East Asian Arch Psychiatry 2015;25:47-57
ORIGINAL ARTICLE 
Mr William Wai-Kin Wu, FHKAN (Mental Health Nursing), MSc (Mental Health), MSc (Counselling Studies), BSc (Nursing), APNP, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China.
Address for correspondence: Mr William Wai-Kin Wu, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China.
Tel: (852) 2595 4523; Fax: (852) 2515 0412; Email: wuwk@ha.org.hk
Submitted: 17 October 2014; Accepted: 23 December 2014
Abstract
Objective: Clinically, patients’ characteristics may predict the use of physical restraint in a psychiatric ward. This study aimed to explore significant psychosocial variables in predicting the risk for application of physical restraint with intention of identifying patients at high risk for physical restraint at the time of admission to an acute psychiatric setting.
Methods: The case records of 335 adult patients aged > 18 years, who were treated in 4 acute psychiatric admission wards of a public hospital in Hong Kong from 1 November 2013 to 28 February 2014, were retrospectively reviewed.
Results: Results of statistical analysis indicated involuntary admission, current use of psychiatric medications, no history of violent behaviour, age, and depression as significant predictors of use of physical restraint. The model accounted for 28.5% to 38.5% of the variance in the use of physical restraint. Overall, this model had a success rate of 77.6%.
Conclusion: It was concluded that 39.7% of inpatients admitted to the acute psychiatric admission ward had been restrained at least once in the first 7 days. Significant predictors of restraint included involuntary admission, current use of psychiatric medications, no history of violent behaviour, age, and depression; all of which could be regarded as risk factors for restraint.
Key words: Restraint, physical; Social environment
Introduction
Appropriate usage of physical restraint has challenged psychiatric nurses on ethical and practical levels. Physical restraint has been used frequently to manage challenging behaviour and to safeguard both patients and staff. Clinically, patients’ characteristics seem important enough to predict the use of physical restraint. It is worthwhile examining the psychosocial profile of patients undergoing physical restraint in the acute psychiatric admission ward. A review of the extant literature shows that there have been very few studies on the psychosocial correlates of patients receiving such treatment. It would therefore be interesting to examine whether there are any significant psychosocial factors exhibited by patients via the use of physical restraint. Through understanding patient profiles, it is intended that psychiatric nurses will be able to identify the high-risk group for physical restraint. This would allow them to promptly provide intensive nursing care so as to minimise the application of physical restraint.
Guidelines for Physical Restraints
Systematic literature review on physical restraint of adult psychiatric inpatients indicates that, by physically restraining a patient, the use of physical force is applied to prevent or restrict a patient’s movement. Mechanical devices for physical restraint include straps, cuffs, belts, and some other external devices to restrict a patient from moving. In the psychiatric setting, mechanical restraints involve strapping a patient to a bed in the supine position with wrist and ankle cuffs, with or without a belt across their waist. This is known as the ‘four- or five-point restraint’.1 Hence, physical restraint in this study is defined as “the use of mechanical devices including safety vests, magnetic limb holders, magnetic shoulder straps, pelvic holders, magnetic waists and abdominal belts applied to the patient’s wrists, ankles, shoulders, waist and body that restrict freedom of movement or being secured to the bed or chair”.2
In the UK, the Royal College of Nursing offers guidelines stating that physical restraint should only be used when all other methods of managing the identified problem are considered not suitable or have failed.3 In Ireland, however, there is no legislation about restraining adults.4 In Australia, guidelines for the use of restraint vary across different states.5 In Israel, psychiatric nurses are allowed to restrain patients independently.6 Nurses in Canada are prohibited from using any form of restraint without consent from the client or decision-maker, except in some emergency situations.7 In the US, the JCAHO (Joint Commission on Accreditation of Healthcare Organizations) and the HCFA (Health Care Financing Administration) have both stated clearly that “Seclusion and restraint must be a last resort, emergency response to a crisis situation that presents imminent risk of harm to the patient, staff, or others”.8 In China, there are no nationwide standards concerning physical restraint.9 In Hong Kong, strict standards and regulations have been applied regarding the use of physical restraint. Nurses are required to complete special documentation and observe the process of restraint application.10
Prevalence Rates of Physical Restraint
According to the study by Stewart et al,11 there is a lack of reliable estimates on the prevalence of physical restraint. Since then, various methods of calculating the rate of physical restraint use have been developed with no consensus reached.12 Some studies have suggested that the prevalence rates of physical restraint were very low in psychiatric settings, while other studies have recorded high prevalence rates of physical restraint, with 1 in 3 patients (or more) being restrained during their hospital stay.13 In the US, Canada, Finland, Switzerland, the Netherlands, and Hong Kong, physical restraint is defined as any type of physical restraint applied during the last (or past) 7 days of a patient’s stay at the hospital, including trunk or limb restraint and chair restraint preventing rising, but excluding use of bedrails.14-16
