East Asian Arch Psychiatry 2021;31:13-18 | https://doi.org/10.12809/eaap1961
ORIGINAL ARTICLE
Amlan Kusum Jana, KPC Medical College & Hospital, Kolkata, India
Address for correspondence: Amlan Kusum Jana, KPC Medical College & Hospital, Kolkata, India.
Email: amlankjana@gmail.com
Submitted: 18 September 2019; Accepted: 14 August 2020
Abstract
Objectives: To determine factors associated with remission from positive symptoms in Indian patients with schizophrenia.
Methods: We evaluated 151 patients (99 men and 52 women) aged 18 to 65 years who were diagnosed with schizophrenia and followed up for ≥6 months (with a minimum of two evaluations). We assessed psychopathology, the level of best functioning in the past year, premorbid functioning (up to 1 year), daily living skills, medication adherence, adverse effects to medications, the number of stressful events in the 6 months before illness onset, perceived social support, expressed emotion from family, and personal construct of empowerment. Remission from positive symptoms of schizophrenia was defined as simultaneous attainment of a score of ≤3 (mild) for ≥6 months in the following symptoms: delusions, concept disorganisation, hallucinatory behaviour, unusual thought content, mannerisms, and posturing. Patients were categorised as remitted and non-remitted.
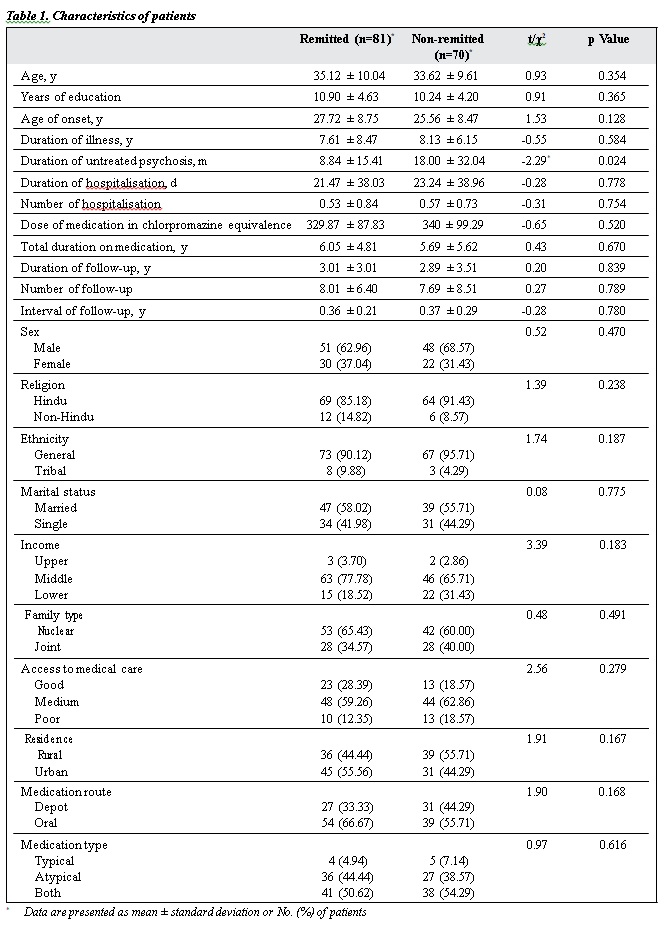
Results: Of 151 patients, 81 (53.64%) fulfilled the remission criteria. Compared with non-remitted patients, remitted patients had a shorter duration of untreated psychosis (t = -2.29, p < 0.05), better premorbid functioning in childhood (t = -1.99, p < 0.05) and general (t = -9.34, p < 0.001) subscale, higher medication adherence (t = 6.91, p < 0.001), higher daily living skills ( t = 8.65, p < 0.001), better perceived social support (t = 6.69, p < 0.001), higher empowerment (t = 5.64, p < 0.001), and received higher warmth (t = 1.99, p < 0.05) and lower hostility (t = -4.00, p < 0.001), dissatisfaction (t = -6.96, p < 0.001), and critical comments (t = -2.48, p < 0.05) from family members. Predictors of remission were duration of untreated psychosis (B = -0.020, p < 0.05), daily living skills (B = 2.063, p < 0.001), perceived social support (B = 0.084, p < 0.01), and dissatisfaction from family members (B = -0.621, p < 0.01).
