East Asian Arch Psychiatry 2023;33:44-64 | https://doi.org/10.12809/eaap2261
REVIEW ARTICLE
Beryl Yee, Department of Medicine, College of Medicine and Public Health, Flinders University, Adelaide, South Australia, Australia
Jeffrey CL Looi, Academic Unit of Psychiatry and Addiction Medicine, The Australian National University School of Medicine and Psychology, Canberra Hospital, Canberra, Australian Capital Territory, Australia
Madelyn Agaciak, Department of Medicine, College of Medicine and Public Health, Flinders University, Adelaide, South Australia, Australia
Stephen Allison, Department of Medicine, College of Medicine and Public Health, Flinders University, Adelaide, South Australia, Australia
Sherry Kit Wa Chan, Department of Psychiatry, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR, China
Tarun Bastiampillai, Department of Medicine, College of Medicine and Public Health, Flinders University, Adelaide, South Australia, Australia; Department of Psychiatry, Monash University, Melbourne, Victoria, Australia
Address for correspondence: Dr Madelyn Agaciak, College of Medicine and Public Health, Flinders University, Flinders Drive, Bedford Park, 5042, South Australia, Australia. Email: maddie.agaciak@sa.gov.au
Submitted: 14 December 2022; Accepted: 15 May 2023
Abstract
Objective: Clozapine is a potent antipsychotic medication with a complex receptor profile. It is reserved for treatment-resistant schizophrenia. We systematically reviewed studies of non-psychosis symptoms of clozapine withdrawal.
Methods: CINAHL, Medline, PsycINFO, PubMed, and the Cochrane Database of Systematic Reviews were searched using the keywords ‘clozapine,’ and ‘withdrawal,’ or ‘supersensitivity,’ ‘cessation,’ ‘rebound,’ or ‘discontinuation’. Studies related to non-psychosis symptoms after clozapine withdrawal were included.
Results: Five original studies and 63 case reports / series were included in analysis. In 195 patients included in the five original studies, approximately 20% experienced non-psychosis symptoms following discontinuation of clozapine. In 89 patients in four of the studies, 27 experienced cholinergic rebound, 13 exhibited extrapyramidal symptoms (including tardive dyskinesia), and three had catatonia. In 63 case reports / series included, 72 patients with non-psychosis symptoms were reported, which were catatonia (n=30), dystonia or dyskinesia (n=17), cholinergic rebound (n=11), serotonin syndrome (n=4), mania (n=3), insomnia (n=3), neuroleptic malignant syndrome (NMS) [n=3, one of them had both catatonia and NMS], and de novo obsessive compulsive symptoms (n=2). Restarting clozapine appeared to be the most effective treatment.
Conclusions: Non-psychosis symptoms following clozapine withdrawal have important clinical implications. Clinicians should be aware of the possible presentations of symptoms to ensure early recognition and management. Further research is warranted to better characterise the prevalence, risk factors, prognosis, and optimal drug dosing for each withdrawal symptom.
Introduction
Clozapine is the gold standard for managing treatment- resistant schizophrenia.1 In clinical practice, cessation of clozapine is typically due to adverse effects or patient non-adherence. Studies regarding withdrawal symptoms following antidepressant2 and benzodiazepine3 treatment cessation are widely reported, but studies of withdrawal of clozapine or other antipsychotics are limited. The main symptom associated with antipsychotics withdrawal is rebound psychosis,4 which is common in clozapine withdrawal.4,5 The non-psychosis symptoms after withdrawal of antipsychotics or clozapine are also clinically significant but not widely discussed.
Based on guidelines for differentiating withdrawal symptoms from a relapse of the primary disease,3 an acute, severe, and sudden onset of symptoms suggests withdrawal rather than a gradual relapse. Similarly, an alteration in disease course, such as a new-onset mood or movement disorder, or refractory illness that does not respond to previously effective medications, may also suggest a withdrawal symptom.6
Withdrawal symptoms can be classified as new withdrawal symptoms, rebound symptoms, and persistent post-withdrawal symptoms.6 New withdrawal symptoms typically peak within 36 to 96 hours after dosage decrease or discontinuation and are usually transient, lasting from several hours to <6 weeks. New-onset disorders, such as mood or movement disorders, are considered new withdrawal symptoms. Rebound psychosis after clozapine discontinuation is indicated by a sudden onset of symptoms seen in the original disorder, usually at greater intensity than baseline, that typically resolve within 6 weeks. Persistent post-withdrawal symptoms are those that do not resolve within 6 weeks and can be irreversible.
The unique receptor profile of clozapine, which differs from that of other antipsychotics, likely explains the symptomatology of clozapine withdrawal.7 Clozapine has a low affinity for the dopamine (D)2 receptor in the striatum but a high affinity for the D4 receptor. The D4 receptors concentrate in the frontal cortex and amygdala but are in small quantities in the basal ganglia. Clozapine also antagonises serotonin (5-HT) receptors, notably 5-HT1C and 5-HT2A, allowing dopamine release. Thus, clozapine can ameliorate symptoms without causing the extrapyramidal adverse effects associated with other antipsychotics.8 In addition, clozapine can antagonise A1 and A2 cholinergic receptors, exerting stronger anticholinergic actions than other antipsychotics.7,8 Other neuroleptics decrease gamma- aminobutyric acid (GABA) turnover, but clozapine increases GABA turnover in the substantia nigra. Thus, patients who develop tardive dyskinesia after taking other antipsychotics can experience tardive dyskinesia remission after switching to clozapine.8 Clozapine also exhibits antihistaminergic action at H1 receptors. Therefore, clozapine withdrawal involves a combination of dopamine, serotonin, choline, GABA, and histamine receptor interaction.7,8
In a systematic review of clozapine withdrawal symptoms in schizophrenia,9 the scope of symptoms was limited only to psychosis, catatonia, cholinergic, and serotonergic symptoms. This systematic review aims to identify all possible non-psychosis symptoms of clozapine withdrawal (catatonia, dyskinesia and dystonia, cholinergic rebound, serotonin syndrome, neuroleptic malignant syndrome, insomnia, mania, and obsessive-compulsive symptoms), their prevalence, and the best treatment options so that clinicians can better recognise and manage these conditions.
Methods
This systematic review was registered with PROSPERO (reference: 382789) and was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework. Databases CINAHL, Medline, PsycINFO, PubMed, and the Cochrane Database of Systematic Reviews were searched using the ‘cessation,’ ‘rebound,’ or ‘discontinuation’ (search 1). A preliminary literature review also yielded the keywords ‘catatonia,’ ‘cholinergic rebound,’ ‘dystonia or dyskinesia,’ ‘serotonin syndrome,’ and ‘neuroleptic malignant syndrome,’ each of which was combined with search 1 using ‘and’. Following review of major papers, keywords ‘delirium,’ ‘anxiety,’ ‘insomnia,’ ‘mania,’ and ‘seizure’ were also added. Using this reiterative approach, several rounds of searching were conducted for English-language papers published before December 2021.