Systematic literature review of studies in the US shows that relatively high baseline frequency rates of physical restraint (29% of patients; 42.7/1000 patient days) have been reported among children and adolescents in psychiatric settings.17 A review of 4 studies conducted in the US from 1990 to 1995 reported a high prevalence of aggressive behaviour in adult psychiatric units, with more than 16% of hospitalised patients displaying aggressive behaviour during the first week after admission.18 Approximately 1 in 15 children undergoing psychiatric evaluation were restrained.19 In one study in a state psychiatric hospital, 51% of the patients required seclusion and restraint.20 The frequency of physical restraint varied from 8.5% to 31% in different states in the US.21,22
Similar results have been found in Europe, with Italy displaying a variance of 10- to 20-fold in the prevalence rate of physical restraint.23 The frequencies of physical restraint in other European countries were as follows: 10% in Finland,24 15% in Denmark,25 and 1.4% in a French psychiatric emergency unit.26 In various Dutch hospitals, 1 in 4 admitted patients experienced a seclusion episode,12 while 19% of patients were mechanically restrained in an Italian acute psychiatric ward.27 In countries such as Iceland and the UK, seclusion and restraint were abolished decades ago and never used again.13,28
The prevalence rates of physical restraint in both China and Taiwan are relatively high. In Taiwan the rate is 39.1%.29 In China, one study indicated that the frequency of physical restraint was 42.6% (213 of 500 cases) with most of the patients being physically restrained (87.6%) having schizophrenia.30 Recently, another study in China reported a higher frequency of physical restraint, at 51.3%, among Chinese psychiatric patients.31 In Israel, the frequency of physical restraint was 14.2%32 and was 8.5% to 18.5% in Australia.33
Psychosocial Correlates and Predictors of Physical Restraints
Gender is almost the commonest psychosocial variable of physical restraint being studied. However, the effects of gender on physical restraint remain a controversial factor. Some studies showed that gender was not related to physical restraint34,35; while others showed that both female36,37 and male38,39 sex were significantly associated with physical restraint. In addition, one study showed that gender, age, and diagnosis were all predictive for restraint.26 One study indicated that ethnicity was a significant predictor of restraint.40 In contrast, some studies suggested that factors such as ethnicity, occupational status, and education level were insignificantly associated with restraint use.34,37,41,42
Similar to gender, the relationship between age and physical restraint is equivocal. In some studies, younger individuals appeared to be at higher risk of being secluded with or without restraint.34,35,37,41 However, in another study of schizophrenic patients, no association with age was found.43 A recent study stated that younger age, schizophrenia or other psychosis, bipolar disorder, personality disorder, and longer stay in hospital were predictors of an episode of seclusion with or without restraint.44
In addition to demographic variables, one study suggested that there were clinical risk factors for physical restraint, including violent behaviour, current alcohol or drug abuse, and pro-criminal attitudes.41 Moreover, involuntary hospitalisation has been linked to seclusion,34 with restrained patients experiencing more episodes of psychiatric admissions.41 Another study indicated that restrained adolescents were more likely to be of male sex, in particular, being an African-American diagnosed with a psychotic disorder and with a history of violent behaviour towards themselves and others.45 Patients with a diagnosis of dementia, impaired mobility, or behavioural problems were more likely to be restrained.46 One study found a primary diagnosis of schizophrenia or other psychosis to be related to use of physical restraint,34 but other research has demonstrated no such association.41 Patients diagnosed with bipolar disorder and who had a history of violence towards others were also suggested to be more likely to be restrained in some studies.44 Another study found a higher seclusion and restraint trajectory to be associated with patients with borderline personality disorder and mental retardation, but found no particular trajectory to be associated with bipolar disorder.37 One study found that young age, diagnosis of borderline personality disorder, and irritability were predictors of seclusion and restraint.21 Another study indicated that patients with mood disorders were more likely to be restrained than patients with schizophrenia or schizoaffective disorder.47 Older age, psychosis, and suicidal behaviour were correlated with seclusion and restraint as shown in another study.48
In summary, a considerable amount of studies have been conducted on the relationship between physical restraint and psychosocial / clinical variables. Although there were no consistent results found among these studies, most of them suggested the variables under study were, to a certain extent, associated with physical restraint. The present study aimed to explore any significant association and possible prediction between patients’ psychosocial / clinical variables and physical restraint.
