East Asian Arch Psychiatry 2017;27:97-105
ORIGINAL ARTICLE
Ms Sanku Jalla Sangeeta, MA, Department of Psychiatric Social Work, Central Institute of Psychiatry, Ranchi, Jharkhand, India.
Mr K. J. Mathew, MSW, MPhil, Department of Psychiatric Social Work, Central Institute of Psychiatry, Ranchi, Jharkhand, India.
Address for correspondence: Mr K. J. Mathew, Department of Psychiatric
Social Work, Central Institute of Psychiatry, Ranchi, India. Tel: (91)
9709288932; Email: mathewkunnath@gmail.com
Submitted: 11 November 2016; Accepted: 5 May 2017
Abstract
Introduction: Understanding and perceptions about mental illness vary among individuals based on their experience with the illness or their contact with the people affected by it. These may be further influenced by the individuals’ sociocultural background. This study aimed to understand the differences in the beliefs about, understanding of, and explanations for mental illness between different population groups of Jharkhand, India.
Methods: During July 2014 to February 2016, we recruited the following 3 groups of individuals aged between 18 and 60 years: individuals with mental illness (group 1, n = 240), relatives of individuals with mental illness (group 2, n = 240), and the general public (group 3, n = 240). Qualitative and quantitative findings were combined in this study, and participants were asked about their beliefs about, understanding of, and explanations about mental illness.
Results: Individuals with mental illness and their relatives shared similar beliefs whereas the general public held a different opinion in various domains. There were significant differences among all groups in their understanding of various aspects of mental illnesses including the definition, causes, signs and symptoms, treatment, and outcomes.
Conclusion: Individuals’ perception towards different aspects of mental illness varies, despite they are sharing the same sociocultural milieu. Differences in beliefs, understanding, and explanations may lead to conflicts in treatment goals and expectations, and hamper the intervention strategies that promote mental health and patient care. Focused strategies to develop uniformity in beliefs and explanations about various aspects of mental illness may help to develop collaboration with different community groups that may in turn help in developing effective interventions and treatment.
Key words: Attitude to health; India; Mental disorders
Introduction
Mental illness is the result of many complex mechanisms. Presentation of symptoms, cause, treatment, progress, and prognosis vary from case to case. It is difficult for an individual to understand various aspects of mental illness when he / she have such disease, or when witnessing it in a relative or observing it as a third party. Based on their culture, education and experiences, different individuals view mental illness in different ways. They will offer various explanations for a mental illness such as brain disorder, psychological disturbance, weakness of mind, possession by a spirit / evil spirit, an illness, or a behavioural problem. Based on their belief the attribution differs and so does the model of illness that explains these phenomena, no matter these are due to internal or external forces. Previous studies have identified many common beliefs about the cause of mental illness including a curse or punishment by God, being possessed by a divine or evil spirit or ghost, black magic, evil eye, astrological problems, bad deeds in the previous life, and sexual problems.1-14
People often believe inappropriate conversation, hallucinatory behaviour, and wandering to be the symptoms of mental illness. Psychotic disorders are usually considered to be mental illness while non-psychotic mental illnesses often remain under-recognised by cultural explanations. When mental health practitioners are not sensitive to the explanatory models of the individual, there is a high chance that the illness will remain unrecognised.15-18 An in-depth understanding of various sociocultural aspects and socio- economic scenarios is important to develop effective strategies to address mental health issues.
Individuals with mental illness often cannot understand what has happened to them. In cases of psychotic illness, denial prevails. Studies of common mental disorders, however, have reported different findings. Patients with depression, anxiety, and somatoform disorder attribute their illness to psychosocial and organic factors and have high levels of stigma.7,16 In other studies, people were reported to be resistant to biomedical or psychological models and attributed mental illness to spiritual or supernatural causes.19,20 Hence there is a need for more studies.
