East Asian Arch Psychiatry 2019;29:41-7 | https://doi.org/10.12809/eaap1808
THEME ARTICLE
Arthur DP Mak, MBChB, FRCPsych (UK), FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, The Chinese University of Hospital, Hong Kong Justin CY Wu, MBChB (CUHK), MRCP (UK), MD (CUHK), FRCP (Edin), FRCP (Lond), FHKAM (Gastroenterology and Hepatology), AGAF, Institute of Digestive Disease, The Chinese University of Hong Kong, Hong Kong
Yawen Chan, BASc, MPhil, M Soc Sci (Clinical Psychology), Institute of Digestive Disease, The Chinese University of Hong Kong, Hong Kong
YK Tse, BSc Statistics (CUHK), MPhil Statistics (CUHK), Institute of Digestive Disease, The Chinese University of Hong Kong, Hong Kong
Sing Lee, MD, FRCPsych (UK), FHKAM (Psychiatry), Department of Psychiatry, The Chinese University of Hospital, Hong Kong
Address for correspondence: Dr Arthur DP Mak, Department of Psychiatry, The Chinese University of Hong Kong, Shatin, Hong Kong. Email: arthurdpmak@cuhk.edu.hk
Submitted: 30 January 2018; Accepted: 26 September 2018
Abstract
Objective: To examine the prevalence and comorbidity of gastro-oesophageal reflux disease (GORD) with generalised anxiety disorder (GAD) and major depressive episodes (MDE) in a general population using DSM-IV, and to evaluate the associations between these conditions and healthcare utilisation. Methods: A random population-based telephone survey was conducted to record frequency of GORD symptoms, symptoms of GAD and MDE based on DSM-IV, and healthcare utilisation.
Results: Of 2011 respondents, 4.2% had weekly GORD and 13.9% had monthly GORD, whereas 3.8% reported GAD and 12.4% reported MDE. Those with monthly GORD had higher risk of GAD (p = 0.01) and MDE (p < 0.001). GORD symptom frequency was independently correlated with MDE and GAD in a dose-response manner. The number of psychiatric diagnoses was independently correlated with GORD. GORD symptom frequency, GAD, and MDE were correlated with consultation frequency. GORD symptom frequency was corelated with high investigation expenditure.
Conclusion: GORD had a strong dose-response relationship with GAD and MDE in a Hong Kong population. Excessive healthcare utilisation should alert clinicians to the risk of psychiatric comorbidity.
Key words: Anxiety disorders; Depressive disorder, major; Gastroesophageal reflux
Introduction
Gastro-oesophageal reflux disease (GORD) is characterised by troublesome reflux symptoms of heartburn and regurgitation as well as complications such as esophagitis.1 In Western populations, 15% to 25% have been reported to have GORD at least weekly.2
Generalised anxiety disorder (GAD) and major depressive episodes (MDE) are the most common mental disorders globally.3 GORD is often associated with anxiety and depression,4 with a bidirectional link.5 However, most evidence is derived from patient samples.5 For example, a study reported association between GORD and mental disorders (such as schizophrenia and major depression) in patients,6 but selection bias may have distorted the association,7 as only 38% of people with GORD seek care.8 In addition, studies on psychiatric comorbidity of GORD have failed to measure mental disorders using standardised diagnostic criteria such as the DSM-IV-TR.9 All population studies on psychiatric comorbidity of GORD used rating scales such as the Hospital Anxiety and Depressive Scale4,8 instead of diagnostic interviews. These symptom rating scales do not capture the clinically relevant symptoms, symptom duration, and functional impairment required for the DSM-IV9 diagnoses of GAD or MDE. Therefore, existing community data do not provide adequate evidence on the association of GORD with mental disorders such as GAD and MDE.
Anxiety and depressive symptoms result in increased healthcare utilisation in GORD.8 Treatment of anxiety and depression may alleviate comorbid gastrointestinal symptoms.10 It remains uncertain how GORD may interact with specific mental disorders, for which effective interventions exist. We conducted a community survey to evaluate the association between GORD of various symptom frequencies and GAD and MDE. Sociodemographic and diagnostic indicators of healthcare utilisation were also investigated.
Methods
This study was approved by the Chinese University of Hong Kong research ethics committee. Verbal consent was obtained from each respondent. The Hong Kong Institute of Asia-Pacific Studies of the Chinese University of Hong Kong was commissioned to conduct a telephone survey about ‘digestive problems and emotional health’ of a random selection of the general population aged 15 to 65 years. Interviews were conducted from 22 April to 13
May 2009. Interviewers were university students with 1 to 3 years of part-time experience in telephone interviews. They were trained on questionnaire administration and skills involved in eliciting symptoms of GORD, GAD, and MDE. Interviews were conducted in Cantonese and took approximately 20 minutes.