Methods
This was a cross-sectional retrospective observational research study, with a convenience sampling method. The participants were patients admitted to the acute psychiatric admission wards at a psychiatric unit of a public hospital in Hong Kong. All patients were assigned to either ‘restraint’ or ‘non-restraint’ group depending on whether or not they were physically restrained during the first 7 days of stay in the acute psychiatric admission wards. The medical records of all participants were reviewed to assign participants to the 2 study groups and for data collection.
Intergroup comparisons were made on any significant group differences in the psychosocial and clinical variables. Logistic regression was performed to find out significant predictors of physical restraint.
Participants
All study participants were automatically recruited from inpatients admitted to 4 acute psychiatric admission wards of a public hospital during a 4-month period from 1 November 2013 to 28 February 2014. Those aged < 18 years and discharged against medical advice on the first day of admission were excluded from the study. If a patient had more than one admission to the acute psychiatric admission ward during the study period, only the data for the first admission were included in this study. A total of 335 participants were recruited during the 4-month study period. There were 133 participants in the restraint group and 202 participants in the non-restraint group. The restraint group consisted of 56 men and 77 women, with a mean (± standard deviation) age of 38.3 ± 15.4 years (range, 18-93 years). The non-restraint group consisted of 89 men and 113 women, with a mean age of 43.5 ± 16.9 years (range, 18-87 years).
Measures
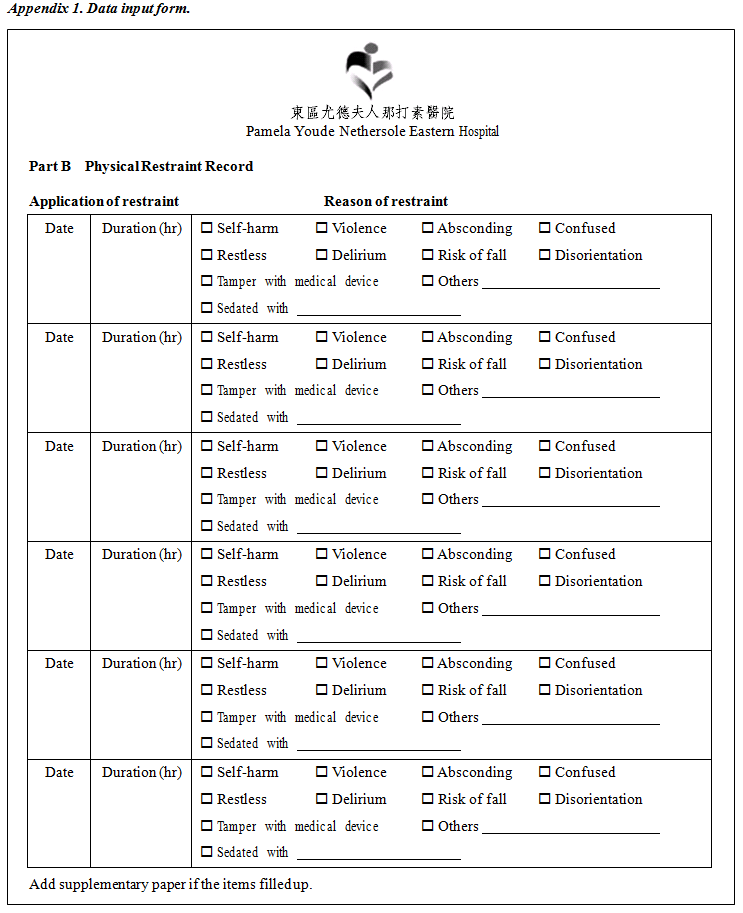
A data collection instrument was designed (Appendix 1) to record individual patient’s demographic information and clinical conditions. The data entry form consisted of 2 pages. The first page was a data collection form for psychosocial and clinical variables. The second page was a form for data collection on the incident(s) of physical restraint during the stay in the acute admission ward.
Sixteen psychosocial and clinical variables were used, 12 of which were nominal variables and 8 of which were dichotomous variables (sex, ethnicity, occupational status, history of psychiatric treatment, history of violent behaviour, co-morbidity with substance misuse, physical complications, and types of hospitalisation). Three of the nominal variables (marital status, use of antipsychotic medications, and source of admission) had 3 categories, whereas 1 nominal variable (primary diagnosis) contained more than 3 categories.
Of the 2 ordinal variables, education level had 4 levels, while ‘priority follow-up’ (PFU) status had 3 levels. Priority follow-up is a system that provides guidance to medical and nursing staff to identify and manage patients with a history of criminal violence, violent propensity, or assessed disposition to violence. Patients given PFU status required additional care and attention. The 3 levels of PFU status included ‘non-PFU (ordinary)’ referring to the absence of a history of criminal violence or assessed disposition to violence; ‘PFU-target’ referring to the presence of a history of criminal violence or assessed disposition to violence; and ‘PFU-subtarget’ which classified the most dangerous patients with a history of criminal violence or assessed disposition to violence who required special assessment and extra care.