The relatives of an individual with mental illness are more concerned about the associated social stigma. They feel that the illness should remain a private matter for the sake of the family. The explanatory models and stigma have been found to be associated in many studies. Often, an individual will not wish to be identified as a relative of a family member with mental illness. This significantly affects treatment and help-seeking behaviour. Studies report high levels of psychological distress among the relatives of individuals with mental illness but help is not sought for fear of stigma and a lack of awareness. The relatives often consider mental illness as more severe than a chronic physical illness such as cancer and express feelings of loss and guilt.4,10,13,21-26
Among the general public there is a general fear of interaction with a mentally ill person whom they consider to be dangerous. Members of the general public rarely initiate any contact with the mentally ill individuals because of their abnormal behaviour; hence they fail to try and understand their problem. On the other hand, cultural beliefs and attributions play a significant role in forming an individual’s beliefs and attitude towards mental illness in both developed and developing countries.13,27,28
Although many studies have been conducted to understand individuals with mental illness in different populations, the explanatory models of different sections of the same population were rarely reviewed and compared. Jharkhand is a state in the north of India with a population of around 33 millions. It is one of the least developed states in India. The health and mental health utility rates are very poor in this region although the underlying reasons are unclear and few studies have been carried out in this area.29-34
Any study in the community is very difficult in Jharkhand because of local Naxal extremists and the lack of transport to remote areas. This limits the ability of an outsider to carry out any study in the Naxal-affected areas.29-32
The current study aimed to understand the different beliefs about, understanding of, and explanations associated with mental illness among individuals based on their own experience and contact with a mentally ill person. The experience or observation of mental illness as a sufferer, being close to a sufferer, or being an outsider or an unrelated individual may result in differences in understanding of the illness, even though they share the same sociocultural environment.
Methods
This was a community-based cross-sectional study conducted in the Hazaribagh district of Jharkhand state in India; Hazaribagh district has a total population of approximately 1.7 millions, including 1.2 millions of adults.35,36 The researchers are engaged in community- based psychiatric service in collaboration with various governmental and non-governmental organisations. They were helped by Nav Bharat Jagriti Kendra (NBJK), an organisation supporting various disadvantaged people. The NBJK shares a database of more than 1400 individuals with mental illness in the Hazaribagh district. This helped the research team to identify individuals with mental illness and their relatives. Although most patients with a diagnosis of chronic mental illness had conditions such as schizophrenia and mood disorders, specific details of the diagnoses were not available.
Because of the local Naxalite issues and inadequate transport facilities, we limited our data collection to those areas with a high concentration of individuals with mental illness by using convenient sampling. During July 2014 to February 2016, we recruited the following 3 groups of individuals who were aged between 18 and 60 years:
- Group 1: Individuals with mental illness diagnosed by a registered psychiatrist and who agreed to participate without the interference of psychopathology.
- Group 2: Individuals who were related to a person with mental illness through blood relationship or marriage, and who had been living with such person for the last 2 years.
- Group 3: Individuals with no personal history of any kind of mental illness, no family history of mental illness in first-degree relatives, and who were in contact but not resident with a mentally ill person. This group was selected from the same locality as groups 1 and 2, and had knowledge of the illness of their neighbour.
Individuals with any kind of severe physical illness or disability, mental retardation, or developmental disabilities were excluded from all groups.
This study combined qualitative and quantitative research, and enquired the participants about their beliefs about, understanding of, and explanations about mental illness. Power calculations suggested a sample size of 240 participants per group based on the assumptions of 1.2 millions of adult population with an expected prevalence of mental illness of 20% (power = 0.95; alpha = 0.05).37
Data were collected from individual respondents at home. Once identified, a detailed explanation about the purpose of the study was provided to individuals. Socio-demographic details were recorded using a semi- structured questionnaire based on the guidelines given by Kleinman.1,2 A group of postgraduate social work student volunteers helped with data collection. They were given training to record the data. Respondents were asked open- ended questions and their responses recorded verbatim. The researchers analysed and categorised the data based on different themes. The categories were then numerically coded and used for quantitative analysis. Data analysis was performed using the Statistical Package for the Social Sciences (SPSS Windows version 16.0; SPSS Inc., Chicago [IL], US). Frequencies, percentages, and Chi-square test were used for comparing data among the 3 groups.
This study was approved by Ethics Committee of Dr Guislain Svastha Education Trust, Ranchi. All participants provided written informed consent.
