Hong Kong Journal of Psychiatry (1997) 7 (2) 26-35
SPECIAL TOPIC: SCHIZOPHRENIA
Summary
Recent studies have consistently shown that behavioural family therapy (BFT) is effective in reducing the replace rate of chronic schizophrenic patients by modifying the social environmental in which patients live (Liberman et al, 1987). By changing the attitudes, stress level, teaching the patients and their families in skills such as problem solving and communication, BFT aims at improving the coping abilities and the quality of life of all members of the family. The purpose of this study is to investigate the applicability and cost- effectiveness of BFT in the local context. 63 families have been randomly assigned into the behavioural family therapy group and the controlled group. The six-month preliminary result indicated that BFT increase family members’ knowledge about the illness and maintained patients’ level of psychosocial functioning.
Keywords: family management, cost-effectiveness, schizophrenia, community based rehabilitation
INTRODUCTION
With deinstitutionalisation of mental hospitals, family members have assumed the burden of care for up to 70% of the discharged chronic mental patients (Goldman, 1982). In order to assist these carers, many models of family therapies have been developed such as systems-oriented therapies (Langsley, 1971, Haley, 1980, Madanes, 1982, Selvini-Palazzoli, 1989), family crisis therapy (Goldstein, 1978, Glick, 1985), psychoeducation for family groups (Leff, 1982,1989, Hogarty, 1986, 1991, McFarlane, 1995) and behavioural family management (Falloon, 1982, 1985, Tarrier & Barrowclough, 1988, 1989, Randolph, 1994). It should be noted that the differences between these models are not really distinct and quite often a mixture of each is incorporated in the family therapy sessions.
However, the above studies were carried out in western countries with well-trained staff and resources, and may not be applicable or practicable in other cultures. For the Chinese patients, there may be a different pattern of communication between the family members (Hsu, 1995) where mutual discussion and open expression of emotion do not take place easily, and there may be practical difficulties to generalize abstract concepts into real life situations (Hsu & Tseng, 1991), not to mention the hierarchy of power within the family. In Hong Kong, which is quite westernized, the traditional extended structure has been replaced by still relatively stable nuclear family structure, and family members are still fairly receptive of chronic schizophrenic patients, though often with quite a lot of suffering and psychological pain. Therefore, family therapy is indicated for these carers of chronic mental patients. However, therapy in this area has been eclectic and piecemeal, and there has not been any formal testing of these treatment models for schizophrenic patients in Hong Kong.
The purpose of this study, therefore, is to compare the cost-effectiveness of a form of behavioural family therapy for a group of schizophrenic patients with that of conventional treatment.
METHODOLOGY
This is a longitudinal prospective controlled study to compare the cost-effectiveness of a community behavioral family management service to that of the conventional clinic-based management for chronic schizophrenic patients who are high consumers of psychiatric rehabilitation. This study covered a period of one year involving out-patients of the University Psychiatric Unit of the University of Hong Kong. All the investigators are experienced clinicians in the field of rehabilitation.
SELECTION OF SUBJECTS
Subjects of either sex who were in the age range of 18 to 62 years with the diagnosis of schizophrenia (according to DSM-III-R) attending the out-patient psychiatric clinic were screened. Other criteria for selection were included: (I) chronicity with duration of illness of 2 years or over; (2) frequent follow-up of at least once a month; and (3) having regular face-to-face contact of 4 hours or more per week with a close relative for at least two months prior to the admission of the study. Patients who had definite evidence of drug abuse or mental retardation were excluded.
Relatives of the subjects were then approached and invited to participate in the study. Consents to participate in the study were obtained in both the subjects and their relatives. 63 such families were thus recruited and were randomly allocated to the experimental and the control groups. Two weeks later, 8 families withdrew from the programme, leaving 28 subjects in the experimental group and 27 subjects in the control group.