Sampling telephone lines should generate a representative sample of households, as >99% of households have a telephone line.11 Phone calls were made in the evening (6-10 pm) to access the working population.
Instrument
A 40-item questionnaire was used to record demographics, frequency of GORD symptoms (troublesome reflux symptoms of heartburn and/or regurgitation over the past 3 months) using the Rome III Classification of Dyspepsia module pertaining to the Montreal definition,1 symptoms of GAD and MDE based on DSM-IV, and healthcare utilisation.
The questionnaire has been used in previous telephone surveys and has reported the 12-month prevalence to be 4.1% for GAD12 and 8.4% for MDE.13 Clinical re-appraisal for diagnoses of MDE and GAD using the Structured Clinical Interview for DSM-IV Axis I Disorders yielded good agreement.14,15 In Hong Kong, the prevalence of Rome III irritable bowel syndrome was reported to be 5.4% and Rome III dyspepsia to be 8%, comparable with overseas estimates.16,17
Respondents were also asked “how much did you spend over the past 5 years on investigations for your gastrointestinal problems?” to assess investigation expenditure and “how frequent did you see a doctor for your health problems” to assess frequency of consultations over the past 5 years. Frequent consulting behaviour was arbitrarily defined as more than monthly consultations; high investigation expenditure was defined as ≥HK$50 000 over the past 5 years, with both indexes representing unusually high levels of healthcare utilisation.
Study power
With an overall sample of 2011, a logistic regression of binary response variable of GORD (monthly) [n = 254, 13.1% GORD (monthly) without GAD] on the binary independent variable of GAD (n = 77, 3.8%), to achieve 80% power at a significance level of 0.05, would have a minimum detectable odds ratio of 2.23.18
Analysis
The study sample was weighted according to age and sex distribution of the Hong Kong general population based on the 2008 Census data.11 The current prevalence of GERD and 12-month prevalence of GAD and MDE were presented as percentages. All variables were put into logistic regression analysis to determine variables that were independent associated with high investigation expenditure (arbitrarily defined as ≥HK$50,000 over the past 5 years) and frequent medical consultations (arbitrarily defined as monthly or more). Statistical analysis was performed using SPSS (Windows version 16; SPSS Inc., Chicago [IL], US). All p values were two-tailed with the significance level at 0.05.
Results
Prevalence
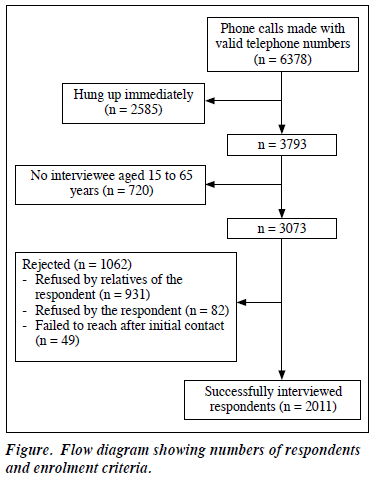
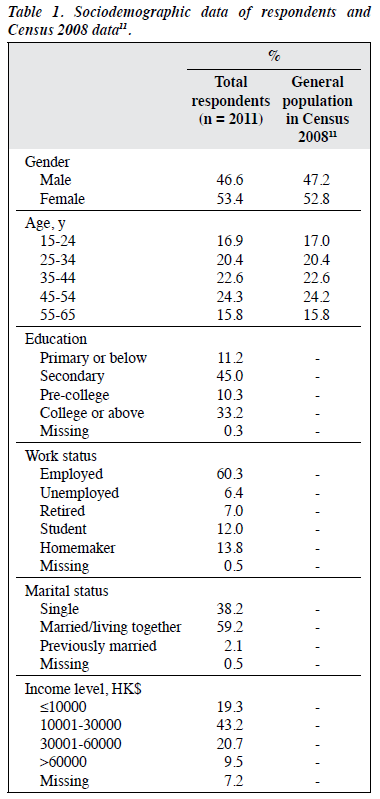
Of the 6378 valid home telephone numbers randomly selected, 2585 hung up immediately, 720 had no interviewees aged 15 to 65 years, and 3073 were successful contacts. Of these contacts, 1062 were turned down by relatives of the respondent (n = 931) or the respondent (n = 82) or contact could not be made to the respondent after initial contact (n = 49) [Figure]. The final sample comprised 2011 respondents (937 men and 1074 women), with a participation rate of 65.4%, which has been reported in a study.19 The age distribution of respondents is comparable to that of the general population in Census 2008 (Table 1).11
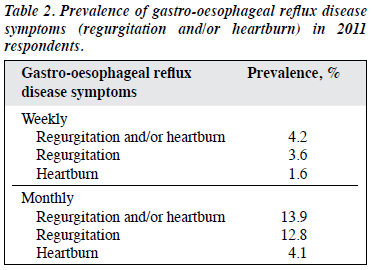
Of the 2011 respondents over the past 3 months, 4.2% and 13.9% reported at least weekly and monthly GORD symptoms, respectively, whereas 3.6% and 12.8% reported at least weekly and monthly regurgitation, respectively; 1.6% and 4.1% reported at least weekly and monthly heartburn, respectively (Table 2). The 12-month prevalence of GAD has previously been reported to be 3.8%, and that of MDE to be 12.4%.16
Comorbidities of GORD
GORD was associated with both GAD and MDE in terms of symptoms and disorder level. MDE was reported more frequently by respondents with regurgitation than by those without (21% vs 10.2%, p < 0.001) and by those with heartburn than by those without (31% vs 11.1%, p < 0.001).