Results
Socio-demographics of the Respondents
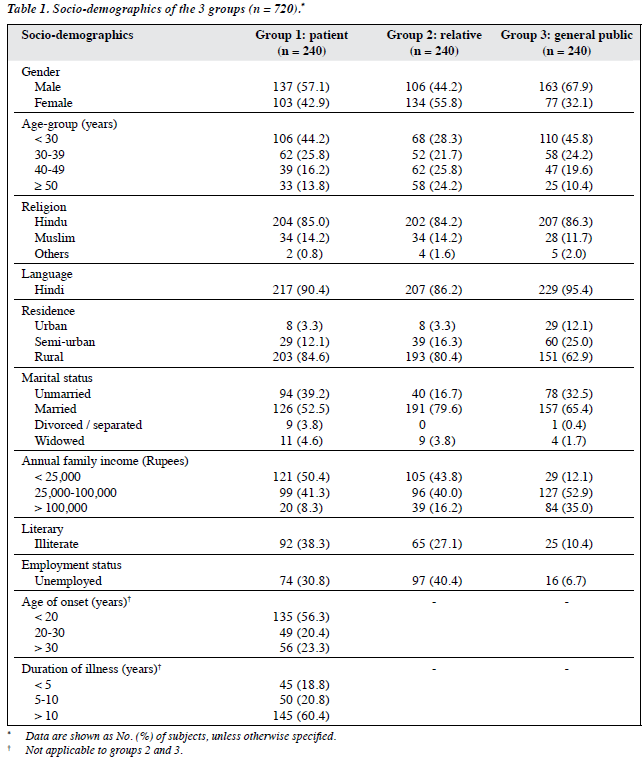
Table 1 shows the socio-demographic details of the 3 groups. Except in the relatives (group 2), most respondents were male. Among all groups, the largest number of respondents were Hindi-speaking Hindus aged below 30 years; the majority of the respondents belonged to a rural nuclear family. The socio-economic conditions of general public (group 3) were better than those of the other groups.
A majority of patients (group 1) were aged below 20 years at the onset of mental illness, and had been ill for more than 10 years.
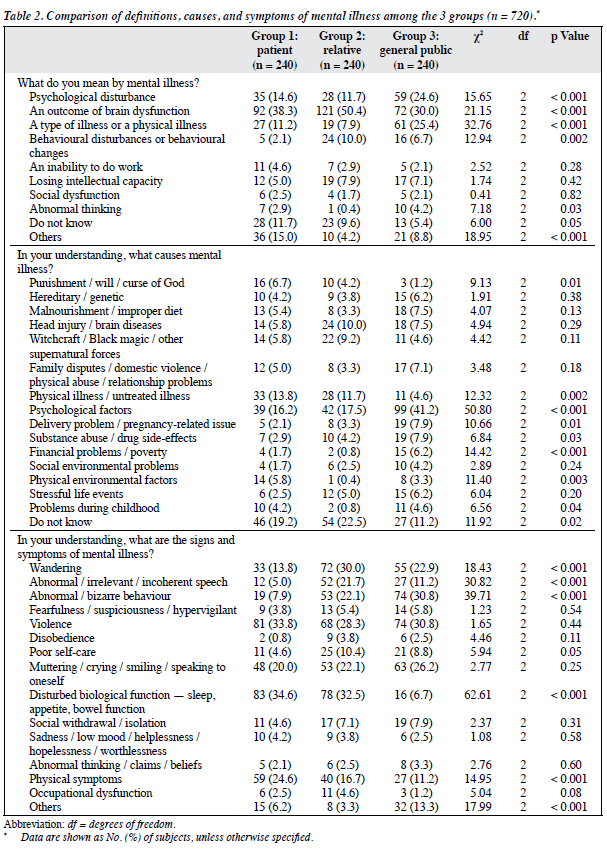
As there were many explanations and opinions in each category, only the most popular items in the description of the results were presented. These included definitions, causes, and symptoms of mental illness (Table 2); effects of mental illness on an individual and his / her family (Table 3); and the treatment and outcome (Table 4).
Definition of Mental Illness
Among the 3 groups, 30% to 50% of respondents believed mental illness to be due to brain dysfunction; these formed the largest proportion of respondents in each group. This was followed by believing mental illness was a psychological disturbance by patients (group 1) and relatives (group 2), although a higher percentage of respondents held such belief in the general public (group 3). The second largest group of respondents in the general public considered mental illness to be a type of illness. Compared with the other groups, fewer respondents in relatives considered mental illness to be an illness. On the other hand, respondents in this group were more likely to consider mental illness a behavioural disturbance. Some respondents, mostly patients, said they did not know the answer (Table 2).