For the experimental group, a series of six group behavioral family therapy sessions at two weekly interval were provided by a family therapist, followed by a roughly monthly individual family therapy for one year by the family therapist.
For the control group, apart from receiving conventional care (which can include ordinary medical educational information), no behavioral therapy or family therapy was given for the same year.
DESIGN
The behavioral family management (BFM) started with a home visit to enable the therapist to engage the family and to build up the rapport with the members in the home environment; and to obtain some understanding of the living home environment.
The one-year treatment program consisted of two parts:
(I) the Group Behavioral Family Management therapy (GBFM), and (2) supportive Individual Behavioural Family Management (IBFM)
Group Behavioral Family Management (GBFM)
The subjects were divided into small groups of 5 to 8 families, according to the time of recruitment and their convenience to come together for the group sessions. Both the patient and his relative were invited to join the group. In case of the relative declining to join the group, the patient was still eligible for participation in the group sessions.
Each group comprised patients of different sex, age group, background and level of functioning. The group consisted of six sessions of an hour and a half duration and was held biweekly (with the exception of one group which was run weekly). These sessions were conducted by a family therapist of counseling background and assisted by an assistant (who was a graduate in psychology).
The key contents of the group consisted of psycho-education, communication skills and problem-solving skills. The techniques in running the group include discussion, modeling, role-play, feedback, reinforcement and home-work assignments. Psychoeducation was provided through printed information on schizophrenia, the importance of regular drug compliance was stressed and strategies in preventing relapse were discussed. Education was offered first to instill hope in relatives, so that they would feel more optimistic about the future (Berkowitz, 1984). In order to help the families communicate effectively and enhance the subjects' confidence in interacting with other people, communication skills such as active listening, expressing positive feeling, making a positive request, expressing negative feeling, compromising and time-out were discussed and practiced in the third and fourth sessions. In the last two sessions, systemic problem solving training, which included defining a problem, brainstorming, evaluating alternatives, selecting an optimal solution, planning implementation and review of the solution, was rendered. The family was encouraged to solve an individual member's problem together at a family meeting so as to reduce stress and improve family relationship. Finally, behavioral strategies to handle residual symptoms were explored.
Individual Behavioural Family Management (IBFM)
Upon completion of the GBFM, the therapist conducted monthly sessions for the families in the subsequent nine months, reinforcing what they had learnt in the group, helping relatives in patient management and assisting the families to resolve family conflicts such as overinvolvement, overprotectiveness and marital problems. Regular drug compliance was emphasized and emotional support was given to the families. High EE (expressed emotion) relatives were helped to assume a lower EE role (Leff, 1982), but if the attempt was unsuccessful, the subject was advised to decrease the face-to-face contact with the relative, as Bebbington and Kuipers (1994) confirmed that the association with relapse was stronger when high EE relatives were in close contact with patients. Referral was made to social agency or other organization if the subject required such additional services. Moreover, the therapist encouraged the subjects to set realistic goals and to become more independent.
The families had the therapist's paging number which could be reached in case of an urgent need. In such a way, the therapist could offer immediate assistance in resolving any family crisis.
Conventional Care
Conventional treatment and care (including day hospital treatment) were still provided for the experimental and control subjects, usually by the outpatient staff including psychiatrists,
ASSESSMENT INSTRUMENTS
Socio-demographic data were collected for the two groups. Their clinical status, social functioning, change in the quality of life, the relatives' acceptance and burden were assessed, using the following instruments:
1. Clinical symptomatology and relapse
The Brief Psychiatric Rating Scale or BPRS (Overall & Gorham, 1962) was employed to measure subjects' psychopathology and degree of remission or exacerbation. Rating of 5 (moderately severe) or above indicates an exacerbation. Individual items are summed to produce 4 subscale scores (schizophrenic thought, anxious depression, hostility and suspiciousness, as well as emotional withdrawal and retardation) and a total score. The BPRS was administered at the beginning, at six months and at the end of the program. The rater was blind to the treatment condition.