GAD was reported more frequently by respondents with regurgitation than by those without (7.6% vs 2.9%, p < 0.001) and by those with heartburn than by those without (14.7% vs 3.1%, p < 0.001).
On univariate analysis, respondents with either MDE or GAD were more likely to report at least monthly GORD symptoms, and respondents with at least monthly GORD symptoms were more likely to report either MDE or GAD. On multivariate analysis, both GAD and MDE were independently associated with at least monthly GORD symptoms (Table 3).

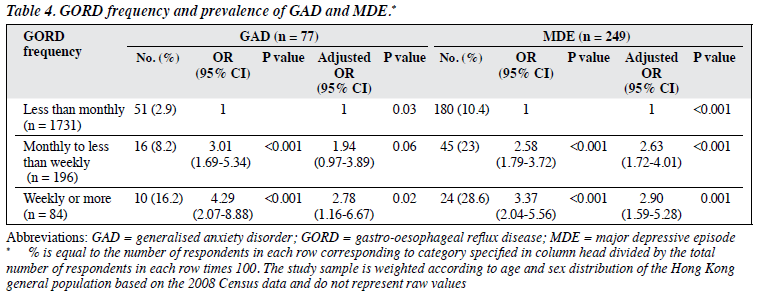
Association with concomitant MDE and GAD
More respondents with both MDE and GAD reported GORD than did those with either or no psychiatric diagnosis (32.1% vs 27.4% vs 11.7%, p < 0.001). On multivariate analysis, respondents with at least monthly GORD symptoms more commonly reported having one or both psychiatric diagnoses, with odds ratios increasing with the number of psychiatric diagnoses (Table 4).
GORD frequency and psychiatric comorbidity
Odds ratios for having GAD and/or MDE increased with GORD frequency in a dose-response manner, even after adjusting for all sociodemographic variables (Table 4).
Frequent medical consultations
Approximately 25% of respondents with at least monthly GORD symptoms reported medical consultations at least once per month over the past year, compared with those without the condition (12.4%). In addition, the proportion of respondents who reported more frequent consultations increased with GORD symptom frequency. Respondents with GAD or MDE also reported more frequent consultations, and the likelihood increased in respondents with both diagnoses. On multivariate analysis, frequent medical consultations were positively associated with at least monthly GORD symptoms, GAD, MDE, both psychiatric diagnoses, GORD frequency, and female sex, whereas frequent medical consultations were negatively associated with work status of respondents (Table 3).
High investigation expenditure
Only 1.4% of respondents spent ≥HK$50,000 in investigation expenditure over past 5 years, but this proportion was overrepresented in those with at least monthly GORD symptoms (especially those with at least weekly symptoms), GAD, having one (but not both) psychiatric diagnosis, those aged 45 to 54 years, and those married/living together with a partner. On univariate analysis, high investigation expenditure was weakly associated with income. On multivariate analysis, high investigation expenditure was associated with at least monthly GORD symptoms, GORD frequency, income, and work status of respondents (Table 3).
Discussion
The participation rate of the present study is comparable to previously reported telephone surveys.15 GORD was found to be strongly associated with GAD and MDE in this random, representative sample using standardised diagnostic criteria. This indicates that the association found in clinical studies is not a consequence of help-seeking bias.