Conclusions: 53.64% of patients with schizophrenia achieved remission from positive symptoms. Remission was more likely to occur in patients with shorter duration of untreated psychosis, better daily living skills, higher perceived social support, and less dissatisfaction from family members.
Key words: Remission induction; Schizophrenia; Social support
Introduction
Schizophrenia used to be considered a chronic condition that eventually leads to a deterioration of clinical and functional status. The core feature of schizophrenia is a downhill course and eventual adverse outcome. DSM III stated that “a complete return to premorbid level of functioning in individuals diagnosed with schizophrenia is so rare as to cast doubt upon the accuracy of the diagnosis”.1 However, the course of schizophrenia is heterogeneous and not necessarily a downhill one.2
Outcome is an ambiguous concept and is defined as the net balance of the clinical and functional descriptors at the endpoint. However, no such endpoint exists in dynamic conditions such as schizophrenia.3 There is no single parameter to assess the outcome, along with clinical symptoms, functionality, and social role performance.3 Newer parameters have been included in the concept of outcome, and rehabilitation or treatment satisfaction4 should also be considered.
The International Pilot Study of Schizophrenia5 investigated the nature of the illness using standardised methods and procedures to assess prognosis and illness course. In two Swiss studies of the long-term course of schizophrenia, a considerable proportion of patients achieved better outcome, with significant reduction in symptoms and a fair level of social and occupational functioning.2,6
Predictors of outcome of schizophrenia have been studied7,8 and include neurological soft signs9 and mental
The present study aimed to determine factors associated with remission from positive symptoms in Indian patients with schizophrenia. This study is a part of a larger study on outcomes of schizophrenia published previously.14
Methods
This cross-sectional retrospective study was approved by the ethics review board of the Central Institute of Psychiatry, Ranchi, India. Written informed consent was obtained from each patient. We evaluated 151 patients (99 men and 52 women) aged 18 to 65 years who were diagnosed with schizophrenia according to ICD-10-DCR15 and were on regular follow-up for ≥6 months (with a minimum of two evaluations). Patients with any comorbid major medical or neurological disorder, mental retardation or any comorbid psychiatric illness were excluded.
Psychopathology was assessed using the Positive and Negative Syndrome Scale (PANSS).16 The level of best functioning in the past year was assessed using the Global Assessment of Functioning.17 Premorbid functioning (up to 1 year) was assessed using the Cannon-Spoor Premorbid Adjustment Scale after modification (PAS).18 Daily living skills were assessed using the informant-rated version of the Independent Living Skills Survey (ILSS).19 Medication adherence was assessed using the Drug Attitude Inventory (DAI).20 Adverse effects to medications were assessed using the Udvalg for Kliniske Undersogelser21 and by interview of the patients. The number of stressful events in the 6 months before illness onset was recorded using the Presumptive Stressful Life Event Scale,22 which is an Indian adaptation of Social Readjustment Rating Questionnaire.23 Perceived social support was measured using the patient-rated PGI Social Support Questionnaire,24 which is based on the Social Support Questionnaire.25 Expressed emotion from family was assessed using the Attitude Questionnaire.26 Personal construct of empowerment was assessed using the self-report Empowerment Scale,27 with responses ranging from 1 (strongly agree) to 4 (strongly disagree).