Clinical improvement was also evaluated through information about the frequency and duration of hospitalization, symptom exacerbation (mild relapse requiring no hospitalization), suicide rate and criminal offence etc. in the study period.
2. Knowledge about schizophrenia
The Knowledge About Schizophrenia Interview (KASI) (Barrowclough et al, 1987) is a semi-structured interview in which relatives are asked about diagnosis, symptomatology, aetiology, medication, course, prognosis and management of schizophrenia. Ratings are intended to assess "not just the presence of information about schizophrenia, but the effects of that information on the relative's behavior" and poor knowledge about schizophrenia is associated with greater levels of criticism of the patient by relatives, This instrument is sensitive to change from brief educational interventions. The interview was conducted at the beginning of the program to the relative who participated at the GBFM, and the same interview was repeated to the same relative at six months and at the end of the study.
3. Disability assessment
The WHO Psychiatric Disability Assessment Schedule (DAS) (W.H.O., 1989) was used to measure the patient's social functioning and adjustment. The patient's dysfunctional overall behavior, dysfunction in social roles, behavior in hospitals, assets, liabilities and current total social adjustment are measured. The DAS was completed by the therapist at the beginning, at 6 months and at the end of the program. Data on the employment situation and .their financial assistance were also evaluated.
4. Personal satisfaction with service
The Client Satisfaction Questionnaire (CSQ) (Larsen, 1979) is considered to be a useful measure of general satisfaction with services. For this study, the CSQ was modified with more detailed questions suitable for the Chinese culture. Modified from the CSQ, the Relative Satisfaction Questionnaire was also designed and similar questions were posed. Experimental subjects and relatives were asked to complete the questionnaires respectively one month after the GBFM and at the end of the program.
RESULTS
Altogether 63 subjects were initially recruited for the study, but subsequently 8 subjects withdrew for various reasons (time, convenience, etc.) from the experimental group during the orientation stage. Therefore, the experimental group was left with 28 families while the control group had 27. A comparison between the two groups over the various socio-demographic data at the initial stage was tabled below (Table 1).
It was noted that there were no significant differences between the two groups as regard age, sex, marital status, chronicity of the illness, and employment status except for education level. The mean number of years of education is 10.14 for the experimental group and 8.00 for the control group (t = 27, p<.03). Nevertheless, the differences in years of schooling was not of much meaning because the number of subjects which had secondary education are similar in both group, and data analysis using chi-square showed no statistical significance between the two groups (X.2 = 2.39, p<.1, NS).
Psychopathology
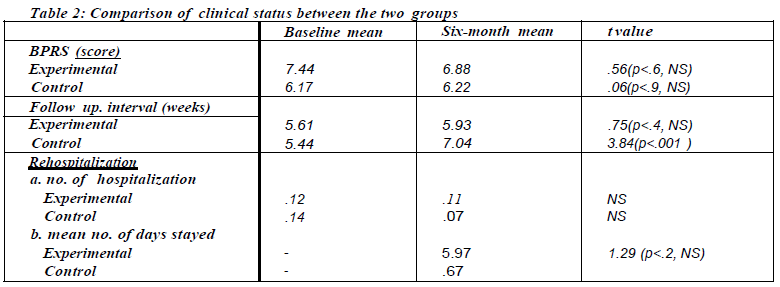
A comparison between the two groups at the initial and the interim stages was presented in Table 2.
The prolonged interval at out-patient clinic follow-up by the control group was interesting, and may in fact reflect the poor compliance to regular treatment, compared to the experimental group. It was noted that there was some improvement in the BPRS score of the experimental group, but not of statistical significance. The number of patients suffering from a relapse was similar in both groups (three for experimental and two for control); but they were again not of statistical significance. Interestingly, for the experimental group, there was a prolonged stay in hospital for two patients. This was mainly because they were admitted into the hospital for drug trial (Clozapine) which required at least 18 weeks stay (for weekly blood monitoring) in hospital disregarding mental state. Surprisingly, the control group on the whole required less out-patient attendance than the experimental group.