The title and abstract of each paper were screened to determine relevance. Exclusion criteria were animal studies, case reports of psychosis symptoms of clozapine withdrawal only, studies involving concurrent withdrawal of clozapine and other drugs, and studies involving narrative reviews of clozapine withdrawal.
Full texts of included papers were assessed for eligibility. The study population was patients undergoing treatment with clozapine who had their dosage decreased or discontinued or switched to an alternative antipsychotic abruptly or with tapering. This included patients who were compliant or non-compliant with a prescribed regimen. Symptoms were considered to be due to clozapine withdrawal only if they were not caused by other factors. Both non-randomised controlled trials (RCTs) and RCTs were assessed for risk of bias using the validated tools ROBINS-I (Risk of Bias in Non-randomized Studies of Interventions) and RoB 2 (Risk of Bias 2), respectively.10,11 Case studies were eligible only if the patient’s demographics, clinical findings, diagnosis, and treatment were reported. The CARE guidelines were used to determine the quality of case studies.12
Results
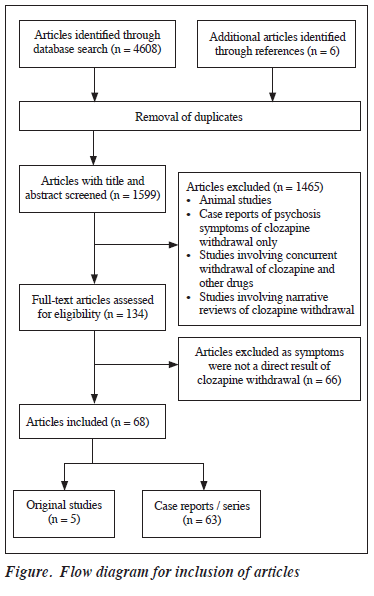
A total of 4608 papers were returned after searching. Six additional papers were identified through references of these papers. After removal of duplicates, 1599 remained. After screening their titles and abstracts, 1465 were excluded. The full text of the remaining 134 papers were assessed by two reviewers. 66 papers were excluded based on the exclusion criteria, whereas five original studies and 63 case reports / series were included in the analysis (Figure).
Original Studies
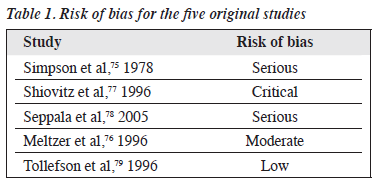
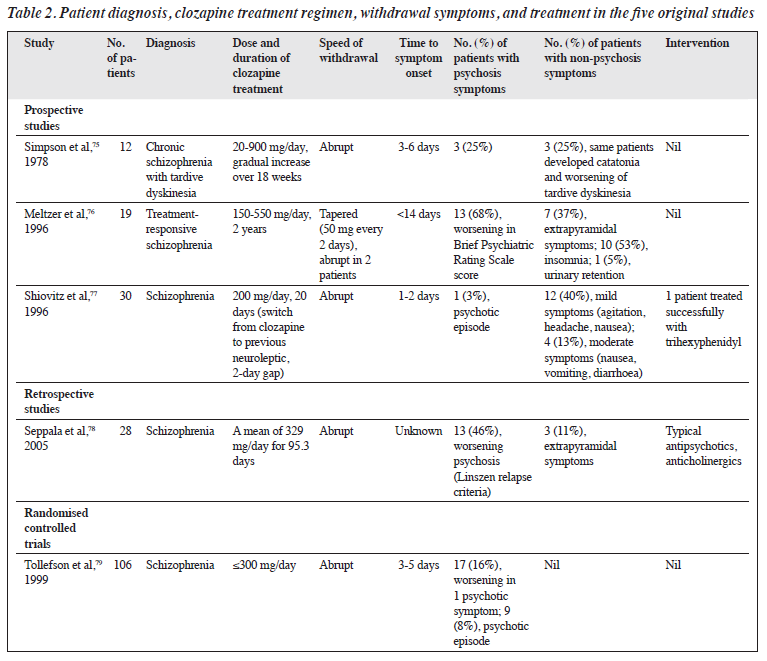
Five original studies reported psychosis symptoms after clozapine withdrawal. Three of these papers also reported non-psychosis symptoms. The risk of bias of the four non- RCTs was serious in two, critical in one, and moderate in one, whereas the risk of bias of the only RCT was low (Table 1).
In 195 patients included in these five studies, approximately 29% experienced psychotic symptoms and 20% experienced non-psychosis symptoms following discontinuation of clozapine (Table 2). In 89 patients included in the four non-RCTs, 27 experienced cholinergic rebound, 13 exhibited extrapyramidal symptoms (including tardive dyskinesia), and three had catatonia.