Remission from positive symptoms of schizophrenia was assessed using the operationalised criterion proposed by the Remission in Schizophrenia Working Group.11 This requires simultaneous attainment of a score of ≤3 (mild) for ≥6 months in the following symptoms of the PANSS: delusions, concept disorganisation, hallucinatory behaviour, unusual thought content, mannerisms, and posturing. Patients were categorised as remitted and non-remitted.
Data were analysed using SPSS (Windows version 10; IBM Corp, Armonk [NY], US). Normality of data was checked using Shapiro-Wilk test. The remitted and non- remitted groups were compared using the independent t test for continuous variables and the Chi-squared test for categorical variables. Logistic regression was conducted with remission as outcome variable, and predicting variables were entered in the forward conditional method. Predictors included duration of untreated psychosis (DUP), severity of positive and negative symptoms, medication adherence, number of stressful events, expressed emotions, perceived social support, and empowerment. The assumption of lack of autocorrelation was tested with Durbin-Watson test. To identify multicollinearity, variance inflation factor was tested. The assumption of homoscedasticity was checked from the plots of standardised predicted values and standardised residuals. The Nagelkerke R2 was calculated to measure the variance explained by the model.
Results
Of 151 patients, 81 (53.64%) fulfilled the remission criteria. Compared with non-remitted patients, remitted patients had a shorter DUP (t = -2.29, p < 0.05), better premorbid functioning in childhood (t = -1.99, p < 0.05) and general (t = -9.34, p < 0.001) subscale in PAS, higher medication adherence in DAI (t = 6.91, p < 0.001), higher daily living skills in ILSS ( t = 8.65, p < 0.001), better perceived social support (t = 6.69, p < 0.001), higher empowerment (t = 5.64, p < 0.001), and received higher warmth (t = 1.99, p < 0.05) and lower hostility (t = -4.00, p < 0.001), dissatisfaction (t = -6.96, p < 0.001), and critical comments (t = -2.48, p < 0.05) from family members (Table 1).
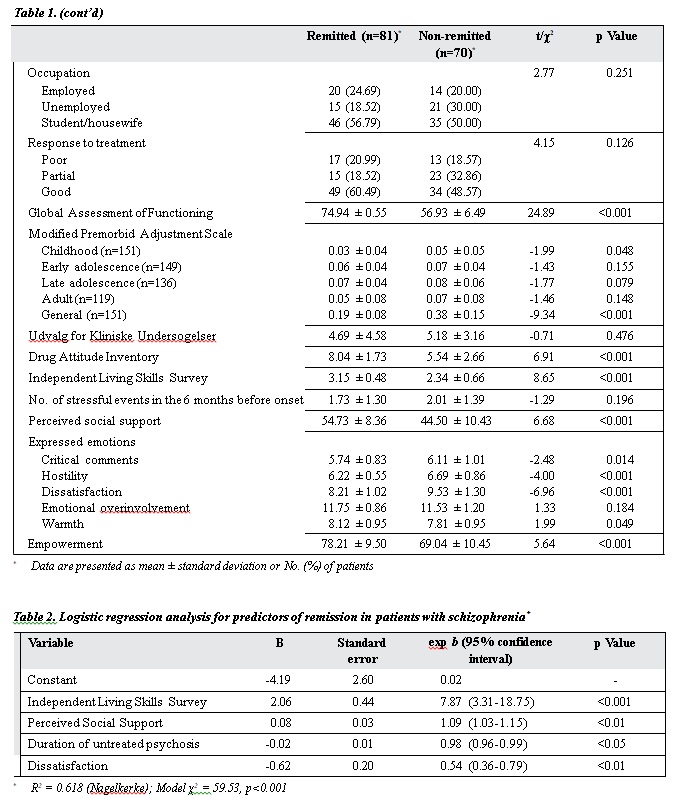
Predictors of remission were DUP (B = -0.020, Exp(B) = 0.980, p < 0.05), ILSS score (B = 2.063, Exp(B) = 7.873, p < 0.001), perceived social support (B = 0.084, Exp(B) = 1.088, p < 0.01), and dissatisfaction from family members (B = -0.621, Exp(B) = 0.538, p < 0.01) [Table 2]. The model explained 61.8% of the variance (adjusted R2 = 0.618) in remission.