There was no reported death in either group, but there was one patient in the experimental group who was charged for common assault (under provocation by a customer at a gas station), but this single incident of criminal behaviour did not make any statistical difference compared to the control group.
Social functioning
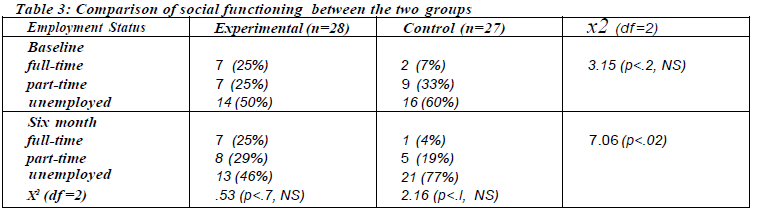
This was mainly reflected by the employment status and the level of disability (DAS) of the subjects. Employment means working for at least one month in the job. The experimental group started off with a greater proportion of employed subjects but it did not reach statistical significance when compared with the control group. At the six-month interval, it was obvious that the experimental group maintained its level of employment, whereas the control group deteriorated with more unemployment (Table 3).
Concerning the income gained by both groups, there was no statistical significance change between the two groups, despite a numerical difference in the amount of money received from the social assistance (US$500 for the experimental group versus US$1,400 for the control group).
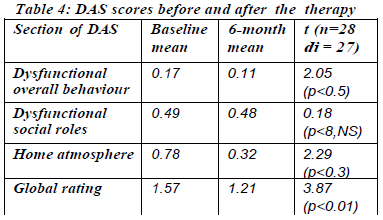
As regard social disability, there were significant differences in the area of ysfunctional behaviour' (t=2.05, p<0.5) and one atmosphere' (t=2.29, p<0.3). The findings suggested that the subjects could have gained some improvement in self-care and social contact, which were consistent with the direct observation of lowered emotional expression of family members. On the other hand the improvement in the score of social role was not of significance. The overall social adjustment was reflected on the score of global rating (t=3.87, p<.001) which increased significantly as a result of the intervention.
Service Satisfaction
At the end of the group therapy sessions, the patients and their relatives were all given a questionnaire as regard satisfaction of service. Of all the responders (23 patients and 15 relatives), 95.6% of the patients and 86.6% of the relatives were satisfied with the service. However, only half of the patients (56.55) and the relatives (53.3%) felt that the programmes provided met most of their needs, which was not unexpected as the needs of the subjects and relatives could be quite varied and individualized.
As regard the various components of the therapy, 73.9% of the patients and 53.3% of the relatives were certain that there was an increase in knowledge about schizophrenia. This was comparable with the findings in the KASI scores between the two groups. As regard improvement in communication and mutual understanding between patients and relatives, about two-thirds (95.6% of patients and 93.4% of relatives) felt the therapy had assisted them to some extent. Finally, 96.0% of the patients and 86.7% felt the therapy had helped the patients in solving problems in their lives to a more or less extent, though only one-fifth of the group felt its assistance was very significant. Though there could be an overrating of the results to the positive side by the respondents, the questionnaire did convey that there was at least no significant negative results from the family therapy programme. This was also confirmed by the active participants and relatively high attendance rates (12 attended every session, 9 missed one session and the 7 missed two sessions), compared with other studies such as Leff (1989).
Knowledge about schizophrenia
There is an overall improvement in the knowledge about schizophrenia as reflected by the KASI. As shown in table 5, the scores for section 1 (diagnosis), 2 (symptomatology) and 5 (course and prognosis) increased significantly, as did the total score. However, the education intervention seemed to have little or no effect on the knowledge of aetiology, medication and management of the illness. Despite a positive correlation (r=.4, p<.05) between the relative education level and the total score, no significant differences were found when relatives were grouped according to the chronicity of the patient illness and the number of hospitalizations.
