East Asian Arch Psychiatry 2018;28:28-32
ORIGINAL ARTICLE
Dr MM Kwan, MBBS, Department of Psychiatry, Kowloon Hospital, Hong Kong.
Dr Desmond GH Nguyen, MBBS, MHA, MRCPsych, FHKCPsych, FHKAM (Psychiatry). Department of Psychiatry, Kowloon Hospital, Hong Kong.
Dr Roger MK Ng, MBChB, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, Kowloon Hospital, Hong Kong.
Address for correspondence: Dr MM Kwan, MBBS, Department of Psychiatry, Kowloon Hospital, 147A Argyle Street, Kowloon, Hong Kong.
Tel: 31297111; Email: kmm174@kh.ha.org.hk
Submitted: 29 March 2017; Accepted: 7 November 2017
Abstract
Objective: To assess the adherence to guidelines for electrocardiographic (ECG) monitoring in Hong Kong psychiatric in-patients who have been prescribed antipsychotic medications.
Methods: In-patients who had been prescribed antipsychotic drugs on hospital admission during the baseline audit period of 15 April 2015 to 16 July 2015 and the re-audit period of 28 January 2016 to 30 April 2016 were included. Quality improvement interventions were delivered after the baseline audit. ECG monitoring adherence was categorised as full adherence (ECG before taking antipsychotics), partial adherence (ECG after taking antipsychotics), or non-adherence (no ECG during hospital stay). Overall compliance was defined as full adherence plus partial adherence.
Results: The baseline audit and re-audit included 378 and 422 patients, respectively. Overall compliance with ECG monitoring increased significantly from the baseline audit to re-audit (40.2% vs. 69.9%; p < 0.001). Case-doctors having the grade of resident was associated with stronger adherence to ECG monitoring in both audits.
Conclusion: Adherence to ECG monitoring guidelines for in-patients who are prescribed antipsychotic drugs is low in Hong Kong, and junior doctors (residents) demonstrate stronger adherence than more- senior doctors.
Key words: Antipsychotic agents; Electrocardiography; Guideline adherence
Introduction
Antipsychotic drugs are commonly prescribed for a wide range of psychiatric diagnoses, in addition to their approved use for schizophrenia and bipolar affective disorder.1 However, patients taking antipsychotic medications have an increased rate of sudden cardiac death.2 In a meta- analysis in 2016, sudden cardiac death was reported to be associated with antipsychotic use, mediated by the effect of antipsychotics on a cardiac potassium channel that is coded by the human Ether-à-go-go-related (hERG) gene.3 This cardiac potassium channel is responsible for the rapid delayed rectifier potassium current. Blockade of this channel by antipsychotics delays cardiac repolarisation and induces heterogeneity of electrical phasing in different ventricular structures. Channel blockade thus increases the risk of potentially lethal polymorphic ventricular arrhythmia (torsade de pointes) and ultimately leads to sudden cardiac death in some patients.
On electrocardiography (ECG), lengthened cardiac repolarisation is demonstrated as prolongation of the heart rate–corrected QT (QTc) interval.4 Different antipsychotics have varying effects on QTc prolongation. The Arizona Center for Education and Research in Therapeutics, United States, classifies antipsychotics on the basis of their potential to cause QT prolongation and torsade de pointes. Both the United Kingdom’s National Institute for Clinical Excellence and The Maudsley Prescribing Guidelines in Psychiatry recommend that ECG be performed in patients who are prescribed antipsychotics on admission to hospital.5,6 This study aimed to assess the adherence to guidelines for hospital ECG monitoring in Hong Kong psychiatric in- patients who were prescribed antipsychotic medications.
Methods
This clinical audit study was approved by the Kowloon Central / Kowloon East Cluster Research Ethics Committee of the Hong Kong Hospital Authority (Ref No. KC/KE- 15-0005/ER-2). During the baseline audit period between 15 April 2015 and 16 July 2015 and the re-audit period between 28 January 2016 and 30 April 2016, in-patients who had been admitted to 4 psychiatric wards of Kowloon Hospital, Hong Kong, and subsequently discharged from the Kowloon Psychiatric Observation Unit, and who had been prescribed antipsychotics on admission were included. No patients were excluded based on their diagnoses or prescription periods.