The 2 continuous variables were age and the Nurses’ Global Assessment of Suicide Risk (NGASR) scores. The dependent variable was use of physical restraint during the 7-day stay in the acute psychiatric admission wards. Each category of the independent variables and characteristic of the restraint episode are shown in Appendix 2.
Before implementing the study, approval was obtained from the psychiatric department of a local public hospital. The research proposal was subsequently submitted to the hospital research ethics committee for approval. Neither written consents nor interviews were needed as data were retrieved retrospectively from the patients’ medical records. Participants’ personal identifying information was kept confidential. The data were analysed by using the Statistical Package for the Social Sciences Windows version 19.0 (IBM Corp, Armonk [NY], US). All decisions were made at the confidence level of p ≤ 0.05.
Results
Intergroup Comparisons
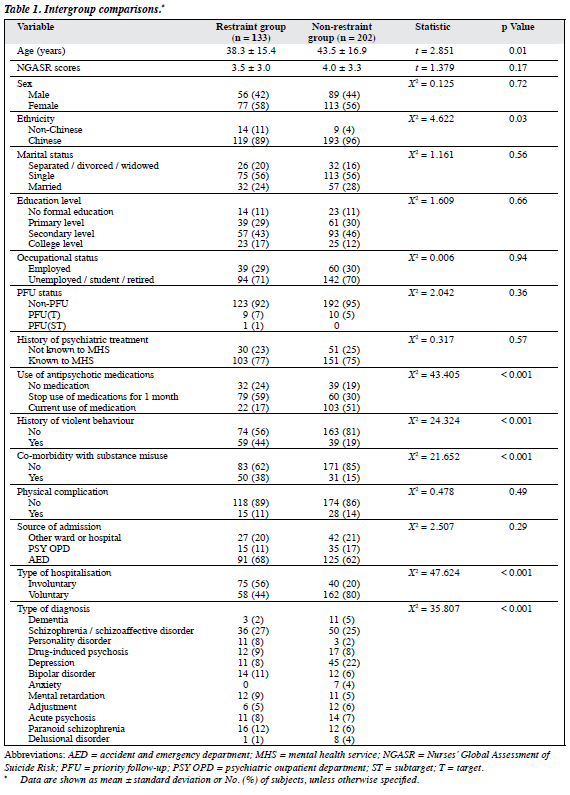
In this study, 39.7% (133/335) of inpatients during the first 7 days in acute psychiatric admission wards had been restrained at least once. Chi-square and independent t tests based on bivariate statistics were utilised for intergroup comparison of the variables under study. As shown in Table 1, there were statistically significant intergroup differences for the factor of age. The restraint group was significantly younger (t = 2.851, p = 0.01) than the non-restraint group. The results indicated that the restraint group had significant differences in the factor of ethnicity (X2 = 4.622, p = 0.03), use of antipsychotic medications (X2 = 43.405, p < 0.001), type of diagnosis (X2 = 35.807, p < 0.001), co-morbidity with substance misuse (X2 = 21.652, p < 0.001), type of hospitalisation (X2 = 47.624, p < 0.001), and history of violent behaviour (X2 = 24.324, p < 0.001) when compared with the non-restraint group. No significant relationships were reported between use of physical restraint and education level, marital status, occupation status, sex, PFU status, history of psychiatric treatment, physical complications, source of admission, and NGASR scores. Thus, all these factors were excluded from the logistic analysis regarding theoretical and statistical hypotheses.
Logistic Regression Model
Logistic regression models were applied to predict the use of physical restraint based on multiple psychosocial covariates and clinical factors. A stepwise likelihood ratio (forward likelihood ratio) method was adopted to conduct logistic regression analysis. For this method, factors were entered into the analysis not based on their likelihood ratio values, but on the maximum partial likelihood-ratio estimates. In all, 7 factors were entered in the analysis: ethnicity, use of antipsychotic medications, primary diagnosis, co- morbidity with substance misuse, type of hospitalisation, history of violent behaviour, and age. The factor with the highest likelihood-ratio values was entered first, followed by the second highest until no additional contribution to the variance in the outcome was found.
