East Asian Arch Psychiatry 2015;25:164-167
ORIGINAL ARTICLE
Dr Kit-Ling Lau, MBCHB, FHKAM (Psychiatry), FHKCPsych, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China.
Dr Patty Heung-Wah Yim, MBCHB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China.
Address for correspondence: Dr Kit-Ling Lau, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China.
Tel: (852) 2595 6111; Email: laukl@ha.org.hk
Submitted: 17 March 2015; Accepted: 28 May 2015
Abstract
Objectives: To examine the rate of neutropenia and agranulocytosis, and the pattern of development of these 2 disorders among Chinese patients prescribed clozapine treatment in a local psychiatric unit.
Methods: Patients who were receiving clozapine when they were under the care of Pamela Youde Nethersole Eastern Hospital Psychiatric Unit, Hong Kong, from 1 January 1997 to 31 December 2012 and who developed neutropenia and agranulocytosis from 1 January 1997 to 30 June 2013 were retrospectively reviewed.
Results: A total of 13 patients out of 980 clozapine recipients developed neutropenia and 3 developed agranulocytosis during treatment. Half of them were aged > 50 years and three quarters were female. The majority of patients who developed neutropenia and agranulocytosis were prescribed > 1 psychotropic medication in addition to clozapine. Half of the incidents occurred in the first 18 weeks of clozapine treatment.
Conclusion: Long-term monitoring of white cell count is necessary during clozapine treatment. The concurrent use of clozapine with other potentially leukopenic psychotropic drugs should be limited.
Key words: Agranulocytosis; Clozapine; Neutropenia
Introduction
The introduction of dibenzodiazepine antipsychotic agent, clozapine, is an important development in the pharmacotherapy of schizophrenia. Clozapine is superior to standard antipsychotic drugs in the treatment of patients with refractory schizophrenia.1 Unlike classic neuroleptic agents, clozapine is not associated with the development of acute extrapyramidal symptoms or tardive dyskinesia.
Despite the promise of clozapine, its use has been limited by the risk of neutropenia and potentially fatal agranulocytosis.2 The pathophysiologic mechanism is unknown, but there is evidence that the reaction is immunologically mediated.3 Reports from Europe in the 1970s described an incidence of agranulocytosis among patients given clozapine of 1% to 2% per year, and mortality among agranulocytosis cases of 32%.4
After the introduction of a clozapine monitoring system in the 1990s, the incidence of agranulocytosis among clozapine recipients dropped significantly.2 In many countries, patients treated with clozapine must register with the Clozapine Patient Monitoring Service, ensuring that no patient will receive the drug without a recent satisfactory haematological result. It also helps guarantee that clozapine is stopped immediately if a patient develops severe neutropenia or agranulocytosis.
In the UK and Ireland, the white cell count must be monitored weekly for the first 18 weeks of clozapine treatment, fortnightly to the end of the first year of treatment and 4-weekly thereafter. This practice was based on the findings of a study of 12,670 clozapine recipients in the UK and Ireland,5 in which over 80% developed agranulocytosis within the first 18 weeks of treatment.
In Hong Kong, clozapine monitoring follows the practice in the UK. Nonetheless different racial groups may have a different metabolic capacity that can have an important effect on treatment efficacy and side-effect profile. For clozapine, racial differences in metabolism have been noted for Caucasian compared with Chinese patients.6 Clozapine-related agranulocytosis may also be more common in Asians than in Caucasians.5
Despite the significance of neutropenia and agranulocytosis among clozapine recipients, there are no local data. This study aimed to determine the rate of neutropenia and agranulocytosis, and the pattern of development of these incidents among Chinese patients prescribed clozapine in a local psychiatric unit. The outcome of clozapine recipients who developed neutropenia and agranulocytosis was also examined.
Methods
This was a retrospective review of case notes for all Chinese patients who were receiving clozapine when they were under the care of Pamela Youde Nethersole Eastern Hospital Psychiatric Unit, Hong Kong, from 1 January 1997 to 31 December 2012 and developed neutropenia or agranulocytosis from 1 January 1997 to 30 June 2013. Neutropenia is defined as an absolute neutrophil count of < 1500/mm3. Agranulocytosis indicates a severe degree of neutropenia (i.e. absolute neutrophil count < 500/mm3). The cases of neutropenia and agranulocytosis were identified by the Clinical Data Analysis and Reporting System. The medical records of all the cases were reviewed. Information about each patient’s demographics, psychiatric and physical diagnoses, duration and dose of clozapine upon identification of neutropenia or agranulocytosis, concurrent pharmacological treatment, management of the episode and outcome were retrieved from the medical records.