Case Reports / Series
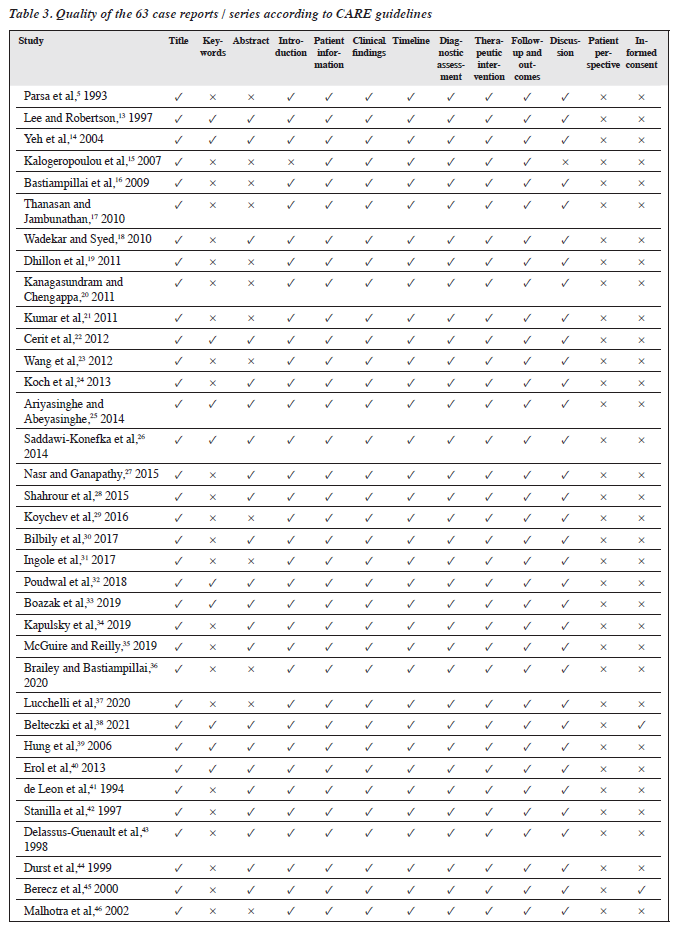
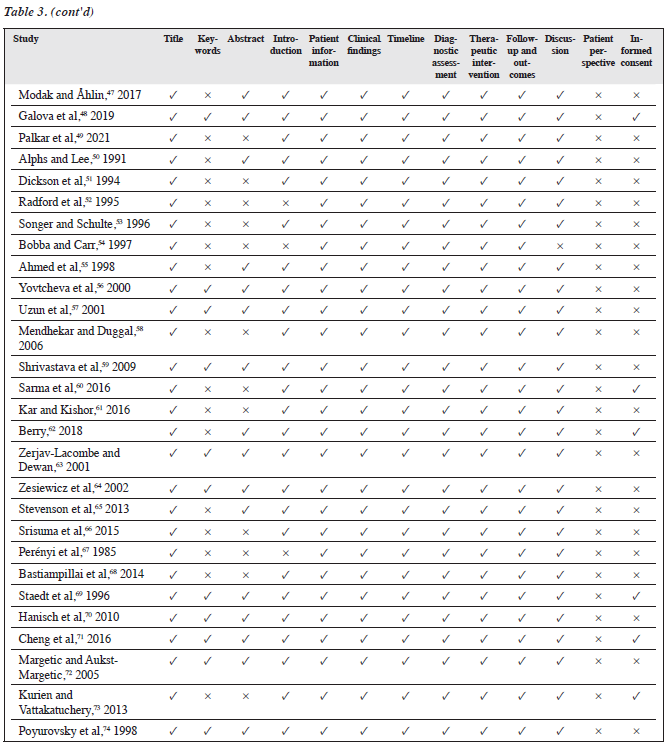
The quality of the 63 case reports / series was assessed according to the CARE guidelines (Table 3). In 63 case reports / series included, 72 patients with non-psychosis symptoms were reported, which were catatonia (n=30), dystonia or dyskinesia (n=17), cholinergic rebound (n=11), serotonin syndrome (n=4), mania (n=3), insomnia (n=3), neuroleptic malignant syndrome (NMS) [n=3, one of them had both catatonia and NMS], and de novo obsessive compulsive symptoms (n=2).
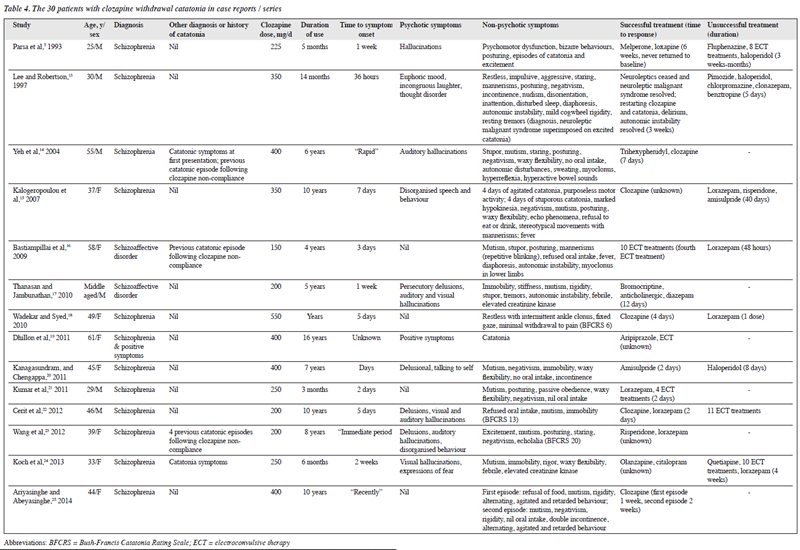
Catatonia
In the 30 patients presenting with catatonia, the mean patient age was 41 (range, 22-66) years and the male-to-female ratio was 1.7:1 (Table 4). The mean clozapine dose was 306 (range, 50-600) mg/day and the median duration of use was 66 (range, 2-120) months. The time from discontinuation to symptom onset ranged from 36 hours to 2 weeks, with 21 cases arising within 1 week. Psychotic symptoms were also present in 16 patients.
Restarting clozapine to treat catatonia was successful in 17 (57%) patients, whereas administration of non-clozapine antipsychotic (risperidone, olanzapine, aripiprazole, amisulpride, melperone, or clozapine) was successful in seven (23%) patients. Other successful treatments were electroconvulsive therapy (ECT) [n=6], lorazepam (n=11), trihexyphenidyl, bromocriptine, anticholinergics, diazepam, citalopram, procyclidine, levetiracetam, dantrolene, biperiden, and benztropine. The time to response ranged from 1 day to 3 months, with 15 patients responding within 1 week.
Unsuccessful treatments for catatonia involved lorazepam (n=10), haloperidol (n=4), ECT (n=6), risperidone (n=2), clonazepam (n=2), olanzapine, fluphenazine, pimozide, chlorpromazine, benztropine, amisulpride, quetiapine, aripiprazole, diphenhydramine, benzodiazepines, bromocriptine, zolpidem, and valproate. The treatment duration ranged from a single dose to 51 days.
Two patients with schizophrenia had catatonic symptoms before taking clozapine. Five patients had previous episodes of catatonia following clozapine withdrawal. Twenty patients reported symptoms fulfilling the DSM-5 criteria for catatonia. The Bush-Francis Catatonia Rating Scale was used to assess severity of catatonia in nine patients only. Cholinergic and serotonergic symptoms were described in one patient only.14 Neuroleptic malignant syndrome was described in one patient only.40

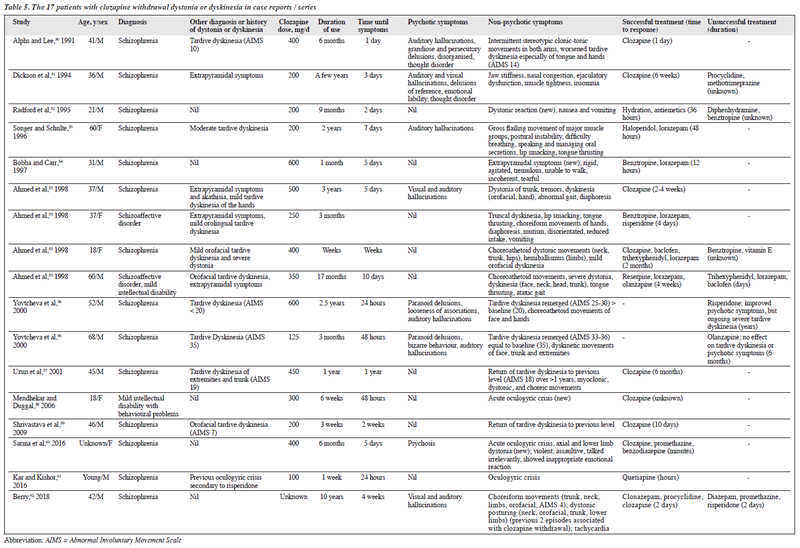
Dystonia or Dyskinesia
In the 17 patients presenting with dystonia or dyskinesia, the mean patient age was 38 (range, 18-68) years and the male-to-female ratio was 2.4:1 (Table 5). The mean clozapine dose was 330 (range, 100-600) mg/day and the median duration of use was 6 months (range, 1 week to 10 years). The time from discontinuation to symptom onset ranged from 1 day to 4 weeks, with 10 cases arising within 5 days. Psychotic symptoms were present in eight patients.