Costs
It is really difficult to calculate the cost-benefits at this juncture. Needless to say, the study had to employ a therapist and research work had to be done. Taking aside those areas which were related to the research, the following items could be calculated:
i. The costs of employing the worker (half-time), but 50% of her work was concerned with research and production of the training programme. Therefore, the actual costs involved should be 25% of the salary which was 25% x US$2,500 per month x 6 months = US3,750
ii. The costs of programme expenditure including traveling expenses, refreshment for group activities, mailing and photocopies were US$200.
iii. The costs due to increased hospitalisation was not calculated because the difference was not of statistical significance and could be due to chance alone.
iv. The savings in costs should be calculated as the difference in employment rate was of statistical significance, and taking an average working salary as US$1,000 per month, the savings in costs was roughly estimated as US$ 18,000 (considering a 6- person differences between the two groups). Therefore the overall rough estimate of the costs of the study was calculated as US$ (3,750 + 200 -18,000) or a net gain of around US$14,000. However, further refinement of the calculation should be taken before a definite conclusion can be made.
DISCUSSION
This is only an interim report of 6 months, and full report could come out later. It had been said that social rehabilitation process did take time to show its effects, and one previous local study on aftercare services did show a positive result only after 18 months of service (Mak, 1996).
Nevertheless, the present study showed that Behavioral Family Therapy could be well accepted by the Chinese schizophrenic patients and their families, at least in Hong Kong. This is compatible with the impression that Chinese patients preferred more directive psychotherapy Uke BFTM than psychoanalysis or self-reflective therapies.
However, the present family therapy schedule is a combination of group and individual therapy. Each mode of family therapy has its own merits. The group setting {which was clinic based) allows mutual support and encouragement, with practical advice from other group members (Mcfarlane, 1995). On the other hand, individual family therapy (home based) often encourages personal or idiosyncratic issues to be discussed, and the therapist's advice is more specific towards the confiding problem. Indeed, Leff et al (1989, 1990) found no difference between home or clinic based family therapy. As regard the type of therapy, Tarrier et al (1988, 1989) found no difference between symbolic and enactive family therapy, and Zastawny et al (1992) found behavioural and supportive family therapy having similar results.
Although the change in clinical conditions had not been too remarkable at the interim period, it was compatible with a previous study on similar chronic schizophrenic patients of an aftercare worker which did not show obvious cllnical changes during the first year (Mak, 1992). That the BPRS changes were not of significance was not surprising, given that the baseline score was not high and small changes would not be detected (ceiling effect). Maybe, instruments testing for negative symptoms could be more useful. Besides, there could be some confounding variables such as drug compliance, change of therapy, etc., which would have more effects on psychopathologies, but these factors could not be analysed in view of the small sample size, and a multi-centre trial could throw light on this.
As regard the relapse rate, there were reports of decreased hospitalizations (Fallon et. al., 1982, 1985) which was the main bull, of money saved. However, this was not the case in the present study, there was an apparent increase in hospital stay in the experimental group, though there was no statistical significance in the number of rehospitalisatons, not to mention that rehospitalisation is not a good indicator of psychotic exacerbation (Randslegh et al, 1994). Furthermore, the relapsed patients in the experimental group were given rather prolonged hospital stay (for quite unique unforseeable reason of drug bial), and this would upset the cost-benefit calculation in the long run. Fortunately, there were no reported death in either group, otherwise the costs of such loss would be difficult to calculate.
What was most heartening was the improvement in employment. While there was a slight increase in employment in the experimental group, there was a more drastic drop of employment in the control group. Similar results of this nature was found in a previous study in Hong Kong (Mak, 1996) which proved that active rehabilitation could maintain work, at least in Hong Kong, where the keen competition and demand in the job market was detrimental to the unsupported mental patients. Besides, it was possible that group pressure and individual advice to the patient could assist in job-seeking behaviour.