Statistical Analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences Windows version 16.0, and included descriptive statistics for the extracted data. Gender difference was compared in patients with and without development of neutropenia and agranulocytosis using the Fisher’s exact test.
Results
Demographic and Clinical Characteristics
During the study period, 980 patients were prescribed clozapine, of whom 504 (51%) were female and 476 (49%) were male. Thirteen (1.3%) patients developed neutropenia and 3 (0.3%) developed agranulocytosis during clozapine treatment. Due to the small number of cases, the patients who developed neutropenia and agranulocytosis were grouped together for analysis.
These 16 patients aged from 28 to 70 years, with a mean of 48 and a median of 49 years. Half of them were aged > 50 years. Twelve (75%) were females. Schizophrenia (81%) was the most common psychiatric diagnosis, followed by schizoaffective disorder (13%) and bipolar affective disorder (6%). Nine (56%) patients enjoyed good physical health. Two (13%) patients had metabolic disorders such as hypertension or diabetic mellitus. One patient had a history of traumatic brain injury. One patient had a history of idiopathic thrombocytopenia and 1 patient had a history of idiopathic pancytopenia: both had a normal blood cell count prior to commencement of clozapine. One patient had a history of developing thrombocytopenia while on sodium valproate that was consequently withheld during clozapine treatment.
The dosage of clozapine upon detection of neutropenia and agranulocytosis ranged from 25 mg to 600 mg, with a mean of 323 mg per day and a median of 250 mg per day.
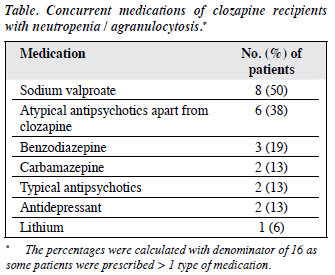
In all, 14 (88%) patients were prescribed concurrent psychotropic medications (Table). Anticonvulsants were the most common concurrent medication. Eight (50%) patients were taking sodium valproate while 2 (13%) were prescribed carbamazepine. Six (38%) patients were prescribed other atypical antipsychotic agents and 2 (13%) were also taking typical antipsychotics. Three (19%) patients were receiving benzodiazepine, and 13% and 6% of them were prescribed antidepressants and lithium, respectively.
Duration of Clozapine Treatment upon Identification of Neutropenia and Agranulocytosis
Eight (50%) patients developed neutropenia and agranulocytosis within the first 18 weeks of clozapine treatment. Six (37.5%) cases occurred between 1 and 4 years. The remaining 2 occurred at the 9th year of treatment and the 17th year of treatment, respectively (Fig).
Outcome
In all cases, clozapine was stopped after detection of neutropenia and agranulocytosis. All of the 3 patients with agranulocytosis were given granulocyte-macrophage colony-stimulating factor to stimulate granulopoiesis. No mortality was reported. In this cohort, 2 of the patients with clozapine-induced neutropenia were rechallenged with clozapine at a later time but both developed neutropenia again on second exposure to clozapine.