Causes of Mental Illness
Approximately 20% of respondents in patients (group 1) and relatives (group 2) did not know the cause of mental illness; these formed the largest proportion in both groups. Among the 3 groups, most attributed mental illness to psychological factors. Compared with the general public (group 3), more patients and relatives attributed mental illness to physical illness and superstitious attributions. Compared with the other groups, more respondents in the general public considered pregnancy-related issue, substance abuse, poverty, and problems during childhood as the causes of mental illness. More patients attributed physical environmental factors as the cause of mental illness than the other groups (Table 2).
Signs and Symptoms of Mental Illness
Approximately one-third of patients (group 1) and relatives (group 2) cited biological disturbances and violence as symptoms of mental illness; this forms the largest proportion of respondents in both groups. A higher proportion of relatives considered wandering and abnormal / irrelevant / incoherent speech as signs of mental illness than the other groups. Abnormal / bizarre behaviour was mentioned by more respondents in the general public (group 3) than the other groups (Table 2).
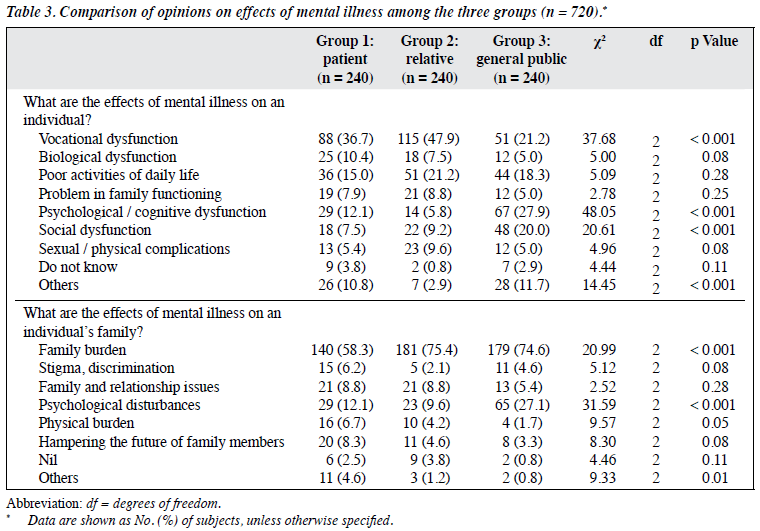
Effects of Mental Illness on an Individual’s Life
The largest number of patients (group 1) and relatives (group 2) believed job-related issues were the major effect of mental illness, followed by impaired ability to carry out day-to-day activities. The largest number of general public (group 3) considered psychological / cognitive dysfunction as the main effect, followed by job-related issues. Compared with the other 2 groups, more respondents in the general public considered psychological / cognitive dysfunction and social dysfunction were the effects on an individual with mental illness (Table 3).
Effects of Mental Illness on an Individual’s Family
Majority of respondents in all groups considered family burden to be the main effect of mental illness on a family, followed by psychological disturbances. Relatives (group 2) gave the largest number of responses to family burden whereas patients (group 1) were the least likely to identify this effect. Compared with the other groups, a higher proportion of the general public (group 3) considered psychological disturbances to be the main effect of mental illness on a family (Table 3).
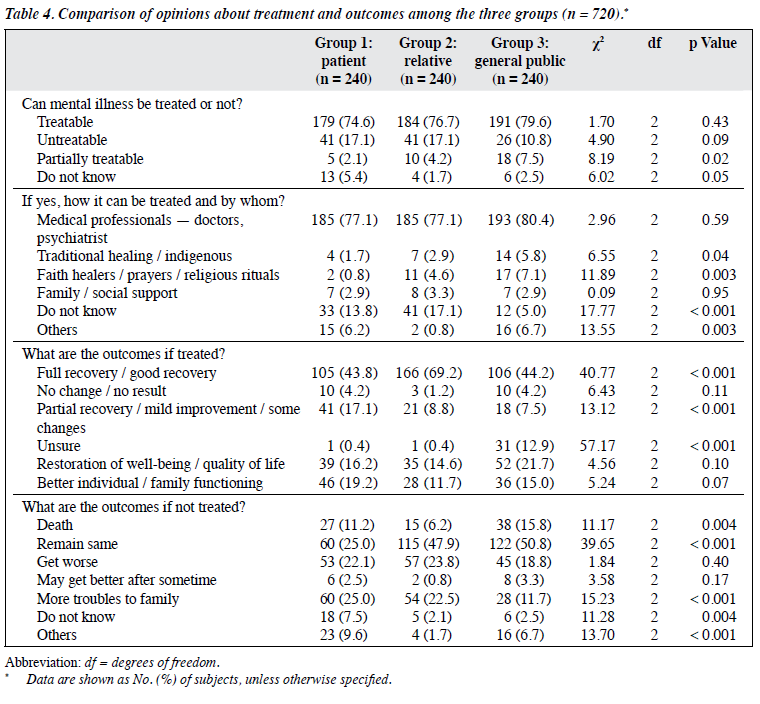
Treatment of Mental Illness
Table 4 shows the majority of respondents in all groups believed that mental illness could be treated, and recognised that this could be treated by medical professionals. Certain respondents from all groups also mentioned that they did not know the right person to approach for treatment, with a higher proportion in patients (group 1) and relatives (group 2).