As regard psychiatric disability, The improvement in this area was not surprising and this was a primary objective of the family therapy. However social role dysfunction still persisted and perhaps time is a limiting factor. Another short-corning of DAS was that certain areas of the schedule such as marital, sex, and parental roles were not applicable for this group of subjects who were mostly unmarried.
Furthermore, the group treasured the knowledge in schizophrenia which had a direct bearing on the handling of schizophrenic patients (Barrowclough et al, 1987). Indeed this was an important element in most psychoeducational family therapy therapies (Schooler, 1995). Hopefully, this improved knowledge could induce a better quality of life (QOL) for the patients and their carers. However, this QOL had not been systematically explored in the present study and would merit attention in future studies.
On the other hand, the satisfaction feedback from the participants should not be taken too optimistically, as those who did attend the group were quite enthusiastic to know more and perhaps to change, and they might cognitively incline to rate the questionnaire with a more favourable or positive attitude. However, it is difficult to compare the results with the control group who did not receive any particular or placebo service.
As regard the economic balance, the analysis at 6 months appeared favourable, but the results should be taken with caution. As mentioned above, the savings from decreased hospitallsations was not proven, but the increase in earnings should merit further detailed attention. It was difficult to quantify the increase in knowledge and service satisfaction into monetary term, though one way is to ask the service recipients how much they are willing to pay for such service. It is prudent to wait for the study to complete before generalization could be made.
If the sample size was big enough, one could further analyze the differential responses to different socio-economic or clinical variables e.g. sex, chronicity (Goldstein, 1978), symptom, symptomatology (Mcfarlane, 1995), etc. Furthermore, other therapeutic measures especially social skills learning (Hogarty et al, 1986, 1991) could be experimented.
The present study did have its limitations. Firstly, the sample of patients was rather small, and a few relatives of the patients had not turned up which could affect the results. Secondly, the therapist was not an expert family therapist, though the instructions from overseas manual and videos were followed. Nevertheless, this lack of high calibre staff could be a more realistic reflection of staff situation in Hong Kong, otherwise the programme could not be applied to other settings in the future. Ths brought to the third defect in the present study and that was the setting. The study was conducted in a university department with extra staff provision. Whether the same programme could be carried out in other psychiatric settings by non-academic busy clinical staff awaits to be seen. Similarly, whether such a programme could be applied to other Chinese patients of different ethnic cultures in various parts of China is still an unanswerable question.
To overcome these hurdles, a training course was organized for clinical staff from other psychiatric units in Hong Kong and different parts of China (Beijing, Shanghai, Hu Bei, Guangzhou and Shenzhen), and they were taught the method of family therapy. A multi-centre trial with better attention to the quality of life area or even the cognitive function area (using new psychological tests), would be conducted in the near future upon successful fund application.
CONCLUSION
It can be seen that the Chinese family structure is still relatively intact, with relatives quite willing to look after their sick members, though the burden of care was quite high on their shoulders. Therefore, they were quite enthusiastic to come to therapy sessions for more knowledge and skills about the disease.
From the results of this small study, it seems that the family behavioural therapy is applicable in Hong Kong and acceptable by the Chinese families. In a way, this is compatible with the general impression that the Chinese patients are more receptive of directive psychotherapy like behavioural therapy than non-directive one. Nevertheless, one should experiment with other models of psychotherapy, and to find out which therapy suits which patient and at what particular time. Experimentation in other settings of different ethnic groups of the Chinese population should also be explored.
REFERENCES
Barrowclough, C., Tarrier, N., Watts, S., et al. (1987). Assessing the functional value of relatives' reported knowledge about schizophrenia. British Journal of Psychiatry, 151, 1-8.