Restarting clozapine to treat dystonia or dyskinesia was successful in eight patients, whereas administration of non-clozapine antipsychotic (haloperidol, risperidone, olanzapine, quetiapine) was successful in four patients. Other successful treatments involved benzodiazepines (lorazepam [n=5], clonazepam [n=1], unspecified [n=1]), benztropine (n=2), baclofen, trihexyphenidyl, reserpine, promethazine, and procyclidine. The time to response ranged from 12 hours to 6 months, with nine patients responding within 1 week.
Unsuccessful treatments for dystonia or dyskinesia involved benztropine (n=2), risperidone (n=2), olanzapine, promethazine, diphenhydramine, procyclidine, methotrimeprazine, trihexyphenidyl, lorazepam, diazepam, and baclofen. The treatment duration ranged from 2 days to years.
Of the 17 patients, five had no previous movement disorders and 12 were known to have previous extrapyramidal symptoms (EPS) or tardive dyskinesia that were caused by other antipsychotics but were resolved with clozapine treatment. After clozapine withdrawal, the re- emergence of tardive dyskinesia was of similar severity as previously experienced (n=4) or of greater severity (n=2) or of different neuroleptic symptoms (n=6). The Abnormal Involuntary Movement Score was used to assess the severity of movement disorders in five patients only.
Cholinergic Rebound
In the 11 patients presenting with cholinergic rebound, eight had a diagnosis of schizophrenia and three had a diagnosis of schizoaffective disorder (Table 6). The mean patient age was 41 (range, 26-65) years and the male-to-female ratio was 10:1. The mean clozapine dose was 420.5 (range, 250-800) mg/day and the duration of use ranged from 3 weeks to 9 years. The time from discontinuation to symptom onset ranged from 1 to 10 days, with six cases arising within 2 days. Psychotic symptoms were present in eight patients.
Restarting clozapine was successful in four patients; the time to response ranged from 1 hour to 1 day. Other successful treatments involved anticholinergics (trihexyphenidyl [n=2], cyproheptadine [n=1]), other antipsychotics (zuclopenthixol, cyamemazine, levomepromazine, loxapine, risperidone), and ECT; the time to response ranged from 1 day to 6 weeks.
Unsuccessful treatments involved benzodiazepines (clorazepate, lorazepam, clonazepam, alprazolam) [n=4], benztropine (n=3), valproate acid (n=2), risperidone (n=2), olanzapine, lithium, haloperidol, levomepromazine, trihexyphenidyl, trifluoperazine, chlorprothixene, zuclopenthixol acetate, chloral hydrate, and ECT. The treatment duration ranged from one dose to 3 weeks.
Seven patients reported gastrointestinal symptoms (abdominal pain, nausea, vomiting, and diarrhoea). Six patients reported symptoms of delirium that fulfilled the DSM-5 diagnostic criteria. Four patients reported anxiety, and six patients reported diaphoresis. Three patients reported concomitant movement disorder, and one patient reported concomitant catatonia.
Serotonin Syndrome
In the four patients presenting with serotonin syndrome, one had a diagnosis of schizophrenia, one had a diagnosis of obsessive-compulsive disorder (OCD), one had both diagnoses, and one had Parkinson disease (Table 6). The patient age ranged from 44 to 69 years and the male-to- female ratio was 3:1. The mean clozapine dose was 175 (range, 50-500) mg/day and the duration of use ranged from 35 days to 10 years. The time from discontinuation to symptom onset ranged from 1 to 5 days, with two cases arising within 1 day. Psychotic symptoms were not present in any of the patients.

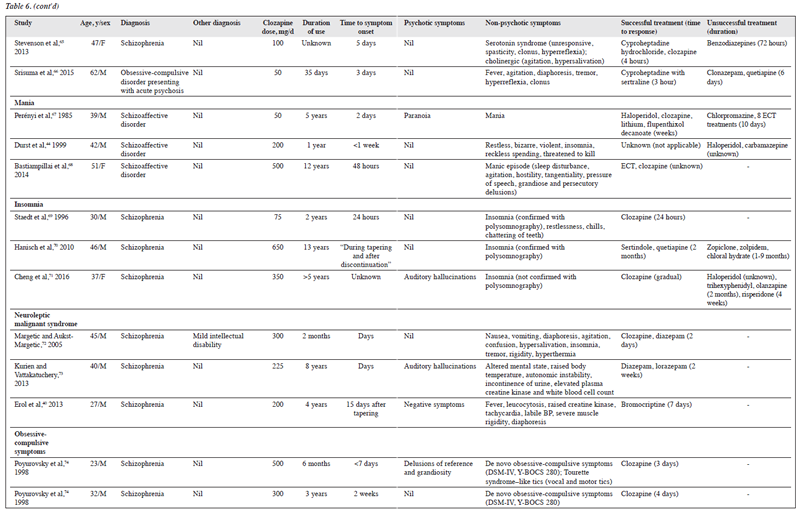
Restarting clozapine was successful in one patient; the time to response was 4 hours. Cyproheptadine treatment was successful in three patients; the time to response ranged from 3 to 24 hours. Unsuccessful treatments involved benzodiazepines (n=2) and quetiapine; the treatment duration ranged from 3 to 6 days.
The Hunter Toxicity Criteria Decision Rules were used to assess serotonin syndrome in three patients.
Mania
The three patients presenting with mania had a diagnosis of schizoaffective disorder (Table 6). The patient age ranged from 39 to 51 years and the male-to-female ratio was 2:1. The clozapine dose ranged from 50 to 500 mg/day and the duration of use ranged from 1 to 12 years. The time from discontinuation to symptom onset ranged from 2 to 7 days, with two cases arising within 2 days. Psychotic symptoms were present in one patient.