Patient data were retrieved and included age, sex, smoking status, presence of diabetes mellitus and hypertension, pre-existing cardiac illness, access to the public psychiatric service, history of violence, detention status under the Mental Health Ordinance, grade of attending doctor, diagnosis based on the ICD-10,7 antipsychotics prescribed, ECG results, and clinical outcome in terms of adverse cardiac events during the hospital stay and up to 8 weeks after discharge. Patient history and propensity for violence was classified based on the Special Care System for psychiatric patients in Hong Kong. The prescribed dose of antipsychotics was converted to the equivalent dose of chlorpromazine, according to published data.6,8-11 The QTc value was calculated from the ECG results by using the Bazett formula,12 which is a widely used heart- rate correction formula in clinical practice.13 Prolongation of the QTc interval was defined as QTc of >450 msec in males and >470 msec in females.14 Adverse cardiac events were retrieved from the Hong Kong Hospital Authority Clinical Management System (CMS) and included torsade de pointes, arrhythmias, cardiac illnesses, sudden cardiac death, and cardiac-related mortalities.
Quality improvement interventions were delivered after the baseline audit. On 27 August 2015, a consultant from the Department of Cardiology at Queen Elizabeth Hospital gave a 1-hour lecture on antipsychotic-related ECG changes to doctors in the Department of Psychiatry at Kowloon Hospital as part of the weekly continuing medical education programme. During the re-audit period, a written reminder of the need for ECG monitoring of in-patients taking antipsychotics was attached to the Medication Administration Record.
Adherence to ECG monitoring guidelines was categorised as full adherence (ECG before taking antipsychotics), partial adherence (ECG after taking antipsychotics), or non-adherence (no ECG during hospital stay). Overall compliance was defined as full adherence plus partial adherence.
Data were analysed using SPSS (Windows version 20.0; IBM Corp, Armonk [NY], US). The 3 adherence groups were compared by using analysis of variance or the chi-square test, as appropriate. Ordinal regression analysis was used to determine variables associated with ECG monitoring adherence.
Results
During the baseline audit period between 15 April 2015 and 16 July 2015, 540 patients completed their hospital stay. Of these, 378 (70.0%) had been prescribed antipsychotics on admission and were thus included. Of the 378 patients, 259 had previously been prescribed antipsychotics, and 8 had undergone ECG in the past year; all 8 had abnormal findings.
In the re-audit period between 28 January 2016 and 30 April 2016, 560 patients completed their hospital stay, 422 (75.4%) of whom had been prescribed antipsychotics on admission and were included. Of these, 302 had previously been prescribed antipsychotics, 11 of whom had undergone ECG within the past year; all 11 had abnormal findings.
Of the patients in the baseline and re-audit periods, 44.7% and 35.5%, respectively, were prescribed antipsychotics (haloperidol or olanzapine) on an ‘as- required’ basis for intramuscular sedation. These patients consisted of 168 (baseline) and 148 (re-audit) who were given haloperidol, and 1 (baseline) and 2 (re-audit) who were given olanzapine.
The percentage of adverse cardiac events that occurred up to 8 weeks after hospital discharge decreased during the study period: from 3.7% (14 patients including 4 deaths) during the baseline audit to 1.7% (7 patients including 2 deaths) during the re-audit.
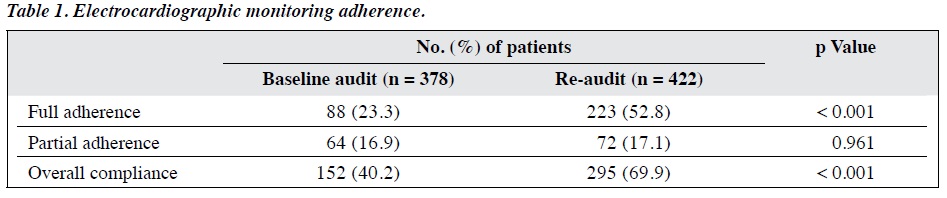
From the baseline audit to re-audit, the rate of full adherence with ECG monitoring increased significantly (23.3% vs. 52.8%; p < 0.001), as did the rate of overall compliance (40.2% vs. 69.9%; p < 0.001) [Table 1].