Regression Model Summary
Table 2 conveys the results of the likelihood ratio (-2 log likelihood), Cox and Snell R2 and Nagelkerke R2 values. When the first factor (involuntary admission) was entered into the analysis, the likelihood ratio was 402.404 and the proportion of variance in the use of restraint due to involuntary admission factor ranged between 13.3% and 18.0% (Cox and Snell R2 = 0.133, Nagelkerke R2 = 0.180). Entry of the second factor (current use of psychiatric medications) into the analysis changed the likelihood ratio to 368.150 and the proportion of variance in the use of restraint due to this factor ranged between 21.7% and 29.4%, and that this factor added between 8.4% and 11.4% to the variance in the use of restraint. Adding the third factor (no history of violent behaviour) into the analysis altered the likelihood ratio to 349.758 and the proportion of variance in the criterion due to this factor ranged between 25.9% and 35.0%. This factor added between 4.2% and 5.6% to the variance in the use of restraint. When the forth factor (age) was incorporated in the analysis, the likelihood ratio was 342.634 and the proportion of variance in the criterion due to this factor ranged between 27.4% and 37.1%. This factor added between 1.5% and 2.1% to the variance in the use of restraint. Finally, with the fifth factor (depression) entering the analysis, the likelihood ratio was 337.751 and the proportion of variance in the criterion due to this factor ranged between 28.5% and 38.5%. This factor added between 1.1% and 1.4% to the variance in the use of restraint.
Hosmer-Lemeshow Test of Goodness-of-Fit
The Hosmer-Lemeshow test compares the observed model with the predicted model to examine how well the model identified from the samples fitted the population from which the data were collected. The results show that the 5-factor model was not significantly different than the expected population’s model (X2 = 10.218, p = 0.25). The 2 models were not significantly different, thus, this model had a very good fit of the population.
Logistic Regression Accuracy of Prediction
Table 3 displays the results of the level of accuracy of the model in classifying the patients in the restraint group or the non-restraint group. This shows the observed and predicted frequency in each group and how correct the model was in predicting use of physical restraint. Of the 202 subjects in observed non-restraint group, the model correctly predicted 173 for a success rate of 85.6%. In other words, the model missed 14.3% of the cases (i.e. 29 cases predicted as non- restraint group when they should have been restraint group). This also shows that of the 133 subjects in observed restraint group, the model correctly predicted 87 for a success rate of 65.4%. That means the model missed 34.5% of the cases (i.e. 46 cases predicted as non-restraint group when they should have been restraint group). The overall accuracy success rate was 77.6%.
Sensitivity and Specificity of the Model
In this study, the sensitivity was 65.4% (87/133) and the specificity was 85.6% (173/202). The false-positive rate was 14.3% (29/202) and the false-negative rate was 34.5% (46/133).
Discussion
This study found that 39.7% of inpatients during the first 7 days in acute psychiatric admission wards had been restrained at least once. The use of physical restraint was not rare for patients in the acute psychiatric admission wards. This frequency of use of physical restraint was more or less the same in nearby Asian countries: 51.3% in China31 and 39.1% in Taiwan.29
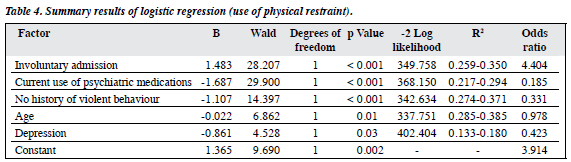
Based on the results of logistic regression, Table 4 shows that 5 factors emerged as significant predictors of inpatients being physically restrained during the first 7 days in acute psychiatric admission wards. These factors were involuntary admission (Wald = 28.207, df = 1, p < 0.001), current use of psychiatric medications (Wald = 29.900, df = 1, p < 0.001), no history of violent behaviour (Wald = 14.397, df = 1, p < 0.001), age (Wald = 6.862, df = 1, p = 0.01), and depression (Wald = 4.528, df = 1, p = 0.03). The older the patients admitted to a psychiatric hospital under involuntary admission without psychiatric medication, and who had a history of violent behaviour while having no diagnosis (such as depression) were more likely to be restrained than younger voluntarily admitted patients with current use of medications, with no history of violent behaviour, and depression. The results of the overall model significantly improved the prediction of the probability of inpatients being restrained during the first 7-day stay in a acute psychiatric admission ward (X2 = 112.343, df = 5, p < 0.001). This model had a very good fit (-2 log likelihood = 337.751, Hosmer-Lemeshow, X2 = 10.218, df = 8, p = 0.25). The results of Cox and Snell and Nagelkerke R2 values indicate that involuntary admission accounted for 13.3% to 18.0%; current use of psychiatric medications for another 8.4% to 11.4%; no history of violent behaviour added 4.2% to 5.6%; as well as age and depression adding 1.5% to 2.1% and 1.1% to 1.4%, respectively, to the variance in the use of physical restraint. Overall the model accounted for 28.5% to 38.5% of the variance in the use of physical restraint. Finally, the model correctly classified 85.6% of the non- restraint group and 65.4% of the restraint group of patients. Overall, this model had a success rate of 77.6%.