Discussion
53.64% of the patients fulfilled the remission criteria, which have good sensitivity and specificity.28 The symptomatic remission rate has been reported to be 37.5%29 and 91.5%.30 Nonetheless, the proportion of patients showing enduring remission is smaller than that showing symptomatic remission for ≥6 months.30 The favourable outcomes of our patients may be because our institute is a renowned institute in India, or because only patients with regular follow-up were included. Generalisation of our findings should be done with caution, as this was a hospital-based study and many patients in the community do not receive any professional help.
Perceived social support and ILSS score positively predicted remission. Social support is believed to be bidirectional and is often determined by personality factors such as self-esteem, sociability, and locus of control.31 Two components determine the overall social support: individual’s own inner resources and characteristics (physical characteristics, biological predisposition, and cognitive capacity to acquire and organise knowledge of self and others) and individual’s external social environments.32
Symptoms, particularly if severe and long-standing, may produce more lasting deficits on the provision of support by family members.31 Schizophrenia is a chronic illness and thus affects social outcome early in the course. Higher social support, better coping and social support seeking33 have been shown to improve outcome. Satisfaction with social support positively influences the quality of life in schizophrenia patients.34
ILSS measures social, occupational, leisurely functions, and skills for daily living. Adequate heterosexual contacts and instrumental competence social adjustment occupational functioning affect outcome.35 Social cognition, which is the connecting link between symptomatic improvement and adequate socio-occupational functioning, is increasingly targeted in treatments of schizophrenia. Nowadays, the goal of treatment in schizophrenia is remission and recovery. Achieving adequate socio- occupational functioning is an essential step towards it. Independent functioning at various levels has a bilateral relation with clinical symptoms, as both tend to negatively influence each other.
Dissatisfaction in family members negatively predicted remission. Expressed emotions may be predictive of relapse and re-hospitalisations in schizophrenia patients. Expressed emotions may differentially affect psychosocial functioning and not much clinical functioning.36 Expressed emotions, specifically dissatisfaction, are associated with poor socio-occupational functioning in schizophrenia.37 The degree and frequency of expressed emotions can change with time, and expressed emotions tend to predict relapse better with long-standing illness. Expressed emotions are a valid prolonged predictor of relapses and rehospitalisations.38
DUP predicts remission9,32 and a favourable outcome (PANSS score).39 A short DUP is associated with better social, occupational, and symptomatic outcome.40 A meta- analysis concluded that DUP had a small but consistent correlation with poor general symptomatic outcome, more severe positive and negative symptoms, less likelihood of remission, and poor social functioning and global outcome.41 Longer DUP predicts worse clinical, functional, and cognitive outcomes in early-onset psychosis42 and predicts social anxiety in schizophrenia, which adversely affects outcome.43 DUP is an important parameter in India where health care system struggles to reduce the overall treatment gap in schizophrenia. Despite the presence of other protective factors, DUP alone can adversely impact the outcome of schizophrenia by worsening symptomatic and functional outcome through its influence on social cognition and social anxiety. Thus, early intervention in schizophrenia helps to improve the patient outcome.
Negative symptoms have been reported to be a predictor (negative) of remission in schizophrenia, along with participation in standardised psychological treatment,30 favourable early response to treatment, general psychopathological symptoms, and lesser psychotic episodes in the longitudinal course.29 However, negative symptoms or general psychopathology symptoms was not a predictor of remission in the present study.