In the baseline audit, variables that were significantly different among the 3 adherence groups were patient age, diagnoses of organic mental disorders, length of stay in the current admission, case-doctor grade, and chlorpromazine equivalent-dose of dispensed antipsychotic on discharge (Table 2). In the re-audit, variables that were significantly different among the 3 groups were being a new patient to the public psychiatric service, number of psychiatric admissions, case-doctor grade, admission-doctor grade, and case-doctor attendance at the staff continuing education lecture on antipsychotic-related ECG changes (Table 2).
An ordinal regression model was developed in which the significant variables were entered as independent variables; grade of doctor was categorised as ‘resident’ or
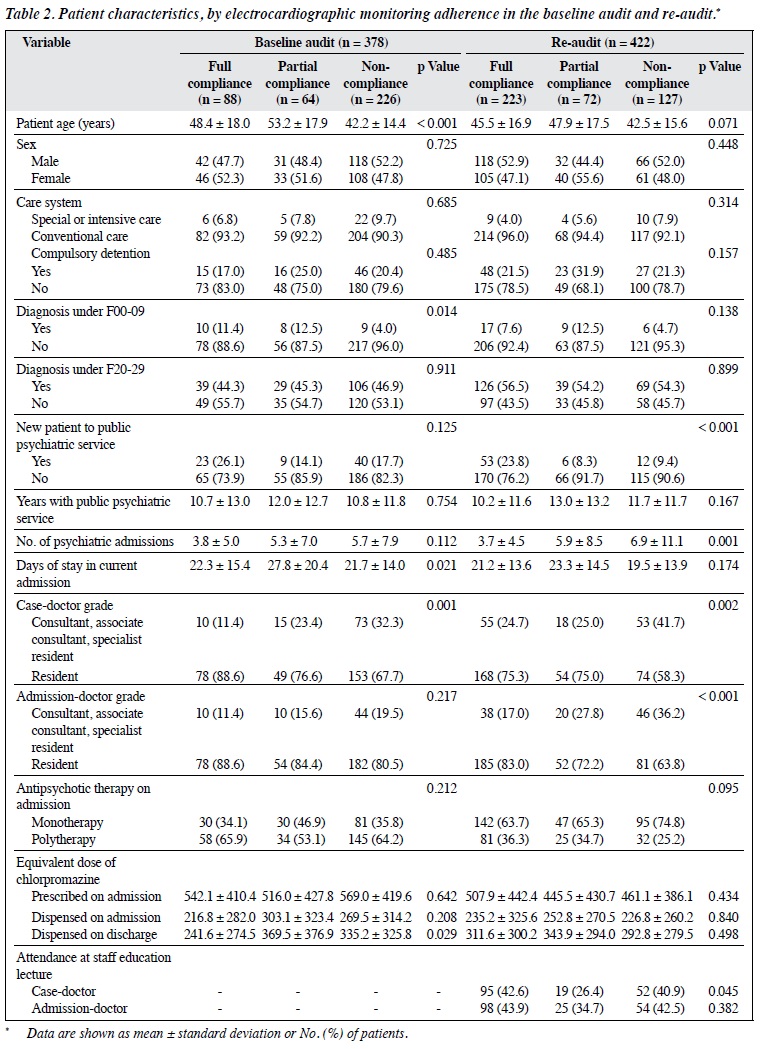
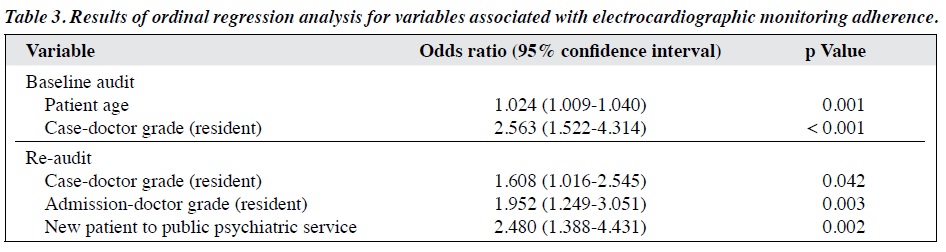
‘specialist resident or above’. Adherence to ECG monitoring was associated with patient age (odds ratio [OR] = 1.024; p = 0.001) and case-doctor of resident grade (OR = 2.563; p < 0.001) in the baseline audit, and case-doctor of resident grade (OR = 1.608; p = 0.042), admission-doctor of resident grade (OR = 1.952; p = 0.003), and being a new patient to the public psychiatric service (OR = 2.480; p = 0.002) in the re-audit (Table 3).