Outcomes if Treated and Left Untreated
Nearly half of the patients (group 1) and general public (group 3) believed full or good recovery could be attained if treated. Relatives (group 2) appeared to be more optimistic than the other groups as almost 70% held such belief. Restoration of well-being / quality of life and better individual / family functioning were the other themes related to positive outcomes if mental illness was treated. On the other hand, most respondents in all groups expected the illness to remain unchanged if left untreated. Compared with the other groups, a higher proportion of patients also thought that untreated mental illness would cause more problems for the family. Approximately 20% of respondents from all groups felt the illness would get worse if left untreated.
Discussion
There are many definitions of mental illness, and most cite it as brain dysfunction, psychological disturbance, behaviour disturbances or behavioural change, or consider it a type of illness or physical illness. Patients, relatives, and the general public have their own definitions about mental illness. Contrary to many previous studies, the present study identified few superstitious, cultural, or religious definitions of mental illness.7-9,12,14,38 Nevertheless, there were many superstitious and religious explanations for the causes of mental illness. Respondents from all groups mostly considered biopsychosocial aspects to define mental illness but the explanations clustered among diverse attributions in all 3 groups. It also appears that the definitions led to traditional and superstitious explanations as the cause. The largest number of respondents from patients (group 1) and relatives (group 2) reported that they did not know the cause of mental illness. The medical model, especially the neurochemical changes explained by the treating team during psycho-education and awareness programmes, may account for the higher number of biological model explanations among patients and relatives. At the same time a lack of emphasis on broad psychosocial aspects was obvious from the responses. Among practitioners, some believe that a biological model of illness is helpful in reducing stigma although studies reported to date offer no evidence to support such a belief.39,40 A better understanding of biopsychosocial perspectives of mental illness may help individuals to consider such factors during various phases of a mental illness.
An understanding of the signs and symptoms of mental illness changed according to an individual’s experience and contact with mental illness. The theme and number of responses significantly varied as many problems mentioned by the respondents from a group were not considered by other groups in the same proportion. Various studies have reported that individuals usually consider severe mental illness to be psychosis, and mood disorders to be mental illness. The symptoms of neurotic spectrum disorders may not be considered related to mental illness by the general public since such symptoms are not visible to others.18 The usual portrayals of mental illness in the media and that evidenced by mentally ill people seen in public places mostly concern psychosis and mood disorders. This may explain why there was a higher agreement among all groups that violence and hallucinatory behaviour are symptoms of mental illness. The general public was mostly unaware of many of the problems mentioned by patients and relatives such as biological disturbances and physical problems. In line with many previous studies, the general public was more concerned about abnormal or bizarre behaviours compared with the other groups. They also thought that an individual with mental illness might not be able to function appropriately on a day-to-day basis and may become dangerous to others.13 Wandering, abnormal speech, and behavioural abnormalities were considered symptoms by a smaller proportion of patients, suggesting that the sufferer might not understand many of the symptoms of mental illness. The physical complaints reported by patients were noticed less by the other groups. This suggests that genuine physical problems of individuals with mental illness are ignored, and hence needs to be specifically addressed.
The majority of respondents expected the worst outcome of mental illness to be job-related problems or an increased burden on the family. This might be because only a small proportion of individuals with mental illness were employed and family members often complained about their difficulties in maintaining day-to-day life.41 Compared with relatives and the general public, fewer respondents from the patient group recognise the family burden. On the other hand, some important problems mentioned by patients and relatives, such as an impaired ability to maintain day-to- day activities and biological dysfunctions, went unnoticed by the general public. Nonetheless problems in social and interpersonal areas and psychological or cognitive dysfunction were noticed. The sexual problems reported by many relatives remained unnoticed by patients and the general public. The responses justified the context of their experience and observation of mental illness.