Restarting clozapine was successful in two patients. Other successful treatments involved clozapine, haloperidol, lithium, flupentixol, and ECT. The time to response ranged from 2 days to <1 week. Unsuccessful treatments involved chlorpromazine, ECT, haloperidol, and carbamazepine.
Insomnia
The three patients presenting with insomnia had a diagnosis of schizophrenia (Table 6). The patient age ranged from 30 to 46 years and the male-to-female ratio was 2:1. The clozapine dose ranged from 75 to 650 mg/day and the duration of use ranged from 2 to 13 years. Psychotic symptoms were present in only one patient.
Restarting clozapine was successful in two patients; the time to response was up to 24 hours. Other successful treatment involved quetiapine; the time to response was 2 months. Unsuccessful treatments involved zopiclone, zolpidem, and chloral hydrate.
Two patients met the DSM-5 criteria for insomnia and were confirmed by polysomnography as rebound insomnia. Sleep disturbances or insomnia were also experienced in four patients with cholinergic rebound and in one patient with NMS.
Neuroleptic Malignant Syndrome
The three patients with NMS had a diagnosis of schizophrenia (Table 6). All were men and their age ranged from 27 to 45 years. The clozapine dose ranged from 200 to 300 mg/day and the duration of use ranged from 2 months to 8 years. The time from discontinuation to symptom onset was up to 15 days. Psychotic symptoms were present in two patients. Treatment was successful in all three patients and involved clozapine, diazepam, lorazepam, and bromocriptine. The time to response ranged from 2 days to 2 weeks.
Two patients met the DSM-5 diagnostic criteria for NMS; one did not because rigidity was not documented.
Obsessive-Compulsive Symptoms
The two patients presenting with obsessive-compulsive symptoms had a diagnosis of schizophrenia (Table 6). Both were men and aged 23 and 32 years. The clozapine dose was 300 and 500 mg/day, and the duration of use was 6 months and 3 years. The time from discontinuation to symptom onset was <7 days and 2 weeks. Psychotic symptoms were present in one patient.
Restarting clozapine was successful in in both patients; the time to response was 3 and 5 days. Both patients met the DSM-IV criteria for OCD and were assessed for severity using the Yale-Brown Obsessive Compulsive Scale.
Discussion
Catatonia
Psychotic symptoms observed in patients with schizophrenia and bipolar disorder are associated with decreased expression of certain GABAergic genes.80 Clozapine induces demethylation of these promoters and promotes GABA activity, alleviating psychotic symptoms. Long-term clozapine use may result in downregulation of GABA receptors, and discontinuation of clozapine may cause GABA hypoactivity80 and catatonia.30 Thus, benzodiazepines, as GABA agonists, are the first-line treatment for catatonia.30 Intravenous lorazepam is the agent of choice when restarting clozapine is not feasible.30 When benzodiazepines are ineffective, the action of clozapine on GABA interneurons rather than the receptors themselves is the cause.80 The complexity and aetiology of catatonia secondary to clozapine withdrawal is demonstrated by cases in which treatment with lorazepam and ECT is not effective, despite these being the mainstay treatments.30
In addition to D2 antagonism, clozapine is a partial dopamine agonist at D1 and D2 receptors.80 Its inhibition of serotonin receptors increases levels of dopamine in the prefrontal cortex. Although most neuroleptics induce catatonia, clozapine is the only antipsychotic associated with catatonia after withdrawal. The hypodopaminergic state caused by clozapine withdrawal manifests as malignant catatonia (catatonic excitement, delirium, hyperthermia, and autonomic disturbance) leading to stuporous exhaustion.38 Because this condition is symptomatically indistinguishable from NMS, in which neuroleptics are traditionally withheld, there can be a delay in restarting treatment with clozapine.38 Early recognition and restarting of clozapine is recommended.80 Benzodiazepines may be used as adjuncts, and ECT can be used in cases when clozapine cannot be restarted.80 Sudden cholinergic overdrive may co-occur with catatonia after clozapine withdrawal.48 This is supported by the successful use of agents with anticholinergic properties (trihexyphenidyl, procyclidine, biperiden, and benztropine) in five patients.
Dystonia or Dyskinesia
Clozapine has a lower affinity for D2 receptors, leading to reduced incidence of EPSs, compared with other antipsychotics.7 Long-term use of clozapine can cause upregulation of D4 receptors and can cause a hyperdopaminergic state following withdrawal, which is associated with the emergence of movement disorders and psychotic features.81
Tardive dyskinesia following clozapine withdrawal can be withdrawal-emergent dyskinesia or covert dyskinesia.62 The former usually affects the limbs, neck, and trunk, whereas the latter primarily affects the oro-bucco-lingual muscles.55 Patients on long-term antipsychotic medications are at greater risk of developing withdrawal- emergent dyskinesia following drug cessation.62 In patients with known EPSs or tardive dyskinesia resolved by clozapine, discontinuation of clozapine can result in a relapse of the movement symptoms.
When other antipsychotics are administered after clozapine cessation, they antagonise presynaptic D2 receptors by reducing their inhibitory effect and allowing more dopamine to act on the supersensitive D receptors.51 This may explain the emergence of symptoms when switching from clozapine to other antipsychotics with greater D2 blockade such as risperidone.51 Dopamine does not act alone. In a case of new-onset oculogyric crisis after clozapine withdrawal, cholinergic rebound causes an imbalance in the dopamine-acetylcholine cross-talk in the basal ganglia.61 Many patients with movement symptoms also have nausea, vomiting, diaphoresis, and confusion.61
GABA dysfunction is associated with movement disorders; the overgrowth of D2 receptors in neuroleptic- induced tardive dyskinesia also supresses the activity of GABA receptors.55 This explains why benzodiazepines, which increase GABA activity, are successful in ameliorating tardive dyskinesia associated with clozapine withdrawal. In addition, the anticholinergic properties of benztropine may contribute to its success in reducing symptoms.
Cholinergic Rebound
Clozapine has strong anticholinergic properties, causing proliferation of muscarinic receptors.42 Long-term blockade of muscarinic receptors results in a rebound hypersensitivity when clozapine is withdrawn. The cholinergic effects can be classified as peripheral (nausea, vomiting, diaphoresis, rhinitis) or central, and can be mild (restlessness, insomnia) or severe (irritability, restlessness, ataxia, delirium, hallucinations).42 Administration of anticholinergic agents (trihexyphenidyl and cyproheptadine) has been effective treatment.41,42 Benztropine may not be potent enough, and a dosage of trihexyphenidyl 1 mg for every 40 mg of clozapine is recommended.41 More studies are required to establish the efficacy and dosing of anticholinergics in cases of cholinergic overdrive.