Discussion
This study represents a pilot investigation to delineate the rate of neutropenia and agranulocytosis in Chinese clozapine recipients in Hong Kong. The rate of neutropenia was 1.3% in our study, which is lower than that reported in the UK (2.9%) and Korea (10.28%). The rate of agranulocytosis among clozapine recipients in our study was 0.3%, which is also lower than that reported in the UK (0.8%), the US (1%), and Korea (0.8%).5,7,8
Of the cases of neutropenia and agranulocytosis, 75% of patients were female, but the difference was not statistically significant (p = 0.08). This finding is contrary to previous data that identified female gender as a risk factor.5,8
Half of the incidents occurred in the first 18 weeks. This figure is consistent with other large-scale studies that demonstrated a peak incidence of both neutropenia and agranulocytosis in the first 18 weeks of treatment.5,8
The majority of our patients who developed neutropenia and agranulocytosis were prescribed > 1 psychotropic medication in addition to clozapine. Sodium valproate was the most commonly prescribed concurrent drug. A combination of clozapine and sodium valproate appears to be associated with a greater risk for neutropenia or agranulocytosis.9 It has been suggested that the addition of leukopenic drugs to clozapine treatment should be limited because of an increased risk of neutropenia or agranulocytosis, especially since clozapine is often a last- resort treatment for refractory schizophrenia.10
Two patients were rechallenged with clozapine but both developed neutropenia. This result is in accordance with previous findings that a significant number of patients who have previously experienced neutropenia or agranulocytosis during clozapine therapy will develop a blood dyscrasia on rechallenge.11
Limitations
Many countries have a central patient database of the clozapine monitoring service, in which all patients treated with clozapine must be registered and their blood results recorded. This database serves as an important source to estimate the incidence of clozapine-induced neutropenia and agranulocytosis and to examine potential risk factors. In Hong Kong, there is no such central registry. Therefore, for such a rare incident, only a retrospective review is possible. Although the period that we studied spanned > 16 years, the number of cases remained small. Collaborating with other local psychiatric centres would definitely increase the statistical power and better delineate the rate and associated factors of neutropenia and agranulocytosis among clozapine recipients in Hong Kong.
Conclusion
This study represents a pilot investigation to delineate the pattern of clozapine-induced neutropenia and agranulocytosis in Hong Kong. Although half of the affected patients developed neutropenia and agranulocytosis within 18 weeks, both disorders could also develop several years after clozapine treatment. Long-term monitoring of white blood cells is thus necessary. Closer monitoring should be applied to clozapine recipients with a history of blood dyscrasia. The combination of clozapine and other potentially leukopenic drugs, especially sodium valproate, should be limited. Clozapine rechallenge should not be undertaken lightly, because patients rechallenged with clozapine are considerably more likely to develop a further blood dyscrasia.
Declaration
The authors declare that they have no source of financial support for the study.
References
- Kane J, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1998;45:789-96.
- Honigfeld G, Arellano F, Sethi J, Bianchini A, Schein J. Reducing clozapine-related morbidity and mortality: 5 years of experience with the Clozaril National Registry. J Clin Psychiatry 1998;59 Suppl 3:3-7.
- Pisciotta AV, Konings SA, Ciesemier LL, Cronkite CE, Lieberman JA. Cytotoxic activity in serum of patients with clozapine-induced agranulocytosis. J Lab Clin Med 1992;119:254-66.
- de la Chapelle A, Kari C, Nurminen M, Hernberg S. Clozapine- induced agranulocytosis. A genetic and epidemiologic study. Hum Genet 1977;37:183-94.
- Munro J, O’Sullivan D, Andrews C, Arana A, Mortimer A, Kerwin R. Active monitoring of 12,760 clozapine recipients in the UK and Ireland. Beyond pharmacovigilance. Br J Psychiatry 1999;175:576-80.
- Chong SA, Remington G. Ethnicity and clozapine metabolism. Br J Psychiatry 1998;172:97.
- Alvir JM, Lieberman JA, Safferman AZ, Schwimmer JL, Schaaf JA. Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med 1993;329:162-7.
- Kang BJ, Cho MJ, Oh JT, Lee Y, Chae BJ, Ko J. Long-term patient monitoring for clozapine-induced agranulocytosis and neutropenia in Korea: when is it safe to discontinue CPMS? Hum Psychopharmacol 166 East Asian Arch Psychiatry 2015, Vol 25, No.4 2006;21:387-91.
- Madeb R, Hirschmann S, Kurs R, Turkie A, Modai I. Combined clozapine and valproic acid treatment-induced agranulocytosis. Eur Psychiatry 2002;17:238-9.
- Imbarlina MJ, Sarkar S, Marwah S, Parepally H, Johnston PR, Brar JS, et al. Leukopenia in clozapine treated patients may be induced by other drugs: a case series. Eur Psychiatry 2004;19:506-9.
- Dunk LR, Annan LJ, Andrews CD. Rechallenge with clozapine following leucopenia or neutropenia during previous therapy. Br J Psychiatry 2006;188:255-63.