Equation of Logistic Regression
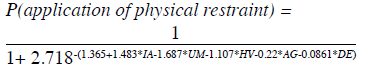
The odds of an event occurring was defined as the probability of an event occurring divided by the probability of its non- occurrence. In this study, the odds was interpreted as the probability (P) of application of physical restraint divided by the probability of no application of physical restraint:
The “odds ratio regression” equation was used to compute the probability of an event occurring:
According to the results of the logistic regression coefficient (Table 4), the equation was presented as follows:
where IA stands for involuntary admission, UM for current use of psychiatric medications, HV for no history of violent behaviour, AG for age, and DE for depression.
The logit — the natural logarithm of an odds ratio — is the central mathematical concept of logistic regression and is the basis for developing the model in this study. The logistic equation was recast as an odds formula as follows.
Logit (application of physical restraint) = α+ β1*IA + β2*UM + β3*HV +β4*AG +β5*DE
The mathematical model of the predicted logit of (application of physical restraint) was 1.365 + (1.483) * involuntary admission + (-1.687) * current use of psychiatric medications + (-1.107) * no history of violent behaviour + (-0.22) * age + (-0.861) * depression.
Implications
This is, to the author’s knowledge, the first study in Hong Kong to elucidate psychiatric patients’ psychosocial and clinical factors associated with physical restraint practice in the acute psychiatric services. The findings of this study can be used as a reference for training mental health professionals — especially in the field of psychiatric nursing — in minimising the incidences of physical restraints in hospitals. The significant predictors of physical restraint obtained in this study can be regarded as risk factors for restraint. Patients admitted to acute admission wards, or the psychiatric wards in general, can be checked to ascertain whether they possess these risk factors for physical restraint. In this way, effective handling can be done promptly before applying the last resort of physical restraint. Psychiatric nurses could become more competent and confident in preparing appropriate strategies to meet the needs of patients prior to the use of physical restraint, provided they are able to acquire knowledge of an individual patient’s clinical presentation and characteristics upon admission to acute psychiatric wards.
Limitations
This study have several limitations. First, the data collection was retrospective and therefore causality could not be established. Second, this study was permitted in the psychiatric services within general hospitals where the restraint practice was explicitly influenced by corporate factors. In traditional psychiatric hospitals, the practice of restraint might be different and tended to report less use of physical restraint. Thus, the transferability is considered to be limited and the generalisability of the findings was also limited by the fact that only a single psychiatric department was investigated. The results could then be considered as representative since the study included 335 consecutive admissions with no selection bias found in the comparison of the restrained and non-restrained groups.
In addition, this study only included the patient- related variables and the clinical factors associated with the use of physical restraint. The process of making the decision to apply physical restraint is one of complex interactive reasoning. The frequency of use of physical restraint was determined not only by individual psychosocial variables and clinical presentations, but also by staff attitudes and behaviour, interactions of fellow patients, and other environmental influences.49 Thus, the study excluded other staff-related factors and institutional policy factors from the logistic regression analysis that might limit the validity of the findings. However, the use of physical restraint was indicated and carried out within the strict guideline and protocol, and this study was conducted in the same department that was relatively independent from staff-related factors and institutional policy–related factors. Thus, this study assumed a constant to the staff-related factors and institutional policy–related factors.
Recommendations
To obtain greater precision in the severity of physical restraint, particularly that used in psychiatric acute admission settings, it is further recommended to rate the intensity and durations of physical restraint on an ordinal scale and to perform ordinal logistic regression analysis. In addition, prospective study of physical restraint practice is recommended in the future to examine the effects of psychosocial covariates and clinical parameters on restraint practice.
Declaration
No financial support and no conflict of interest were declared. This study was self-supported for the preparation of thesis of MSc (Mental Health), The Chinese University of Hong Kong.
Acknowledgement
I gratefully acknowledge and express my appreciation to volunteers Mr Dixon Man, Ms Cindy Lee, and Ms KL Cheng for their assistance in data collection of this study. I would like to thank Dr Eva Dunn (Chief of Service), Mr Ben Hui (Department Operations Manager), and Mr Ken Chan (Department Operations Manager) from the Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, for their permission to conduct this study.
References
- Stewart D, Bowers L, Simpson A, Ryan C, Tziggili M. Manual restraint of adult psychiatric inpatients: a literature review. J Psychiatr Ment Health Nurs 2009;16:749-57.