Serotonin Syndrome
Clozapine exerts its action as a serotonin antagonist, which helps alleviate the symptoms of dopamine blockade.7 Long- term clozapine use results in downregulation of 5-HT2A and 5-HT2C receptors, resulting in serotonin overstimulation following clozapine withdrawal.46
There is a classic triad of altered mental status (agitation, anxiety), neuromuscular abnormalities (tremor, clonus, rigidity, hyperreflexia, etc), and autonomic hyperactivity (hypertension, tachycardia, hyperthermia, diaphoresis). Rarely, hyperthermia and seizures can precede death in severe toxicity.82 Cyproheptadine, a 5-HT2A antagonist, is an effective treatment and supports the proposed action of clozapine on serotonin receptors.46
Mania
Mania related to clozapine withdrawal is due to the sudden upregulation of dopamine DA2 receptors upon cessation.68 Dopamine plays an important role in mood disorders; the use of dopamine agonists, including antidepressants, can trigger episodes of mania in patients with bipolar affective disorder. 83 It is important to distinguish mania from rebound psychosis upon clozapine withdrawal for determining the correct threshold for ECT treatment.
Insomnia
Increased central levels of GABA following clozapine administration have been shown in an animal study.69 Many patients with schizophrenia report increased sleep latency, reduced sleep efficiency, and reduced total sleep time, which are resolved with clozapine treatment. Thus, the sudden reduction of GABA receptor stimulation after clozapine withdrawal may cause rebound insomnia.69
Neuroleptic Malignant Syndrome
NMS usually occurs during antipsychotic use; it can emerge after antipsychotic discontinuation, owing to imbalances in the dopaminergic system rather than dopamine blockade alone.84 Clozapine antagonises both dopaminergic and cholinergic receptors; cessation reduces dopamine blockade (despite removing the protective anticholinergic effects) and potentially precipitates NMS.84
Obsessive-Compulsive Symptoms
Dose-dependent clozapine-induced OCD symptoms are likely due to the antagonistic effect of clozapine on serotonin receptors.74 Clozapine also blocks certain dopamine receptors, preventing movement disorder symptoms. In a patient with concurrent OCD and Tourette syndrome, an imbalance between the serotonin and dopamine systems may result in OCD symptoms after sudden clozapine cessation.
Clinical Significance
Non-psychosis symptoms after clozapine withdrawal pose significant risks. Clinicians should educate patients and carers about the possible withdrawal symptoms to facilitate early detection and treatment. Clozapine dose reduction should be gradual, and patients should be closely monitored for withdrawal symptoms. In patients with repeated non- adherence to clozapine treatment or a history of withdrawal symptoms, alternative antipsychotics should be considered, although restarting clozapine produces the fastest and most effective resolution of withdrawal symptoms.
Limitations
There are several limitations to this systematic review. Case reports / series are susceptible to over-interpretation, publication bias, and recall bias. Non-psychosis symptoms after clozapine withdrawal may be underdiagnosed and underreported. Many case reports did not accurately document timing such as the time from clozapine discontinuation to symptom onset and the time to response after treatment. There is no standardised classification system for clozapine withdrawal symptoms, and many case reports did not use validated diagnostic criteria or severity scales. Consequently, the symptoms described may not be comparable and reproducible. There is also the possibility of other causative or confounding factors. For example, clozapine withdrawal symptoms are less evident in cross- titration studies. Generalisation of findings in clinical practice may be unreliable, particularly for rarer symptoms. A meta-analysis was not possible given the poor quality of the data.
Conclusion
Studies of non-psychosis symptoms following clozapine withdrawal are limited. Clinicians should monitor for both psychosis and non-psychosis symptoms in patients undergoing clozapine withdrawal to enable their early detection and treatment. Restarting clozapine may be the most appropriate treatment, but prompt use of alternative pharmacotherapies may be considered in some cases. Further studies are warranted to determine the risks, incidence, prevalence, and pathophysiology of clozapine withdrawal, as well as safe and effective treatments for clozapine withdrawal symptoms.
Contributors
All authors designed the study, acquired the data, analysed the data, drafted the manuscript, and critically revised the manuscript for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, SKW Chan was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability
All data generated or analysed during the present study are available from the corresponding author on reasonable request.
References
- Baig AI, Bazargan-Hejazi S, Ebrahim G, Rodriguez-Lara J. Clozapine prescribing barriers in the management of treatment-resistant schizophrenia: a systematic review. Medicine 2021;100:e27694. Crossref
- Dilsaver SC, Greden JF. Antidepressant withdrawal phenomena. Biol Psychiatry 1984;19:237-56.
- Chouinard G. Issues in the clinical use of benzodiazepines: potency, withdrawal, and rebound. J Clin Psychiatry 2004;65(Suppl 5):7-12.
- Moncrieff J. Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse. Acta Psychiatr Scand 2006;114:3-13. Crossref
- Parsa MA, al-Lahham YH, Ramirez LF, Meltzer HY. Prolonged psychotic relapse after abrupt clozapine withdrawal. J Clin Psychopharmacol 1993;13:154-5. Crossref
- Chouinard G, Chouinard VA. New classification of selective serotonin reuptake inhibitor withdrawal. Psychother Psychosom 2015;84:63-71. Crossref
- Naheed M, Green B. Focus on clozapine. Curr Med Res Opin 2001;17:223-9. Crossref
- Verghese C, DeLeon J, Nair C, Simpson GM. Clozapine withdrawal effects and receptor profiles of typical and atypical neuroleptics. Biol Psychiatry 1996;39:135-8. Crossref
- Blackman G, Oloyede E. Clozapine discontinuation withdrawal symptoms in schizophrenia. Ther Adv Psychopharmacol 2021;11:20451253211032053. Crossref
- Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. Crossref
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. Crossref
- Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Glob Adv Health Med 2013;2:38-43. Crossref
- Lee JW, Robertson S. Clozapine withdrawal catatonia and neuroleptic malignant syndrome: a case report. Ann Clin Psychiatry 1997;9:165-9.Crossref
- Yeh AW, Lee JW, Cheng TC, Wen JK, Chen WH. Clozapine withdrawal catatonia associated with cholinergic and serotonergic rebound hyperactivity: a case report. Clin Neuropharmacol 2004;27:216-8. Crossref
- Kalogeropoulou A, Leotsakou C, Fotara I, et al. Catatonia after abrupt discontinuation of chronic clozapine treatment. Eur Psychiatry 2007;22(S1):S120-1. Crossref
- Bastiampillai T, Forooziya F, Dhillon R. Clozapine-withdrawal catatonia. Aust N Z J Psychiatry 2009;43:283-4.