Previous studies have reported both positive and negative attitudes of patients and the general public towards modern treatments for mental illness. Some studies reported that subjects prefer traditional and faith-healing methods and place little trust in medical treatments.9-16 Contrary to this, other studies reported that individuals were aware of and had a positive view of medical treatment for mental illness, similar to the present study.7,10,12,14,17 The general public who had least exposure to mental illness showed more positive responses. This may be because they have had no personal experience of mental illness and its effects and believe it can be treated like any other physical illness. Patients were the least optimistic of treatment among all groups. The long duration of treatment and a lack of expected outcomes may make them less motivated. Compared with the general public, more patients and relatives did not know the appropriate facility to treat mental illness. This may have been due to disappointment with previously tried methods and poor outcomes of treatment although this requires further clarification.
A majority of respondents expected a positive outcome from the treatment of mental illness. Many patients, however, expected only a partial recovery and some of the general public remained unsure. Relatives had knowledge of the patient before and after the development of a mental illness and its treatment. Such knowledge may have helped them to be more optimistic about positive outcomes of treatment. The general public usually observe the illness from keeping themselves outside the purview. The relief from difficulties after treatment for mental illness may make the individuals more optimistic. Patients often do not remember clearly about their psychotic episodes. This may explain their varied responses in many domains when compared with others. Approximately half of the respondents in the relatives and general public expected the illness to remain unchanged if left untreated, but only a quarter of the patients felt the same. The patients and relatives shared a similar response to the outcome of mental illness if left untreated such as getting worse and cause more trouble to the family.
This study had some limitations. The use of convenient sampling and because of a lack of time, security issues, and other constraints such as money and manpower, this study was confined to a particular district of Jharkhand, hence this limits the generalisability of findings. Ongoing treatment may have altered various beliefs and explanations as well as trust in modern medicine. Individuals who defaulted from or did not seek treatment may have different explanatory models. The present study used mixed techniques of qualitative and quantitative research. Some information might have been lost while transmitting the response or data. Isolated findings might also have been ignored because of small numbers. Factors associated with the socio-demographic profile of the respondents might not have been addressed in this study. Due to technical limitations, the present study was not specific to clinical diagnoses and there may be a relationship between the diagnoses and study variables. The study cannot explain the specific factors related to the development of particular belief models and explanations and the findings make no inference about the dynamics of beliefs and explanations. Future studies may focus on factors associated with the origin and changes to the models over time so that well- focused intervention strategies can be devised. Interventions need to be developed to address the issues associated with sociocultural factors without offending the community. There is a need for more research to understand how to develop healthy collaboration with the community and to bring a positive change in this regard.
Conclusion
The present study found that the respondents recognised mental illness as a problem of the brain, mind, behaviour, or body. The causes were explained in a more diverse way and included superstitions although most individuals considered various factors in the biopsychosocial context. There were differences in many domains in understanding the signs and symptoms as a sufferer and an observer. The responses indicated that people mostly understand psychotic symptoms as symptoms of mental illness, but they lack knowledge about other mental health problems. All 3 groups differed significantly in their view of the consequences of the illness. The preferences for and expected outcomes of treatment also varied. Overall, patients and relatives shared more similar responses in many domains compared with the general public. Considering mental health in a broader perspective, it is important for various roles in the community to work together to achieve favourable outcomes. Uniformity in beliefs, and explanation and understanding of mental illness play significant roles. Differences in and conflict between models of belief and explanations may hamper strategies to promote mental health and quality care to patients. In this way the present study indicates the need for more research to understand the issues in order to devise collaborative and focused interventions to create favourable attitudes and understanding about mental illness in the community. Such strategies may help mental healthcare practitioners and organisations to plan and implement various community- based mental health programmes. The findings may have implications for generating awareness, involving families and communities in psychosocial management in an effective way, managing stigma, providing support, and forming policy.
Acknowledgements
We thank all the participants and Nav Bharat Jagriti Kendra for their support and cooperation to complete this study. We also thank Prof. KS Jacob, Department of Psychiatry, Christian Medical College, Vellore, India for helping with the study design; and our batch mates and friends for data collection.
Declaration
All authors have disclosed no conflicts of interest.