- Hellerstein DJ, Staub AB, Lequesne E. Decreasing the use of restraint and seclusion among psychiatric inpatients. J Psychiatr Pract 2007;13:308-17.
- Watson R. Restraint: its use and misuse in the care of older people. Nurs Older People 2001;13:21-5.
- Guidelines on the use of restraint in the care of the older person. Irish Nurses Organization 2003. Available from: http://www.inmo.ie/Attachment.aspx?nAttID=1484 . Accessed 20 Sep 2013.
- Registration Transition. Australian Health Practitioner Regulation Agency 2010. Available from: http://www.nursingmidwiferyboard.gov.au/Registration-Transition. Accessed 6 Sep 2013.
- Ben Natan M, Akrish O, Zaltkina B, Noy RH. Physically restraining elder residents of long-term care facilities from a nurses’ perspective. Int J Nurs Pract 2010;16:499-507.
- Practice standard: restraints. Toronto: College of Nurses of Ontario; 2009.
- Patient safety and medical / health care error reduction standards. In: Joint Commission on Accreditation of Healthcare Organizations (JCAHO). Comprehensive Accreditation Manual for Hospitals. Oak Terrace, Illinois: JCAHO 2001; LD.3.4.1.
- Zhou M, Zhang JW, Bian Q, Xie B. The strategy for seclusion and restraint in psychiatric patients [in Chinese]. Lin Chuang Jing Shen Yi Xue Za Zhi 2010;20:131-3.
- Guideline on restraint management. Departmental guidelines. Hong Kong: Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital; 2013.
- Stewart D, Van der Merwe M, Bowers L, Simpson A, Jones J. A review of interventions to reduce mechanical restraint and seclusion among adult psychiatric inpatients. Issues Ment Health Nurs 2010;31:413-24.
- Janssen WA, Noorthoorn EO, de Vries WJ, Hutschemeakers GJ, Lendemeijer HH, Widdershoven GA. The use of seclusion in the Netherlands compared to countries in and outside Europe. Int J Law Psychiatry 2008;3:463-70.
- Steinert T, Lepping P, Bernhardsgrütter R, Conca A, Hatling T, Janssen W, et al. Incidence of seclusion and restraint in psychiatric hospitals: a literature review and survey of international trends. Soc Psychiatry Psychiatr Epidemiol 2010;45:889-97.
- Feng Z, Hirdes JP, Smith TF, Finne-Soveri H, Chi I, Du Pasquier JN, et al. Use of physical restraints and antipsychotic medications in nursing homes: a cross-national study. Int J Geriatr Psychiatry 2009;24:1110-8.
- Huizing AR, Hamers JP, Gulpers MJ, Berger MP. Preventing the use of physical restraints on residents newly admitted to psycho-geriatric nursing home wards: a cluster-randomized trial. Int J Nurs Stud 2009;46:459-69.
- Find and compare nursing homes. Medicare.gov website: http://www.medicare.gov/NHCompare. Accessed 6 Sep 2013.
- De Hert M, Dirix N, Demunter H, Correll CU. Prevalence and correlates of seclusion and restraint use in children and adolescents: a systematic review. Eur Child Adolesc Psychiatry 2011;20:221-30.
- Choe JY, Teplin LA, Abram KM. Perpetration of violence, violent victimization, and severe mental illness: balancing public health concerns. Psychiatr Serv 2008;59:153-64.
- Dorfman DH, Mehta SD. Restraint use for psychiatric patients in the pediatric emergency department. Pediatr Emerg Care 2006;22:7-12.
- Phillips P, Nasr SJ. Seclusion and restraint and prediction of violence. Am J Psychiatry 1983;140:229-32.
- Swett C. Inpatient seclusion: description and causes. Bull Am Acad Psychiatry Law 1994;22:421-30.
- Currier GW, Allen MH. Emergency psychiatry: physical and chemical restraint in the psychiatric emergency service. Psychiatr Serv 2000;51:717-9.
- Beghi M, Peroni F, Gabola P, Rossetti A, Cornaggia CM. Prevalence and risk factors for the use of restraint in psychiatry: a systematic review. Riv Psichiatr 2013;48:10-22.
- Kaltiala-Heino R, Korkeila J, Touhimäki C, Tuori T, Lehtinen V. Coercion and restrictions in psychiatric inpatient treatment. Eur Psychiatry 2000;15:213-9.
- Øhlenschlaeger J, Nordentoft M. Coercion in patients who at their first contact with the psychiatric services system were diagnosed within the schizophrenia-spectrum in Denmark. A register study. Nord J Psychiatry 2008;62:77-81.