Barrowclough, C. & Tarrier, N. (1992). Families of Schizophrenic Patients. London: Chapman & Hall.
Bebbington, P.E., & Kuipers, L.(1994). The predictive utility of expressed emotion in schizophrenia: An aggregated analysis. Psychological Medicine, 24, 707-718.
Berkowitz, R., Eberlein-Fries, R., Kuipers, L. and Leff , J. (1984). Educating relatives about schizophrenia. Schizophrenia Bulletin, 7, 418-429.
Falloon, I.R.H., Boyd, J.L., McGill, C.W., et al.(1982). Family management in the prevention of exacerbations of schizophrenia. New England J. Medicine, 306, 14371440.
Falloon, I.R.H., Boyd, J.L, McGill, C.W., et al. (1985). Family management in the prevention of morbidity of schizophrenia: Clinical outcome of a two-year longitudinal study. Archives of General Psychiatry, 42, 887-896.
Glick, I., Clarkin, J., Spencer, J., Haas, G., Lewis, A., Peyser, J., DeMane, N., Good-Ellis, M., Harris, E. and Lestelle, V. (1985). A controlled evaluation of inpatient family intervention: I. Preliminary results of a 6-month follow-up. Archives of General Psychiatry, 42: 882 - 886.
Goldman, H.H. (1982) Mental illness and family burden: a public health perspecitve. Hospital and Community Psychiatry, 33, 557-560.
Goldstein, M., Rodnick, E., Evans, J., May, P. and Steinberg, M. (1978). Drug and family therapy in the aftercare of acute schizophrenics. Archives of General Psychiatry, 35, 1169- 1177.
Haley J. (1980). Leaving Home: The Therapy of Disturbed Young People. New York: McGraw Hill.
Hogarty, G., Anderson, C.M., Reiss, D.J., et al. (1986). Family psychoeducation, social skills training and maintenance chemotherapy in the aftercare treatment of schizophrenia. l: One-year effects of a controlled study on relapse and expressed emotion. Archives of General Psychiatry, 43, 633-642.
Hogarty, G., Anderson, C.M., Reiss, D.J. et al. (1991). Family psychoeducation, social skills training and maintenance chemotherapy in the aftercare treatment of schizophrenia. II: Two-year effects of a controlled study on relapse and adjustment. Archives of General Psychiatry, 48, 340-347.
Hsu, J. & Tseng, W.S. (1991). Culture and Family Therapy: Problems and Therapy. New York: Haworth Press.
Hsu, J.(1995). Family therapy for the Chinese: problem and strategies. In Chinese Societies and Mental Health (ed. T.Y. Lin, W.S. Tseng and E.K. Yeh). New York: Oxford University Press.
Lam, D.H., Chan, N.and Leff , J.(1995). Family work for schizophrenia: Some issues for Chinese immigrant families. Journal of Family Therapy, 17, no.3, August, 281-297.
Langsley, D.J., Machotka, P. & Flomenhaft, K.(1971). Avoiding mental hospital admission: A follow-up study. American Journal of Psychiatry, 1'-7, 1391 - 1394.
Larsen, D.L., Attkisson, C.C., Hargreaves, W.A. & Nguyen, T.D. (1979). Assessment of client /patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2, 197-207.
Leff , J., Kuipers, L., Berkowitz, R. & Sturgeon, D. (1982). A controlled trial of social intervention in the families of schizophrenic patients. British Journal of Psychiatry, 141, 121-134.
Leff , J., Kuipers, L., Berkowitz, R. & Sturgeon, D. (1985). A controlled trial of social intervention in the families of schizophrenic patients: Two-year follow-up. British Journal of Psychiatry, 146, 594-600.
Leff , J., Berkowitz, R. Shavit, N., Strachan, A., Glass, l. & Vaughn, C. (1989). A trial of family therapy v.s. a relatives' group for schizophrenia. British J. Psychiatry, 154, 58-64.