References
- Kleinman A, Eisenberg L, Good B. Culture, illness and care: clinical lessons from anthropologic and cross-cultural research. Annals of Int Med 1978;88:251-8.
- Kleinman A. Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. Berkeley, Los Angeles and London: University of California Press; 1981.
- Saravanan B, Jacob KS, Johnson S, Prince M, Bhurga D, David AS. Belief models in first episode schizophrenia in South India. Soc Psychiatry Psychiatr Epidemiol 2007;42:446-51.
- Charles H, Manoranjitham SD, Jacob KS. Stigma and explanatory models among people with schizophrenia and their relatives in Vellore, South India. Int J Soc Psychiatry 2007;53:325-32.
- Minas H, Klimidis S, Tuncer C. Illness causal beliefs in Turkish immigrants. BMC Psychiatry 2007;7:34.
- Adewuya AO, Makanjuola RO. Lay beliefs regarding causes of mental illness in Nigeria: pattern and correlates. Soc Psychiatry Psychiatr Epidemiol 2008;43:336-41.
- Girma E, Tesfaye M. Patterns of treatment seeking behavior for mental illnesses in Southwest Ethiopia: a hospital based study. BMC Psychiatry 2011;11:138.
- Kishore J, Gupta A, Jiloha RC, Bantman P. Myths, beliefs and perceptions about mental disorders and health-seeking behavior in Delhi, India. Indian J Psychiatry 2011;53:324-9.
- Kate N, Grover S, Kulhara P, Nehra R. Supernatural beliefs, aetiological models and help seeking behaviour in patients with schizophrenia. Ind Psychiatry J 2012;21:49-54.
- Girma E, Tesfaye M, Froeschl G, Möller-Leimkühler AM, Müller N, Dehning S. Public stigma against people with mental illness in the Gilgel Gibe Field Research Center (GGFRC) in Southwest Ethiopia. PLoS One 2013;8:e82116.
- Patra BN, Grover S, Aggarwal M, Avasthi A, Chakrabarti S, Malhotra S. Explanatory models in patients with obsessive compulsive disorder: an exploratory study. Indian J Soc Psychiatry 2013;29:38-45.
- Schoonover J, Lipkin S, Javid M, Rosen A, Solanki M, Shah S, et al. Perceptions of traditional healing for mental illness in rural Gujarat. Ann Glob Health 2014;80:96-102.
- Poreddi V, BIrudu R, Thimmaiah R, Math SB. Mental health literacy among caregivers of persons with mental illness: a descriptive survey. J Neurosci Rural Pract 2015;6:355-60.
- Iheanacho T, Kapadia D, Ezeanolue CO, Osuji AA, Ogidi AG, Ike A, et al. Attitudes and beliefs about mental illness among church-based lay health workers: experience from a prevention of mother-to-child HIV transmission trial in Nigeria. Int J Cult Ment Health 2016;9:1-13.
- Abbo C, Ekblad S, Waako P, Okello E, Musisi S. The prevalence and severity of mental illnesses handled by traditional healers in two districts in Uganda. Afr Health Sci 2009;9 Suppl 1:S16-22.
- Sorsdahl KR, Flisher AJ, Wilson Z, Stein DJ. Explanatory models of mental disorders and treatment practices among traditional healers in Mpumalanga, South Africa. Afr J Psychiatry (Johannesbg) 2010;13:284-90.
- van der Ham L, Wright P, Van TV, Doan VD, Broerse JE. Perceptions of mental health and help-seeking behavior in an urban community in Vietnam: an explorative study. Community Ment Health J 2011;47:574-82.
- Mbwayo AW, Ndetei DM, Mutiso V, Khasakhale LI. Traditional healers and provision of mental health services in cosmopolitan informal settlements in Nairobi, Kenya. Afr J Psychiatry (Johannesbg) 2013;16:134-40.
- Ward EC, Wiltshire JC, Detry MA, Brown RL. African American men and women’s attitude toward mental illness, perceptions of stigma, and preferred coping behaviors. Nurs Res 2013;62:185-94.
- Chen JA, Hung GC, Parkin S, Fava M, Yeung AS. Illness beliefs of Chinese American immigrants with major depressive disorder in a primary care setting. Asian J Psychiatr 2015;13:16-22.
- Ward EC, Clark le O, Heidrich S. African American Women’s beliefs, coping behaviors, and barriers to seeking mental health services. Qual Health Res 2009;19:1589-601.