- Guedj MJ, Raynaud P, Braitman A, Vanderschooten D. The practice of restraint in a psychiatric emergency unit [in French]. Encephale 2004;30:32-9.
- Grassi L, Peron L, Marangoni C, Zanchi P, Vanni A. Characteristics of violent behaviour in acute psychiatric in-patients: a 5-year Italian study. Acta Psychiatr Scand 2001;104:273-9.
- Steinert T, Lepping P. Legal provisions and practice in the management of violent patients. A case vignette study in 16 European countries. Eur Psychiatry 2009;24:135-41.
- Yeh SH, Lin LW, Wang SY, Wu SZ, Lin JH, Tsai FM. The outcomes of restraint reduction program in nursing homes [in Chinese]. Hu Li Yan Jiu 2001;9:183-93.
- Li LY, Zhou GH. An investigation on physical restraint in psychiatric patients [in Chinese]. Chin J Pract Nurs 1994;10:2-3.
- Zhu XM, Xiang YT, Zhou JS, Gou L, Himelhoch S, Ungvari GS, et al. Frequency of physical restraint and its associations with demographic and clinical characteristics in a Chinese psychiatric institution. Perspect Psychiatr Care 2014;50:251-6.
- Porat S, Bornstein J, Shemesh AA. The use of restraint on patients in Israeli psychiatric hospitals. Br J Nurs 1997;6:864-6, 868-73.
- Irving K. Inappropriate restraint practices in Australian teaching hospitals. Aust J Adv Nurs 2004;21:23-7.
- Tunde-Ayinmode M, Little J. Use of seclusion in a psychiatric acute inpatient unit. Australas Psychiatry 2004;12:347-51.
- Knutzen M, Sandvik L, Hauff E, Opjordsmoen S, Friis S. Association between patients’ gender, age and immigrant background and use of restraint — a 2-year retrospective study at a department of emergency psychiatry. Nord J Psychiatry 2007;61:201-6.
- Ahmed AG, Lepnurm M. Seclusion practice in a Canadian forensic psychiatric hospital. J Am Acad Psychiatry Law 2001;29:303-9.
- Beck NC, Durrett C, Stinson J, Coleman J, Stuve P, Menditto A. Trajectories of seclusion and restraint use at a state psychiatric hospital. Psychiatr Serv 2008;59:1027-32.
- Thompson P. The use of seclusion in psychiatric hospitals in the Newcastle area. Br J Psychiatry 1986;149:471-4.
- Legris J, Walters M, Browne G. The impact of seclusion on the treatment outcomes of psychotic in-patients. J Adv Nurs 1999;30:448- 59.
- Todd RL. The prediction of the intervention usage of restraint and seclusion within an inpatient adolescent male and female psychiatric facility due to extreme agitation and / or aggression [thesis]. Chicago: Adler School of Professional Psychology; 2004.
- Thomas SD, Daffern M, Martin T, Ogloff JR, Thomson LD, Ferguson M. Factors associated with seclusion in a statewide forensic psychiatric service in Australia over a 2-year period. Int J Ment Health Nurs 2009;18:2-9.
- Bennewith O, Amos T, Lewis G, Katsakou C, Wykes T, Morriss R, et al. Ethnicity and coercion among involuntarily detained psychiatric in- patients. Br J Psychiatry 2010;196:75-6.
- Steinert T, Bergbauer G, Schmid P, Gebhardt RP. Seclusion and restraint in patients with schizophrenia: clinical and biographical correlates. J Nerv Ment Dis 2007;195:492-6.
- Dumais A, Larue C, Drapeau A, Ménard G, Giguère Allard M. Prevalence and correlates of seclusion with or without restraint in a Canadian psychiatric hospital: a 2-year retrospective audit. J Psychiatr Ment Health Nurs 2011;18:394-402.
- Hamming SG. Selected demographic and MMPI scales as predictors of seclusion and restraint in an inpatient psychiatric adolescent male population [thesis]. The Chicago School of Professional Psychology; 1993.
- DeSantis J, Engberg S, Rogers J. Geropsychiatric restraint use. J Am Geriatri Soc 1997;45:1515-8.
- Kaplan Z, Schild K, Levine J. Violence in hospitalized psychiatric patients: diurnal and seasonal patterns. Psychiatry Res 1996;60:199- 204.
- Sourander A, Ellilä H, Välimäki M, Piha J. Use of holding, restraints, seclusion and time-out in child and adolescent psychiatric in-patient treatment. Eur Child Adolesc Psychiatry 2002;11:162-7.
- Whittington R, Richter D. Interactional aspects of violent behavior on acute psychiatric wards. Psychol Crime Law 2005;11:377-88.