- Thanasan S, Jambunathan ST. Clozapine withdrawal catatonia or lethal catatonia in a schizoaffective patient with a family history of Parkinson’s disease. Afr J Psychiatry (Johannesbg) 2010;13:402-4.
- Wadekar M, Syed S. Clozapine-withdrawal catatonia. Psychosomatics 2010;51:355-e2. Crossref
- Dhillon R, Bastiampillai T, Tee K, Vanlint A. Clozapine and associated QTc prolongation. Aust N Z J Psychiatry 2011;45:1098-9. Crossref
- Kanagasundram S, Chengappa KNR. Meningoencephalitis or clozapine withdrawal catatonia or both in a patient with schizophrenia. Acta Neuropsychiatrica 2011;23:85-7. Crossref
- Kumar S, Sur S, Singh A. Catatonia following abrupt stoppage of clozapine. Aust N Z J Psychiatry 2011;45:499. Crossref
- Cerit C, Tuzun B, Akpinar E, Sahan E. Clozapine withdrawal catatonia refractory to ECT: a case report. Bull Clin Psychopharmacol 2012;22:275-7. Crossref
- Wang BZ, Gupta A, Bastiampillai T, Sani F. Recurrent clozapine and lorazepam withdrawal psychosis with catatonia. Aust N Z J Psychiatry 2012;46:795-6. Crossref
- KochA, Reich K, Wielopolski J, et al. Catatonic dilemma in a 33-year-old woman: a discussion. Case Rep Psychiatry 2013;2013:542303. Crossref
- Ariyasinghe D, Abeyasinghe R. Catatonia following abrupt discontinuation of clozapine. Sri Lanka J Psychiatry 2014;5:27-8.Crossref
- Saddawi-Konefka D, Berg SM, Nejad SH, Bittner EA. Catatonia in the ICU: an important and underdiagnosed cause of altered mental status: a case series and review of the literature. Crit Care Med 2014;42:e234-41.Crossref
- Nasr Y, Ganapathy R. Treatment resistant catatonia secondary to clozapine withdrawal. Progress Neurol Psychiatry 2015;19:17-9.Crossref
- Shahrour T, Siddiq M, Ghalib S, Alsaadi T. Severe relapsing clozapine- withdrawal catatonia. Case Rep Psychiatry 2015;2015:606853. Crossref
- Koychev I, Hadjiphilippou S, Lynch J, Whelan P, MacCabe J. Sudden- onset catatonia following clozapine withdrawal: a case report. J Clin Psychiatry 2016;77:e899. Crossref
- Bilbily J, McCollum B, de Leon J. Catatonia secondary to sudden clozapine withdrawal: a case with three repeated episodes and a literature review. Case Rep Psychiatry 2017;2017:2402731. Crossref
- Ingole A, Bastiampillai T, Tibrewal P. Clozapine withdrawal catatonia, psychosis and associated neuroleptic malignant syndrome. Asian J Psychiatr 2017;30:96-7. Crossref
- Poudwal YJB, Shah B. Clozapine withdrawal in catatonia: a case report. Indian J Ment Health 2018;5:373-5.
- Boazak M, Cotes RO, Potvin H, Decker AM, Schwartz AC. Catatonia due to clozapine withdrawal: a case report and literature review. Psychosomatics 2019;60:421-7. Crossref
- Kapulsky L, Greiner MG, Daniels JE, Gordon-Elliott JS. Clozapine discontinuation and malignant catatonia: a case report. Psychosomatics 2019;60:75-9. Crossref
- McGuire E, Reilly M. Clozaril withdrawal induced catatonia. Ir Med J 2019;112:938.
- Brailey J, Bastiampillai T. Clozapine withdrawal malignant catatonia in a medical intensive care unit setting. Asian J Psychiatr 2020;52:102043. Crossref
- Lucchelli JP, Kourakou S, Hasler G, Hilal R. Clozapine withdrawal catatonia in a young schizophrenic man. Encephale 2021;47:396-8.Crossref
- Belteczki Z, Ujvari J, Dome P. Clozapine withdrawal-induced malignant catatonia or neuroleptic malignant syndrome: a case report and a brief review of the literature. Clin Neuropharmacol 2021;44:148-53.Crossref
- Hung YY, Yang PS, Huang TL. Clozapine in schizophrenia patients with recurrent catatonia: report of two cases. Psychiatry Clin Neurosci 2006;60:256-8. Crossref
- Erol A, Putgül G, Sert E, Mete L. Clozapine-associated neuroleptic malignant syndrome followed by catatonia: a case report [in Turkish]. Turk Psikiyatri Derg 2013;24:140-4. Crossref
- de Leon J, Stanilla JK, White AO, Simpson GM. Anticholinergics to treat clozapine withdrawal. J Clin Psychiatry 1994;55:119-20.
- Stanilla JK, de Leon J, Simpson GM. Clozapine withdrawal resulting in delirium with psychosis: a report of three cases. J Clin Psychiatry 1997;58:252-5. Crossref
- Delassus-Guenault N, Jegouzo A, Odou P, et al. Clozapine-olanzapine: a potentially dangerous switch. A report of two cases. J Clin Pharm Ther 1999;24:191-5. Crossref
- Durst R, Teitelbaum A, Katz G, Knobler HY. Withdrawal from clozapine: the “rebound phenomenon”. Isr J Psychiatry Relat Sci 1999;36:122-8.
- Berecz R, Glaub T, Kellermann M, de la Rubia A, Llerena A, Degrell I. Clozapine withdrawal symptoms after change to sertindole in a schizophrenic patient. Pharmacopsychiatry 2000;33:42-4. Crossref
- Malhotra S, Franco K, Tomford JW, Iqbal R. Polyserositis, acute withdrawal, and relapse after abrupt clozapine discontinuation. Psychosomatics 2002;43:418-20. Crossref
- Modak A, Åhlin A. The treatment of clozapine-withdrawal delirium with electroconvulsive therapy. Case Rep Psychiatry 2017;2017:1783545. Crossref
- Galova A, Berney P, Desmeules J, Sergentanis I, Besson M. A case report of cholinergic rebound syndrome following abrupt low-dose clozapine discontinuation in a patient with type I bipolar affective disorder. BMC Psychiatry 2019;19:73. Crossref
- Palkar P, Garces E, Chavali S, Zubair AS, Hashmi S. Rapid-onset psychosis and cholinergic rebound after abrupt discontinuation of clozapine. Psychiatr Annals 2021;51:99-100. Crossref
- Alphs LD, Lee HS. Comparison of withdrawal of typical and atypical antipsychotic drugs: a case study. J Clin Psychiatry 1991;52:346-8.