- Ahmedani BK, Kubiak SP, Kessler RC, de Graaf R, Alonso J, Bruffaerts R, et al. Embarrassment when illness strikes a close relative: a World Mental Health Survey Consortium Multi-Site Study. Psychol Med 2013;43:2191-202.
- Girma E, Möller-Leimkühler AM, Dehning S, Mueller N, Tesfaye M, Froeschl G. Self-stigma among caregivers of people with mental illness: toward caregivers’ empowerment. J Multidiscip Healthc 2014;7:37-43.
- Ae-Ngibise KA, Doku VC, Asante KP, Owusu-Agyei S. The experience of caregivers of people living with serious mental disorders: a study from rural Ghana. Glob Health Action 2015;8:26957.
- Sintayehu M, Mulat H, Yohannis Z, Adera T, Fekade M. Prevalence of mental distress and associated factors among caregivers of patients with severe mental illness in the outpatient unit of Amanuel Hospital, Addis Ababa, Ethiopia, 2013: Cross-sectional study. J Mol Psychiatry 2015;3:9.
- Svensson B, Hansson L. How mental health literacy and experience of mental illness relate to stigmatizing attitudes and social distance towards people with depression or psychosis: A cross-sectional study. Nord J Psychiatry 2016;70:309-13.
- Olafadottir S, Pescosolido BA. Constructing illness: how the public in eight Western nations respond to a clinical description of “schizophrenia”. Soc Sci Med 2011;73:929-38.
- Stuber JP, Rocha A, Christian A, Link BG. Conceptions of mental illness: attitudes of mental health professionals and the general public. Psychiatr Serv 2014;65:490-7.
- Saxena KB. The naxalite movement and the crisis of governance: reform measures for regaining people’s trust. Social Change 2009;39:475-503.
- Statistics Division, Ministry of Tribal Affairs, Government of India. Statistical profile of scheduled tribes in India 2013. Noida, India: Chaar Dishayen Printers; 2013.
- Odisha, Bihar least developed states, Goa and Kerala top chart: Rajan panel report. The times of India. Available from: http://timesofindia.indiatimes.com/india/Odisha-Bihar-least-developed-states-Goa-and-Kerala-top-chart-Rajan-panel-report/articleshow/23094131.cms. Accessed Oct 2016.
- Ghosh S. Equity in the utilization of healthcare services in India: evidence from National Sample Survey. Int J Health Policy Manag 2014;2:29-38.
- Kumari S, Mishra SN, Chaudhury S, Singh AR, Verma AN, Kumari S. An experience of community mental health program in rural areas of Jharkhand. Ind Psychiatry J 2009;18:47-50.
- National Mental Health Survey of India, 2015-16: Summary. Bengaluru, India: National Institute of Mental Health and Neuro Sciences Bengaluru; 2016. Available from: http://indianmhs.nimhans.ac.in/Docs/Summary.pdf. Accessed 31 Aug 2017.
- Census Organisation of India. Population Census 2011. Available from: http://www.census2011.co.in/census/district/102-hazaribagh.html. Accessed Oct 2016.
- Office of the Chief Electoral Officer, Jharkhand. Systematic voters’ education and electoral participation: state sveep plan 2014, Jharkhand. Available from: http://eci.nic.in/eci_main1/SVEEP/statesweepplan2014/JHARKHAND.pdf. Accessed Oct 2016.
- Math SB, Srinivasaraju R. Indian psychiatric epidemiological studies: Learning from the past. Indian J Psychiatry 2010;52 Suppl 1:S95-103.
- Khoury NM, Kaiser BN, Keys HM, Brewster AR, Kohrt BA. Explanatory models and mental health treatment: is vodou an obstacle to psychiatric treatment in rural Haiti? Cult Med Psychiatry 2012;36:514-34.
- Rüsch N, Todd AR, Bodenhausen GV, Corrigan PW. Biogenetic models of psychopathology, implicit guilt, and mental illness stigma. Psychiatry Res 2010;179:328-32.
- Angermeyer MC, Holzinger A, Carta MG, Schomerus G. Biogenetic explanations and public acceptance of mental illness: systematic review of population studies. Br J Psychiatry 2011;199:367-72.
- Mechanic D, Bilder S, McAlpine DD. Employing persons with serious mental illness. Health Aff (Millwood) 2002;21:242-53.