Chen WJ, Hsiao CK, Hsiao LL, Hwu HG. Performance of continuous performance test among community samples. Schizophr Bull 1998;24:163-174.
- 22. Nuechterlein KH, Dawson ME, Green MF. Information processing abnormalities as neuropsychological vulnerability indicators for Acta Psychiatr Scand Suppl 1994;384:71-79.
- Rawlings D, Freeman JL. Measuring paranoia/suspiciousness. In: Claridge g, editor. Schizotypy. Implications for illness and health. Oxford: Oxford University Press;1997:38-60.
- Park S, Holzman PS. Schizophrenics show spatial working memory deficits in schizophrenia. Arch Gen Psychiatry1992;49:975-982.
- Perlick D, Stastny P, Katz I, Mayer M, Mattis S. Memory deficits and anticholinergic levels in chronic schizophrenia. Am J Psychiatry 1986;143:230-232.
- Tune LE, Strauss ME, Lew MF, Brietlinger E, Coyle JT. Serum levels of anticholinergic drugs and impaired recent memory in chronic schizophrenic patients. Am J Psychiatry 1982;139:1460-1462.
- Goldberg TE, Greenberg RD, Griffiin SJ, Gold JM, Kleinman JE, Pickar D, et al. The effect of clozapine in cognition and psychiatric symptoms in schizophrenia. Br J Psychiatry 1993;162:43-48.
- Hagger C, Buckley P, Kenny JT, Friedman L, Ubogy D, Meltzer HY. Improvement in cognitive functions and psychiatric symptoms in treatment-refractory schizophrenic patients receiving clozapine. Biol Psychiatry 1993;34:702-712.
- 29. Green MF, Marshall BD, Wirsching WC, Ames D, Marder SR, McGurk S, et al. Does risperidone improve verbal working memory in treatment- resistant schizophrenia? Am J Psychiatry 1997;154;799-804.
- Hemsley, DR. An experimental psychological model of schizophrenia. In: Hafner WF, Gattaz W, Janzarik W, editors. Search for the causes of schizophrenia. Heidelberg: Springer-Verlag Press;1989:230-245.
- Nuechterlein KH, Buchsbaum MS, Dawson M. Neuropsychological vulnerability to schizophrenia. In: AS David, JC Cutting, editors. The neuropsychology of schizophrenia. Hove: Lawrence Erlbaum Press;1994:53-74.
- Braff DL. Impaired speed of information processing in nonmedicated schizotypal patients. Schizophr Bull 1981;7:499-508.
- Asarnow RF, Nuechterlein KH, Marder SR. Span of apprehension performance, neuropsychological functioning, and indices of psychosis- proneness. J Nerv Ment Dis 1983;171:662-669.
- Nuechterlein KH, Edell WS, Norris M, Dawson ME. Attentional vulnerability indicators, thought disorder, and negative symptoms. Schizophr Bull 1986;12:408-426.
- Walker E. Attentional and neuromotor functions of schizophrenics, schizoaffectives, and patients with other affective disorders. Arch Gen Psychiatry 1981; 38:1355.
- Stangler R, Printz A. DSM-III diagnosis in a university population. Am J Psychiatry 1980;137:937-940.