East Asian Arch Psychiatry 2017;27:35-7
CASE REPORT
Dr Nicholas Pang, MBBS, Department of Psychiatry, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia Selangor, Malaysia; Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Malaysia.
Dr Nathisha Thrichelvam, MBBS, Department of Psychiatry, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia. Dr Khin Ohnmar Naing @ Noor Jan, MBBS, MMed, Department of Psychiatry, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia.
Address for correspondence: Dr Nicholas Pang, Department of Psychiatry, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, 43400
UPM Serdang, Selangor, Malaysia. Email: nicholas86@gmail.com
Submitted: 17 May 2016; Accepted: 8 August 2016
Abstract
Unlike clozapine, and despite its structural similarities, olanzapine is not usually associated with haematological suppression. Nonetheless this case report highlights an incident of olanzapine-induced thrombocytopenia and neutropenia in a first-contact patient. We report on a 50-year-old male who presented with 7 years of delusions and hallucinations. A diagnosis of schizophrenia was made in the absence of any suggestive features of mood disorders, substance abuse or organicity, and olanzapine as second-line treatment. Within a week of starting treatment he developed biochemical neutropenia and thrombocytopenia without any clinical symptoms that resolved after cessation of the offending drug. An organic workup for infective, inflammatory, and neoplastic causes was unremarkable. Comparison with other case reports and 3 postulated mechanisms are discussed. Despite its comparative rarity, the addition of this case report to a growing corpus suggests that clinicians should maintain heightened surveillance of patients prescribed olanzapine, to identify any untoward iatrogenic haematological abnormalities or immunosuppression.
Key words: Antipsychotic agents; Neutropenia; Schizophrenia; Thrombocytopenia
Introduction
Olanzapine is a commonly used second-generation antipsychotic (serotonin dopamine agonist) of the thienobenzodiazepine class.1 It is a dibenzodiazepine derivative. As such, it bears structural and functional similarities to clozapine.2 Clozapine is widely known to cause bone marrow haemotoxicity and agranulocytosis.3
Pre-marketing clinical trials of olanzapine did not demonstrate any evidence of agranulocytosis or haemotoxicity.2 Nonetheless case reports have emerged where olanzapine was also associated with haematological abnormalities.4-6 We share an interesting case of olanzapine- induced haematological abnormality, and discuss its postulated causative mechanisms and implications for management.
Case Report
A 50-year-old Chinese, single, and currently unemployed male presented with a 7-year history of abnormal behaviour. He experienced persecutory and bizarre delusions regarding wolves biting him and removing pus from his body. This was accompanied by tactile hallucinations and commanding second-person auditory hallucinations. There were also periods of disorganised behaviour and an insidious onset of concomitant negative symptoms. As a consequence he suffered tremendous occupational and interpersonal dysfunction, losing his job, and being evicted from his rented house.
There were no mood or neurotic symptoms and no history suggestive of cognitive impairment, substance abuse, or organic illness. There was no family history of mental illness. Personal history revealed a premorbid solitary, introverted personality type but no perinatal or childhood insults.
Mental state examination demonstrated auditory, functional, extracampine, and tactile hallucinations. He also experienced bizarre and persecutory delusions. His mood was euthymic and there were no features on examination suggestive of bipolar disorder or depressive illness. He had no cognitive deficits but poor insight regarding his illness. Physical examination was unremarkable.
A diagnosis of schizophrenia, single episode, currently acute episode was made as per the DSM-5 criteria. Prior to starting medications, a full blood count was taken that was unremarkable except for a slightly low haemoglobin (Hb) level of 7.63 mmol/L. Total white count (TW) was 4.33 x 109/L and platelet count being 238 x 109/L (Table). He was initially commenced on risperidone (optimised to 6 mg/day) that failed to ameliorate his symptoms. Olanzapine was then started as an alternative antipsychotic agent and risperidone was stopped abruptly.