Discussion
Full adherence and overall compliance with ECG monitoring increased significantly from the baseline audit to re-audit (from 23.3% to 52.8% for adherence and from 40.2% to 69.9% for compliance). These findings reflect clinicians’ heightened awareness after the intervention of the importance of ECG monitoring for patients who are prescribed antipsychotics and the preference of performing an ECG before commencement of antipsychotic therapy to provide a baseline reference. Advanced patient age was associated with a higher level of ECG monitoring during the baseline audit. This finding suggests that doctors considered patients of advanced age to be more prone to drug-induced QTc prolongation. Although ECG monitoring adherence improved during the re-audit, patient age was not associated with the decision to perform ECG before or after antipsychotic use, and the decision was unlikely to be affected by different ward practices. In the re-audit, ECG monitoring adherence was higher when the patient was new to the public psychiatric service, perhaps owing to heightened awareness of the need for baseline ECG monitoring in new patients.
In both the baseline audit and re-audit, junior case- doctors of resident grade were more compliant with ECG monitoring than psychiatric specialists. In a meta-analysis of factors that influence implementation of clinical guidelines for health care professionals, less-experienced professionals were more inclined than more-experienced professionals to adhere to guidelines.15 Barriers to guideline adherence may have varying effects on doctors of different grades. In addition, baseline ECG monitoring for patients taking antipsychotics has been included in the guideline by the National Institute for Clinical Excellence only since 2009.16 Hence, senior doctors might still have clinical inertia to continue earlier practice.
In our study, 44.7% of patients at the baseline audit and 35.5% of patients at the re-audit were prescribed antipsychotics (haloperidol or olanzapine) as ‘as-required’ intramuscular sedation. Haloperidol was more commonly prescribed than olanzapine at both timepoints: only one patient in the baseline audit and two patients in the re-audit were prescribed olanzapine. However, ECG monitoring adherence was not associated with prescription of ‘as required’ sedation, possibly because of an overall increase in ECG monitoring adherence.
The proportion of patients experiencing adverse cardiac events up to 8 weeks after hospital discharge decreased from 3.7% during the baseline audit to 1.7% during the re-audit. Nonetheless, data retrieved from the Hospital Authority CMS may have underestimated the actual number of adverse cardiac events. In addition, there was no control group for comparison, and results could have been affected by confounding factors.
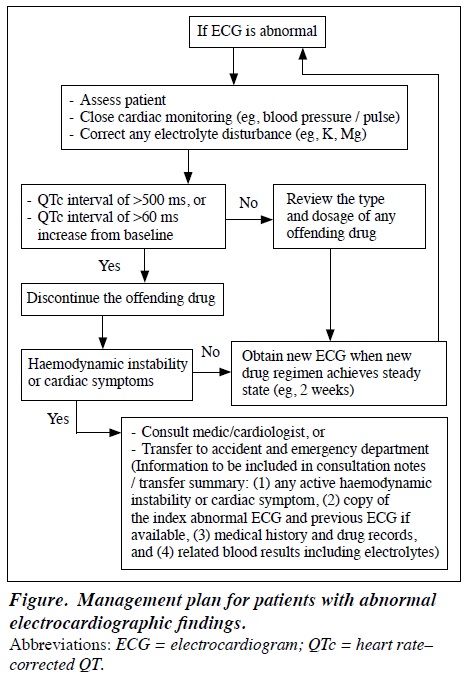
To facilitate multidisciplinary patient care, management options for patients with abnormal ECG findings were explored informally after this study among colleagues of various departments at the Kowloon Hospital. Some doctors expressed concern about a possible future increase in service demand with a rise in the number of consultations and urgent transfers. With reference to the American Heart Association and the American College of Cardiology Foundation,17 a management plan for in- patients with abnormal ECG findings was drafted (Figure). Appropriate investigations (including blood tests for electrolyte disturbance and follow-up ECG) and management options (including alterations to the antipsychotic regimen and consultation for medical advice) were proposed for patients with abnormal ECG findings. The management plan was endorsed by the Quality and Safety Committee of the Department of Psychiatry of Kowloon Hospital on 7 July 2016 and was introduced in a staff education lecture on 18 August 2016, with presentation slide handouts. ECG monitoring of in-patients who are prescribed antipsychotics is non-invasive and practical; further discussion with management and administrative staff is warranted to develop a local guideline for ECG monitoring.