In the present study, GORD was independently associated with MDE and GAD; whereas only symptom scores have been reported previously.4,8 In particular, a dose-response relationship between GORD and GAD or MDE appeared to be bidirectional. This suggests that mental disorders such as GAD and MDE may have different biological correlates (eg, association with serotonin dysfunction, serotonin transporter genetic associations) than the common experience of stress. The association between the pathologies of brain and oesophagus warrants biological and psychosocial research on the mechanisms linking these mental disorders with GORD. In addition, the dose-response relationship suggests a possible causal relationship between GORD and mental disorders, which should be confirmed by longitudinal studies in representative and well-characterised samples. Moreover, the bidirectionality is consistent with the ‘two-way traffic’ of the brain-gut axis. Epidemiological evidence has been found for functional dyspepsia in a population-based cohort study.20 Chronic psychosocial adversities and psychiatric disorders have been associated with reduced pain threshold for reflux symptoms,6,21 altered oesophageal motility,6 and gastric secretion.22 Individuals with depressive and anxiety disorders may tend to feel burdened by more troublesome reflux symptoms.23 The dose-response relationship mirrors evidence from the psychosomatic literature that suggests a dose-response relationship between somatic symptom load and psychopathology.23 Oesophageal acid stimulation has been shown to sensitise the cingulate gyrus and insula to non-painful mechanical stimulations on functional magnetic resonance imaging.24 However, it remains unclear how GORD increases the risk of mental disorders in addition to the anxiety and depressive disorders caused by distress and functional impairment from GORD symptoms.25 There may also be common psychosocial aetiological factors, such as chronic experience of life stress that predisposes individuals to anxiety and depressive disorders as well as GORD.26 This warrants further biopsychosocial research on the bidirectional dynamic in the brain-gut axis in the context of mental disorders.
Our study found unusually high levels of healthcare utilisation. GORD frequency was associated with frequent medical consultations and high investigation expenditure in a dose-response manner. In addition, both GAD and MDE were independently associated with frequent consultations. The lack of correlation between mental disorders and high investigation expenditure could be related to the small proportion of individuals with the extreme level of expenditure arbitrarily selected as a cut-off for the present study. Other possible reasons include more severe occupational impairment from mental disorders that may limit the respondents’ ability to pay as well as reduced motivation and pessimistic tendencies in individuals with MDE that may limit help-seeking behaviour.
Our study has several limitations. First, endoscopy was not performed to confirm erosive or non-erosive diseases and study their disparate relationship with mental disorders. Second, brief telephone surveys were used instead of detailed face-to-face interviews. However, telephone surveys may avoid psychiatric stigma and facilitate disclosure of sensitive information.27 In particular, Chinese people tend to be inhibited about disclosure of psychological distress.28 Third, other potentially important factors associated with GORD were not recorded, such as medication use. However, medication use is unlikely to play a major role in this association, as few respondents with mental disorders had access to treatment.13 Fourth, recall bias and the cross-sectional design limited the study of causality. Prospective illness course studies in the community can better inform causality.20 However, the bidirectional link suggests a complex relationship between mental disorders and GORD. Last, assessment of 12-month prevalence of GAD and MDE may lead to an optimistic result compared with current prevalence of GORD.
Conclusion
GORD is strongly associated with MDE and GAD, with substantial effects on healthcare utilisation. Common anxiety and depressive disorders should be routinely screened when assessing GORD, especially in patients with high healthcare utilisation. Clinicians treating patients with GORD and comorbid GAD or MDE should consider help-seeking behaviour as an important part of the illness experience. Both GAD and MDE respond to psychobehavioural and/or pharmacological therapies. A holistic approach combining gastroenterologists and mental health professionals is recommended.
Disclosure
The authors have no conflicts of interests to disclose.
References
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006;101:1900-20.
- El-Serag HB. Time trends of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol 2007;5:17-26. Crossref
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 2004;291:2581-90. Crossref
- Jansson C, Nordenstedt H, Wallander MA, Johansson S, Johnsen R, Hveem K, et al. Severe gastro-oesophageal reflux symptoms in relation to anxiety, depression and coping in a population-based study. Aliment Pharmacol Ther 2007;26:683-91. Crossref
- Mizyed I, Fass SS, Fass R. Review article: gastro-oesophageal reflux disease and psychological comorbidity. Aliment Pharmacol Ther 2009;29:351-8. Crossref
- Avidan B, Sonnenberg A, Giblovich H, Sontag SJ. Reflux symptoms are associated with psychiatric disease. Aliment Pharmacol Ther 2001;15:1907-12. Crossref
- Haug TT, Mykletun A, Dahl AA. The association between anxiety, depression, and somatic symptoms in a large population: the HUNT-II study. Psychosom Med 2004;66:845-51. Crossref
- Wong WM, Lai KC, Lam KF, Hui WM, Hu WH, Lam CL, et al. Prevalence, clinical spectrum and health care utilization of gastro- oesophageal reflux disease in a Chinese population: a population- based study. Aliment Pharmacol Ther 2003;18:595-604. Crossref
- American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders, 4th Ed. Washington, DC: American Psychiatric Association; 2000.