Leff. J., Berkowitz, R., Shavit, N., Strachan. A., Glass, I. & Vaughn. C. (1990). A trial of family therapy versus a relatives' group for schizophrenia. Two-year followup. British Journal of Psychiatry, 157, 571-577.
Liberman, R.P., De Risi, W.J.& Mueser, KT. (1989) Social Skills Training for Psychiatric Patients. New York: Pergamon Press.
Linn, LS. (1975) Factors associated with patient evaluation of health care. Milbank Memorial Fund Quarterly, 53, 531-548.
Madanes, C. (1982). Strategic Family Therapy. San Francisco:
Jossey-Bass Publishers.
Mak, K.Y.(1992). Full Report on the Special Project on the Aftercare Service for Patients Discharged from Psychiatric Half-way Houses of the Mental Health Association of Hong Kong. Hong Kong: Mental Health Association of Hong Kong.
Mak, KY. (1996) The clinical use of an aftercare worker for schizophrenic patient discharged from half-way houses in Hong I-<ong. British Journal of Psychiatry, 168, 757761 .
Mcfarlane, W.R., Stastny, P. and Deakins, S. (1992). Family-aided assertive community treatment: A comprehensive rehabilitation and intensive case management approach for persons with schizophrenic disorders. In Effective Psychiatric Rehabilitation (ed.R.P. Liberman). San Francisco: Jossey-Bass Publishers, 43-54.
Mcfarlane, W.R., Lukens, E., Link, B. and et al. (1995). Multiple-family groups and psychoeducation in the treatment of schizophrenia. Archives of General Psychiatry, 52, 679-687.
Mueser, K T. & Gingerich, S.(1994). Coping with Schizophrenia. Oakland: New Harbinger Publications Inc.
Mueser, KT. & Glynn S.M. (1995). Behavioral Family Therapy for Psychiatric Disorders. Boston: Allyn and Bacon.
Nguyen, T.D. (1983) Assessment of patient satisfaction: development a refinement of a service evaluation questionnaire. Evaulation & Program Planning, 6, 299-314.
Overall, J.E. & Gorham, D.R.(1962). The Brief Psychiatric Rating Scale. Psychological Reports, 10, 799-812 .
Randolph, E.T., Eth, S., Glynn, S.M., Liberman,R.P. & et al. (1994). Behavioural family management in schizophrenia. Outcome of a clinic-based intervention. British Journal of. Psychiatry, 164, 501-506.
Selvini-Palazzoli, M., Cirillo, S., Selvini, M., & Sorrentino A.M. (1989). Family Games: General Models of Psychotic Processes in the Family. New York: Norton.
Tarrier, N., Barrowclough, C., Vaughn, C., et al. (1988). The community management of schizophrenia: A controlled trial of a behavioural intervention with families to reduce relapse. British J. Psychiatry, 153, 532-542.
Tarrier, N., Barrowclough, C., Vaughn, C., et al. (1989). The community management of schizophrenia: A two-year follow-up of a behavioural intervention with families. British J Psychiatry, 154, 625-628.
World Health Organization(l989). W.H.O. Psychiatric Disability Assessment Schedule. Geneva: World Health Organization.
*Ki-Yan Mak, MD, FRCPsych, Asociate Professor, Department of Psychiatry, The University of Hong Kong.
M.C. Wong, MBBS, MRCPsych Senior Medical Officer, Rehabilitation Unit, Department of Psychiatry, University of Hong Kong.
L.K. Ma, MEd Family Therapist, Rehabilitation Unit, Department of Psychiatry, University of Hong Kong.
S.C. Fung, BA, Research Assistant, Rehabilitation Unit, Department of Psychiatry, University of Hong Kong.
* Correspondence: Dr. Ki-Yan Mak, Asociate Professor, Department of Psychiatry, The University of Hong Kong. Queen Mary Hospital, Pokfulam Road, Hong Kong.