One of the limitations of the present study is the homogeneity of the sample. Patients with comorbid illnesses (eg, obsessive-compulsive disorder, major depression, substance dependence) were excluded; these comorbid illnesses could be important predictors. The study is cross-sectional and retrospective. A study with a baseline assessment followed by prospective evaluations would have identified more predictors. A community-based study could have examined patients who could not reach out to hospitals. Assessment of family dynamics, expressed emotions, housing and living conditions, and social support in patients could have helped determine the real picture of outcomes of schizophrenia in India. Studies of psychosocial and biological parameters among patients in the community with a prospective design are warranted. The number of relapses in the past among patients could not be tracked, which could have been an important predictor.
Conclusion
53.64% of patients with schizophrenia achieved remission from positive symptoms. Remission was more likely to occur in patients with shorter duration of untreated psychosis, better daily living skills, higher perceived social support, and less dissatisfaction from family members.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed; 1980.
- Ciompi L. Catamnestic long-term study on the course of life and aging of schizophrenics. Schizophr Bull 1980;6:606-18. Crossref
- Jablensky A. Course and Outcome of Schizophrenia and Their Prediction. In: Gelder MG, Lopez-Ibor JJ, Andreasen NC, editors. New Oxford Textbook of Psychiatry. 2nd ed. Oxford University Press; 2000: 612-21.
- Lehman AF. Evaluating outcomes of treatments for persons with psychotic disorders. J Clin Psychiatry 1996;57(Suppl 11):61-7.
- World Health Organization. The International Pilot Study of Schizophrenia. Vol. 1. 1973.
- Bleuler M. The Schizophrenic Disorders: Long-Term Patient and Family Studies. Translated by SM Clemens. Yale University Press; 1978.
- Vaillant GE. The prediction of recovery in schizophrenia. J Nerv Ment Dis 1962;135:534-43. Crossref
- Stephens JH, Astrup C, Mangrum JC. Prognostic factors in recovered and deteriorated schizophrenics. Am J Psychiatry 1966;122:1116-21. Crossref
- Emsley R, Oosthuizen PP, Kidd M, Koen L, Niehaus DJ, Turner HJ. Remission in first-episode psychosis: predictor variables and symptom improvement patterns. J Clin Psychiatry 2006;67:1707-12. Crossref
- Torgalsbøen AK, Fu S, Czajkowski N. Resilience trajectories to full recovery in first-episode schizophrenia. Eur Psychiatry 2018;52:54-60. Crossref
- Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 2005;162:441-9. Crossref
- Liberman RP, Kopelowicz A, Venture J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int Rev Psychiatry 2002;14:256-72. Crossref
- Park SA, Sung KM. The effects on helplessness and recovery of an empowerment program for hospitalized persons with schizophrenia. Perspect Psychiatr Care 2013;49:110-7. Crossref
- Jana AK, Ram D, Praharaj SK. Empowerment and its associations in schizophrenia: a cross-sectional study. Community Ment Health J 2014;50:697-701. Crossref
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research. 1993.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76. Crossref
- Patterson DA, Lee MS. Field trial of the Global Assessment of Functioning Scale--Modified. Am J Psychiatry 1995;152:1386-8. Crossref
- van Mastrigt S, Addington J. Assessment of premorbid function in first- episode schizophrenia: modifications to the Premorbid Adjustment Scale. J Psychiatry Neurosci 2002;27:92-101.
- Wallace CJ, Liberman RP, Tauber R, Wallace J. The independent living skills survey: a comprehensive measure of the community functioning of severely and persistently mentally ill individuals. Schizophr Bull 2000;26:631-58. Crossref
- Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med 1983;13:177-83. Crossref
- Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K. The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand Suppl 1987;334:1-100. Crossref
- Singh G, Kaur D, Kaur H. Presumptive Stressful Life Event Scale. Agra: National Psychological Corporation; 1983.
- Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res 1967;11:213-8. Crossref
- Nehra R, Kulhara P, Verma S. Manual for PGI Social Support Questionnaire. Varanasi: Rupa Psychological Centre; 1998.
- Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: the social support questionnaire. J Pers Soc Psychol 1983;44:127-39. Crossref
- Sethi BB, Chaturvedi PK, Trivedi JK, Saxena NK. Attitude of family and outcome in schizophrenia. Indian J Soc Psychiatry 1985;1:186-93.
- Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer- constructed scale to measure empowerment among users of mental health services. Psychiatr Serv 1997;48:1042-7. Crossref
- van Os J, Burns T, Cavallaro R, Leucht S, Peuskens J, Helldin L, et al. Standardized remission criteria in schizophrenia. Acta Psychiatr Scand 2006;113:91-5. Crossref
- Marchesi C, Affaticati A, Monici A, De Panfilis C, Ossola P, Tonna M. Predictors of symptomatic remission in patients with first-episode schizophrenia: a 16 years follow-up study. Compr Psychiatry 2014;55:778-84. Crossref
- Gaebel W, Riesbeck M, Wölwer W, Klimke A, Eickhoff M, von Wilmsdorff M, et al. Rates and predictors of remission in first-episode schizophrenia within 1 year of antipsychotic maintenance treatment. Results of a randomized controlled trial within the German Research Network on Schizophrenia. Schizophr Res 2014;152:478-86. Crossref
- Brugha TS. Social Support and Psychiatric Disorder: Overview of Evidence. In: Brugha TS, editor. Social Support and Psychiatric Disorder Research Findings and Guidelines for Clinical Practice. Cambridge University Press; 1995: 1-40. Crossref
- Champion L. A Developmental Perspective on Social Support. In: Brugha TS, editor. Social Support and Psychiatric Disorder Research Findings and Guidelines for Clinical Practice. Cambridge University Press; 1995: 41-95. Crossref
- Rudnick A, Kravetz S. The relation of social support-seeking to quality of life in schizophrenia. J Nerv Ment Dis 2001;189:258-62. Crossref
- Guedes de Pinho LM, Pereira AMS, Chaves CMCB. Quality of life in schizophrenic patients: the influence of sociodemographic and clinical characteristics and satisfaction with social support. Trends Psychiatry Psychother 2018;40:202-9. Crossref
- Rosen K, Garety P. Predicting recovery from schizophrenia: a retrospective comparison of characteristics at onset of people with single and multiple episodes. Schizophr Bull 2005;31:735-50. Crossref
- Guada J, Hoe M, Floyd R, Barbour J, Brekke JS. How family factors impact psychosocial functioning for African American consumers with schizophrenia. Community Ment Health J 2012;48:45-55. Crossref
- Thonse U, Behere RV, Praharaj SK, Sharma PSVN. Facial emotion recognition, socio-occupational functioning and expressed emotions in schizophrenia versus bipolar disorder. Psychiatry Res 2018;264:354-60. Crossref
- Cechnicki A, Bielańska A, Hanuszkiewicz I, Daren A. The predictive validity of expressed emotions (EE) in schizophrenia. A 20-year prospective study. J Psychiatr Res 2013;47:208-14. Crossref
- Bachmann S, Bottmer C, Schroder J. One-year outcome and its prediction in first-episode schizophrenia--a naturalistic study. Psychopathology 2008;41:115-23. Crossref
- Whitty P, Clarke M, McTigue O, Browne S, Kamali M, Kinsella A, et al. Predictors of outcome in first-episode schizophrenia over the first 4 years of illness. Psychol Med 2008;38:1141-6. Crossref
- Penttilä M, Jääskeläinen E, Hirvonen N, Isohanni M, Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry 2014;205:88-94. Crossref
- Díaz-Caneja CM, Pina-Camacho L, Rodríguez-Quiroga A, Fraguas D, Parellada M, Arango C. Predictors of outcome in early-onset psychosis: a systematic review. NPJ Schizophr 2015;1:14005. Crossref
- Aikawa S, Kobayashi H, Nemoto T, Matsuo S, Wada Y, Mamiya N, et al. Social anxiety and risk factors in patients with schizophrenia: relationship with duration of untreated psychosis. Psychiatry Res 2018;263:94-100. Crossref