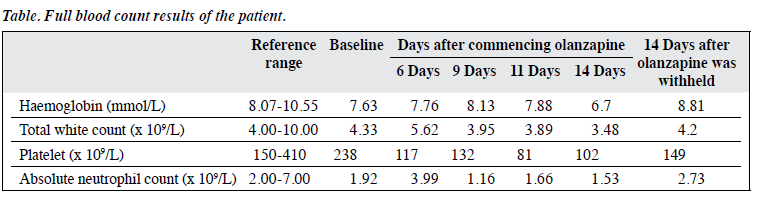
The platelet count dropped to 117 x 109/L after 6 days of olanzapine treatment. Nonetheless the patient demonstrated no signs of infection and no bleeding tendency. Closer full blood count monitoring was initiated. At day 9, he became neutropenic with lowest absolute neutrophil count of 1.16 x 109/L. Platelet count reached a nadir at day 11 (81 x 109/L). The Hb level and TW further dropped to 6.7 mmol/L and 3.48 x 109/L at day 14, respectively (Table).
Olanzapine was withheld and aripiprazole commenced. Over the next 2 weeks his counts gradually normalised, returning to normal 14 days after withholding olanzapine.
Throughout this process there were no clinical signs of infection, inflammation, or insidious malignancy. There was no evidence of Lewy body dementia as no Parkinsonism or fluctuating consciousness was evident. Neither the Mini-Mental State Examination nor Montreal Cognitive Assessment were pathologically altered (29/30 and 28/30 respectively) and B12 and folate levels were within normal range. Electrocardiography showed normal sinus rhythm and renal and thyroid function tests were not pathologically altered.
Further investigations to elucidate the cause of the unexplained haematological abnormality suggested no alternative explanations. The potential differentials considered included any occult malignancy, a haematological disease, or an infective process. His full blood picture merely suggested that platelets were reduced but with no clumping.
Serological screening indicated an incidental chronic hepatitis B infection, but liver function tests suggested no impairment (reactive hepatitis B e antibody, hepatitis B e antigen, and hepatitis B core immunoglobulin M antibody not detected). A liver ultrasound demonstrated cholelithiasis. Tumour marker screening (alpha-fetoprotein, CA 19-9, CA 125, and prostate-specific antigen) was negative. Computed tomographic brain scan demonstrated an old infarct in the left midbrain but no acute bleed. Magnetic resonance imaging of the brain was not done as there were no neurological findings. Cerebrospinal fluid examination, bone marrow aspiration, and trephine biopsy were not performed as there were no clinical symptoms to justify an invasive procedure.
Discussion
Throughout the period of monitoring, the patient demonstrated haematological abnormalities including neutropenia, leukopenia, thrombocytopenia, and anaemia (Table).
Pancytopenia occurred on days 11 and 14 after initiation of olanzapine. Depletion of all other cell lines showed inconsistent timing. Throughout the admission, the only consistent features following 9 days of olanzapine treatment were thrombocytopenia, leukopenia, and neutropenia. Throughout the 14 days of olanzapine treatment, leukopenia was borderline with values almost approaching a normal range. The 2 significant and persistent haematological abnormalities were thrombocytopenia and neutropenia.
In order to determine a causative relationship between agranulocytosis or neutropenia and a medication, several conditions must be fulfilled4: (i) the drug must have been prescribed for 10 days prior to the first symptoms of a haematological reaction (challenge); (ii) the patient recovers on discontinuation of therapy (dechallenge); (iii) there is only 1 possible cause of the haematological reaction; (iv) the patient has not received cytostatic drugs, immunosuppressive agents, or radiotherapy in the 6 weeks prior to onset of the blood disorder; and (v) no systemic disease exists that could have given rise to the neutropenia.
The patient certainly developed thrombocytopenia and neutropenia within a week of commencement of olanzapine, with converse improvement in cell counts upon cessation. History, physical examination, and radiological and blood investigations were unable to ascertain any other causes of this derangement. His incidental finding of pre-existing hepatitis B was not accompanied by any liver impairment that would suggest it was to blame for the derangement.