- Dickson R, Williams R, Dalby JT. Dystonic reaction and relapse with clozapine discontinuation and risperidone initiation. Can J Psychiatry 1994;39:184. Crossref
- Radford JM, Brown TM, Borison RL. Unexpected dystonia while changing from clozapine to risperidone. J Clin Psychopharmacol 1995;15:225-6. Crossref
- Songer DA, Schulte HM. Withdrawal dyskinesia after abrupt cessation of clozapine and benztropine. J Clin Psychiatry 1996;57:40.
- Bobba R. Severe extrapyramidal side effects when discontinuing clozapine and starting haloperidol. Can J Psychiatry 1997;42:530. Crossref
- Ahmed S, Chengappa KN, Naidu VR, Baker RW, Parepally H, Schooler NR. Clozapine withdrawal-emergent dystonias and dyskinesias: a case series. J Clin Psychiatry 1998;59:472-7. Crossref
- Yovtcheva SP, Stanley-Tilt C, Moles JK. Reemergence of tardive dyskinesia after discontinuation of clozapine treatment. Schizophr Res 2000;46:107-9. Crossref
- Uzun O, Cansever A, Ozsahin A. A case of relapsed tardive dyskinesia due to clozapine dose reduction. Int Clin Psychopharmacol 2001;16:369-71. Crossref
- Mendhekar DN, Duggal HS. Isolated oculogyric crisis on clozapine discontinuation. J Neuropsychiatry Clin Neurosci 2006;18:424-5.Crossref
- Shrivastava M, Solanke B, Dakhale G, Somani A, Waradkar P. Relapse of tardive dyskinesia due to reduction in clozapine dose. Indian J Pharmacol 2009;41:201-2. Crossref
- Sarma S, Chetia D, Raha B, Agarwal G. Clozapine withdrawal emergent dystonia, oculogyric crisis and rebound psychosis in a single patient. Ther Adv Psychopharmacol 2016;6:145-6. Crossref
- Kar SK, Kishor K. Quetiapine treatment of occulogyric crisis following abrupt clozapine discontinuation. Aust N Z J Psychiatry 2016;50:183-4.Crossref
- Berry AJ. Acute dyskinesia in a patient with schizophrenia. BMJ Case Reports 2018;11:e225251. Crossref
- Zerjav-Lacombe S, Dewan V. Possible serotonin syndrome associated with clomipramine after withdrawal of clozapine. Ann Pharmacother 2001;35:180-2. Crossref
- Zesiewicz TA, Borra S, Hauser RA. Clozapine withdrawal symptoms in a Parkinson’s disease patient. Mov Disord 2002;17:1365-7. Crossref
- Stevenson E, Schembri F, Green DM, Burns JD. Serotonin syndrome associated with clozapine withdrawal. JAMA Neurology 2013;70:1054-5. Crossref
- Srisuma S, Hoyte CO, Wongvisavakorn S, Wanaukul W. Serotonin syndrome precipitated by sertraline and discontinuation of clozapine. Clin Toxicol (Phila) 2015;53:840-1. Crossref
- Perényi A, Kuncz E, Bagdy G. Early relapse after sudden withdrawal or dose reduction of clozapine. Psychopharmacology (Berl) 1985;86:244. Crossref
- Bastiampillai T, Juneja V, Nance MJ. Clozapine rebound mania. Aust N Z J Psychiatry 2014;48:98-9. Crossref
- Staedt J, Stoppe G, Hajak G, Ruther E. Rebound insomnia after abrupt clozapine withdrawal. Eur Arch Psychiatry Clin Neurosci 1996;246:79-82. Crossref
- Hanisch F, Friedemann J, Pillmann F. Combined treatment with quetiapine and sertindole in therapy refractory insomnia after clozapine discontinuation. J Psychopharmacol 2010;24:1725-6. Crossref
- Cheng M, Gu H, Zheng L, Wang H, Zhong Z, Wen S. Neuroleptic malignant syndrome and subsequent clozapine-withdrawal effects in a patient with refractory schizophrenia. Neuropsychiatr Dis Treat 2016;12:695-7. Crossref
- Margetić B, Aukst-Margetić B. Neuroleptic malignant syndrome and clozapine withdrawal at the same time? Prog Neuropsychopharmacol Biol Psychiatry 2005;29:145-7. Crossref
- Kurien R, Vattakatuchery JJ. Psychotropic discontinuation leading to an NMS-like condition. Progress Neurol Psychiatry 2013;17:8-10. Crossref
- Poyurovsky M, Bergman Y, Shoshani D, Schneidman M, Weizman A. Emergence of obsessive--compulsive symptoms and tics during clozapine withdrawal. Clin Neuropharmacol 1998;21:97-100.
- Simpson GM, Lee JH, Shrivastava RK. Clozapine in tardive dyskinesia. Psychopharmacology (Berl) 1978;56:75-80. Crossref
- Meltzer HY, Lee MA, Ranjan R, Mason EA, Cola PA. Relapse following clozapine withdrawal: effect of neuroleptic drugs and cyproheptadine. Psychopharmacology (Berl) 1996;124:176-87. Crossref
- Shiovitz TM, Welke TL, Tigel PD, et al. Cholinergic rebound and rapid onset psychosis following abrupt clozapine withdrawal. Schizophr Bull 1996;22:591-5. Crossref
- Seppala N, Kovio C, Leinonen E. Effect of anticholinergics in preventing acute deterioration in patients undergoing abrupt clozapine withdrawal. CNS Drugs 2005;19:1049-55. Crossref
- Tollefson GD, Dellva MA, Mattler CA, Kane JM, Wirshing DA, Kinon BJ. Controlled, double-blind investigation of the clozapine discontinuation symptoms with conversion to either olanzapine or placebo. The Collaborative Crossover Study Group. J Clin Psychopharmacol 1999;19:435-43. Crossref
- Lander M, Bastiampillai T, Sareen J. Review of withdrawal catatonia: what does this reveal about clozapine? Transl Psychiatry 2018;8:139. Crossref
- Hazari N, Kate N, Grover S. Clozapine and tardive movement disorders: a review. Asian J Psychiatr 2013;6:439-51. Crossref
- Prakash S, Rathore C, Rana K, Prakash A. Fatal serotonin syndrome: a systematic review of 56 cases in the literature. Clin Toxicol (Phila) 2021;59:89-100. Crossref
- Manji HK, Quiroz JA, Payne JL, et al. The underlying neurobiology of bipolar disorder. World Psychiatry 2003;2:136-46.
- Spivak B, Gonen N, Mester R, Averbuch E, Adlersberg S, Weizman A. Neuroleptic malignant syndrome associated with abrupt withdrawal of anticholinergic agents. Int Clin Psychopharmacol 1996;11:207-8.Crossref