This study had several limitations. It was a clinical audit and data accessed were limited to those in the public health care system; thus, it was not able to determine all variables that may affect ECG monitoring adherence. Doctor factors such as awareness of existing guidelines for antipsychotic use and knowledge of the potential antipsychotic QTc prolongation effect were not assessed; identifying barriers to adherence may help improve future practice. Adverse cardiac events were recorded only up to 8 weeks after hospital discharge and were retrieved from the discharge summary of patients in the Hospital Authority CMS. This method may have underestimated the actual number of adverse cardiac events. Finally, patients from the private sector were not investigated.
Conclusion
Adherence to ECG monitoring guidelines for in-patients who are prescribed antipsychotic drugs was low, and junior doctors (residents) demonstrated stronger adherence than more senior doctors. However, overall compliance with ECG monitoring increased significantly after quality improvement interventions (a staff continuing education lecture and reminders). Regular audits and staff education should be conducted to reinforce good clinical practice. Further discussion with management and administrative staff is needed to establish guidelines for routine ECG monitoring. Collaboration between psychiatric and medical disciplines is recommended for multidisciplinary management of patients with abnormal ECG findings.
Declaration
The authors have no conflicts of interest to disclose.
References
- Marston L, Nazareth I, Petersen I, Walters K, Osborn DP. Prescribing of antipsychotics in UK primary care: a cohort study. BMJ Open 2014;4:e006135. cross ref
- Ray WA, Chung CP, Murray KT, Hall K, Stein CM. antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med 2009;360:225-35. cross ref
- Salvo F, Pariente A, Shakir S, Robinson P, Arnaud M, Thomas S, et al. Sudden cardiac and sudden unexpected death related to antipsychotics: A meta-analysis of observational studies. Clin Pharmacol Ther 2016;99:306-14. cross ref
- Reilly JG, Ayis SA, Ferrier IN, Jones SJ, Thomas SH. QTc-interval abnormalities and psychotropic drug therapy in psychiatric patients. Lancet 2000;355:1048-52. cross ref
- National Collaborating Centre for Mental Health. Psychosis and schizophrenia in adults: treatment and management. The National Institute for Health and Care Excellence; 2014. Available from: https:// www.ncbi.nlm.nih.gov/pubmed/25340235.
- Taylor D, Paton C, Kapur S. The Maudsley prescribing guidelines in psychiatry. John Wiley & Sons; 2015.
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization; 1992.
- Atkins M, Burgess A, Bottomley C, Riccio M. Chlorpromazine equivalents: a consensus of opinion for both clinical and research applications. Psychiatrist Bulletin 1997;21:224-6. cross ref
- Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64:663-7. cross ref
- Bazire S. Psychotropic Drug Directory 2013/14: The Professionals’ Pocket Handbook and Aide Memoire. Lloyd-Reinhold Communications; 2013.
- 1 Joint Formulary Committee. BNF 70: British National Formulary. Pharmaceutical Press; 2015.
- Bazett HC. An analysis of the time-relations of electrocardiograms. Ann Noninvasive Electrocardiol 1997;2:177-94. cross ref
- Darpo B, Nebout T, Sager PT. Clinical evaluation of QT/QTc prolongation and proarrhythmic potential for nonantiarrhythmic drugs: the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use E14 guideline. J Clin Pharmacol 2006;46:498-507. cross ref
- Committee for Proprietary Medicinal Products. Points to consider: the assessment of the potential for QT interval prolongation by non- cardiovascular medicinal products. The European Agency for the Evaluation of Medicinal Products; 1997.
- Francke AL, Smit MC, de Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak 2008;8:38. cross ref
- National Collaborating Centre for Mental Health. Schizophrenia: Core interventions in the treatment and management of schizophrenia in adults in primary and secondary care. National Collaborating Centre for Mental Health; 2009.
- Drew BJ, Ackerman MJ, Funk M, Gibler WB, Kligfield P, Menon V, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation 2010;121: 1047-60. cross ref