Eleven case reports in the literature suggest that this is not an isolated case.5,6 There are a number of postulations as to the means by which olanzapine may induce neutropenia. One is that it may modulate levels of granulocyte colony- stimulating factor (G-CSF).7 The G-CSF is noted to be involved in granulocytopoiesis and it is expressed at enhanced levels during increased granulocyte counts. In clozapine- and olanzapine-induced granulocytopenia, G-CSF was not detectable in plasma.8 Although an exact mechanism of interaction between olanzapine and G-CSF is not clear, there may be a correlation that warrants further study.
The second mechanism postulated is based on a mechanism by which clozapine induces neutropenia, i.e. through the formation of nitrenium cations that are catalysed by the flavin-containing monooxygenase-3 system of leukocytes.9 Although olanzapine is classified as a thienobenzodiazepine, its similar chemical structure and pharmacological profile to clozapine may indicate its mechanism of action in inducing neutropenia is similar to that of clozapine. This nitrenium ion may bind to essential cellular proteins and disrupt neutrophil function.9
Alternatively it may act as a hapten, initiating an immune reaction that results in immune-mediated destruction of the neutrophil.9
A third mechanism is postulated in the specific example of patients with schizophrenia and co-morbid substance use disorder. Several case reports as well as a surveillance study reported neutropenia in patients on olanzapine due to use of cocaine or heroin contaminated with levamisole (ergamisol), a hydrochloride salt with antihelminthic and immunomodulatory properties.10
Blood counts have been shown to recover upon olanzapine withdrawal.5,6 In addition G-CSF administration11 and medications such as lithium12 have been shown to help reverse the neutropenia by stimulating G-CSF and elevating serum cortisol levels.
Conclusion
Despite limited evidence to suggest olanzapine induces thrombocytopenia or neutropenia, clinicians need to be mindful of these possible iatrogenic sequelae when initiating such treatment. It is imperative that blood counts be monitored at regular intervals to ensure it is not undiagnosed by omission.
Declaration
The authors have disclosed no conflicts of interest in this study.
References
- Stahl SM. Stahl’s essential psychopharmacology, neuroscientific basis and practical applications. 4th ed. Cambridge: Cambridge University Press; 2013.
- Fulton B, Goa KL. Olanzapine. A review of its pharmacological properties and therapeutic efficacy in the management of schizophrenia and related psychoses. Drugs 1997;53:281-98.
- Alvir JM, Lieberman JA, Safferman AZ, Schwimmer JL, Schaaf JA. Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med 1993;329:162-7.
- Buchman N, Strous RD, Ulman AM, Lerner M, Kotler M. Olanzapine- induced leukopenia with human leukocyte antigen profiling. Int Clin Psychopharmacol 2001;16:55-7.
- Benedetti F, Cavallaro R, Smeraldi E. Olanzapine-induced neutropenia after clozapine-induced neutropenia. Lancet 1999;354:567.
- Teter CJ, Early JJ, Frachtling RJ. Olanzapine-induced neutropenia in patients with history of clozapine treatment: two case reports from a state psychiatric institution. J Clin Psychiatry 2000;61:872-3.
- Pollmächer T, Fenzel T, Mullington J, Hinze-Selch D. The influence of clozapine treatment on plasma granulocyte colony-stimulating (G-CSF) levels. Pharmacopsychiatry 1997;30:118-21.
- Schuld A, Kraus T, Hinze-Selch D, Haack M, Pollmächer T. Granulocyte colony-stimulating factor plasma levels during clozapine- and olanzapine-induced granulocytopenia. Acta Psychiatr Scand 2000;102:153-5.
- Malhotra K, Vu P, Wang DH, Lai H, Faziola LR. Olanzapine-induced neutropenia. Ment Illn 2015;7:5871.
- Vagi SJ, Sheikh S, Brackney M, Smolinske S, Warrick B, Reuter N, et al. Passive multistate surveillance for neutropenia after use of cocaine or heroin possibly contaminated with levamisole. Ann Emerg Med 2013;61:468-74.
- Duggal HS, Gates C, Pathak PC. Olanzapine-induced neutropenia: mechanism and treatment. J Clin Psychopharmacol 2004;24:234-5.
- Focosi D, Azzarà A, Kast RE, Carulli G, Petrini M. Lithium and hematology: established and proposed uses. J Leukoc Biol 2009;85:20-8.