- Hashash JG, Abdul-Baki H, Azar C, Elhajj II, El Zahabi L, Chaar HF, et al. Clinical trial: a randomized controlled cross-over study of flupenthixol + melitracen in functional dyspepsia. Aliment Pharmacol Ther 2008;27:1148-55. Crossref
- Census and Statistics Department. Hong Kong Statistics. Hong Kong; 2009.
- Johnson T, Owens L. Survey response rate reporting in the professional literature. In: 58th Annual Meeting of the American Association for Public Opinion Research. Nashville; 2003.
- Lee S, Tsang A, Kwok K. Twelve-month prevalence, correlates, and treatment preference of adults with DSM-IV major depressive episode in Hong Kong. J Affect Disord 2007;98:129-36. Crossref
- Lee S, Tsang A, Lau L, Mak A, Ng KL, Chan DM. Concordance between telephone survey classification and face-to-face structured clinical interview in the diagnosis of generalized anxiety disorder in Hong Kong. J Anxiety Disord 2008;22:1403-11. Crossref
- Lee S, Tsang A, Mak A, Lee A, Lau L, Ng KL. Concordance between telephone survey classification and face-to-face interview diagnosis of one-year major depressive episode in Hong Kong. J Affect Disord 2010;126:155-60. Crossref
- Lee S, Wu J, Ma YL, Tsang A, Guo WJ, Sung J. Irritable bowel syndrome is strongly associated with generalized anxiety disorder: a community study. Aliment Pharmacol Ther 2009;30:643-51. Crossref
- Mak AD, Wu JC, Chan Y, Chan FK, Sung JJ, Lee S. Dyspepsia is strongly associated with major depression and generalised anxiety disorder - a community study. Aliment Pharmacol Ther 2012;36:800-10. Crossref
- Hsieh FY, Bloch DA, Larsen MD. A simple method of sample size calculation for linear and logistic regression. Stat Med 1998;17:1623-34. Crossref
- Lee S, Tsang A, Chui H, Kwok K, Cheung E. A community epidemiological survey of generalized anxiety disorder in Hong Kong. Community Ment Health J 2007;43:305-19. Crossref
- Koloski NA, Jones M, Kalantar J, Weltman M, Zaguirre J, Talley NJ. The brain-gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut 2012;61:1284-90. Crossref
- Bradley LA, Richter JE, Pulliam TJ, Haile JM, Scarinci IC, Schan CA, et al. The relationship between stress and symptoms of gastroesophageal reflux: the influence of psychological factors. Am J Gastroenterol 1993;88:11-9.
- Johnston BT. Stress and heartburn. J Psychosom Res 2005;59:425-6. Crossref
- Kroenke K, Jackson JL, Chamberlin J. Depressive and anxiety disorders in patients presenting with physical complaints: clinical predictors and outcome. Am J Med 1997;103:339-47. Crossref
- Lawal A, Kern M, Sanjeevi A, Antonik S, Mepani R, Rittmann T, et al. Neurocognitive processing of esophageal central sensitization in the insula and cingulate gyrus. Am J Physiol Gastrointest Liver Physiol 2008;294:G787-94. Crossref
- Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to gastrointestinal symptoms in the general population? Scand J Gastroenterol 2002;37:294-8. Crossref
- Naliboff BD, Mayer M, Fass R, Fitzgerald LZ, Chang L, Bolus R, et al. The effect of life stress on symptoms of heartburn. Psychosom Med 2004;66:426-34. Crossref
- McQueen DV. Comparison of results of personal interview and telephone surveys of behavior related to risk of AIDS: advantages of telephone techniques. In: Fowler F, editor. Health Survey Research Methods: Conference Proceedings. Washington, DC: Government Printing Office; 1989: 247-52.
- Ho DY, Fu W, Ng SM. Guilt, shame and embarrassment: revelations of face and self. Cult Psychol 2004;10:64-84. Crossref