East Asian Arch Psychiatry 2020;30:32-3 | https://doi.org/10.12809/eaap1878
Letter to Editor
There are concerns about adequacy of care for older people with severe mental illness in terms of health and social care aspects.1 An increasing number of patients with severe mental illness are expected to survive into old age.2 They are likely to develop neurodegenerative disorders such as dementia in addition to psychiatric morbidities. Up to 60% of such patients have clinically relevant cognitive impairment.1
People with severe mental illnesses, including schizophrenia, are at higher risk for developing dementia. These individuals are more likely to have chronic conditions that are also risk factors for dementia.3 Moreover, subtle neuronal pathologies in schizophrenia reduce the normal cognitive reserve that protects against dementia and lowers the threshold for the appearance of clinical impairment.4
Major depression in older adults is also commonly linked to cognitive dysfunctions. Repeated episodes of depression are associated with hypercortisolaemia, which can result in hippocampal damage and cortical abnormalities that are found in elderly patients with cognitive deficits.5
To implement better clinical service, it is important to delineate the complex needs of these patients, especially in cognitive functioning. Early screening of ageing patients with severe mental illness for cognitive impairment enables early treatment and improves prognosis and quality of care.
The Dementia Community Support Scheme (DCSS) aims to develop clinical expertise and to provide training to patients with mild-to-moderate dementia at district elderly community centres in Hong Kong. The scheme was extended to all such centres in 2019. Ageing patients with severe mental illness are potential beneficiaries if their cognitive impairment is detected promptly.
We conducted a pilot study to assess the cognitive functions of older patients with different severe mental illnesses at the adult psychiatric specialist outpatient department of United Christian Hospital, Hong Kong.
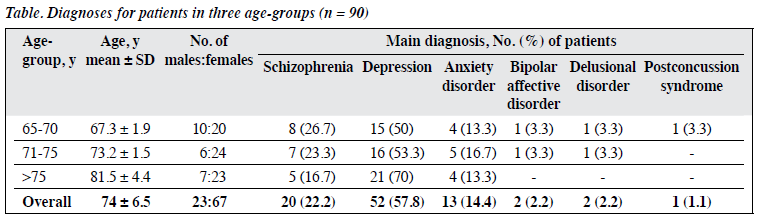
A total of 90 consecutive patients (23 men and 67 women) aged 65 to 95 years (mean, 74 ± 6.5 years) in three age-groups (65-70, 71-75, and ≥76 years) were included (Table). Patients were assessed for cognitive decline by nurses using the Global Deterioration Scale (GDS) before doctor consultation. The GDS measures cognitive decline on a scale of 0 (no decline) to 7 (very severe). The case doctor then screened out pseudo-dementia, and patients with mild-to-moderate dementia were referred to the DCSS. Further cognitive assessment was arranged by the case doctor and performed by nurses if indicated. Case notes of patients were screened for any documentation of symptoms of cognitive decline.
In the 65-70 years age-group, three patients had previously reported symptoms of cognitive decline, with GDS scores of 3 (n = 2) and 4 (n = 1). After the consultation, two patients were found to have a GDS score of 4. Both had a diagnosis of depression; one was referred to the DCSS and another refused.
In the 71-75 years age-group, four patients had previously reported symptoms of cognitive decline but had not been assessed. After the consultation, five patients were found to have a GDS score of 4. Four patients had depression and one had schizophrenia. Three of the five patients agreed to be referred to the DCSS. In addition, two patients with GDS score 2 or 3 were also referred to the DCSS.
In the ≥76 years age-group, one patient had previously reported symptoms of cognitive decline and had already been referred to the DCSS. After the consultation, seven patients were found to have a GDS score of ≥3: GDS score 4 (n = 3), GDS score 5 (n = 1), GDS score 6 (n = 2), and GDS score 7 (n = 1). Four patients had schizophrenia and three had depression. Patients with GDS score 6 or 7 were unsuitable for referral to the DCSS, as one was living in a residential home for the elderly and the other two could not walk unassisted. One patient (GDS score 4) refused referral to the DCSS. The remaining three patients were referred to the DCSS.
In this pilot study, the prevalence of dementia increased with age. Few patients with cognitive decline had previously reported such symptoms before assessment. Case doctors might not have enough time or awareness to assess cognitive function during routine examinations. Most patients were unable to notice or recognise symptoms of cognitive decline. When indicated, cognitive screening was performed by trained nurses using the Hong Kong version of the Montreal Cognitive Assessment.
Regarding screening for referral to the DCSS, targeting the 71-75 years age-group may achieve higher yield. These patients are relatively mobile and can travel to DCSS unassisted, and generally there are more patients with mild dementia in this age-group than in younger age- groups. In the ≥76 years age-group, patients may already have moderate-to-severe dementia and thus restricted in their ability to perform activities of daily living.
Early identification of dementia enables early treatment and support. This pilot study can raise awareness of the need to screen for cognitive decline in ageing patients with severe mental illnesses.
Declaration
The authors have no conflict of interest to disclose.
Mimi MC Wong, MBBS, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, United Christian Hospital, Hong Kong
Pui-fai Pang, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, United Christian Hospital, Hong Kong
Address for correspondence: Dr Mimi MC Wong, Department of Psychiatry, United Christian Hospital, 130 Hip Wo Street, Kwun Tong, Hong Kong.
Email: wmc009@ha.org.hk
Submitted: 10 September2018; Accepted: 19 January 2019
References
- McNulty SV, Duncan L, Semple M, Jackson GA, Pelosi AJ. Care needs of elderly people with schizophrenia. Assessment of an epidemiologically defined cohort in Scotland. Br J Psychiatry 2003;182:241-7.
- Jeste DV, Alexopoulos GS, Bartels SJ, Cummings JL, Gallo JJ, Gottlieb GL, et al. Consensus statement on the upcoming crisis in geriatric mental health: research agenda for the next 2 decades. Arch Gen Psychiatry. 1999;56:848-53.
- Ribe AR, Laursen TM, Charles M, Katon W, Fenger-Grøn M, Davydow D, et al. Long-term risk of dementia in persons with schizophrenia: a Danish population-based cohort study. JAMA Psychiatry 2015;72:1095-101.
- Dwork AJ, Susser ES, Keilp J, Waniek C, Liu D, Kaufman M, et al. Senile degeneration and cognitive impairment in chronic schizophrenia. Am J Psychiatry 1998;155:1536-43.
- Steffens DC, McQuoid DR, Payne ME, Potter GG. Change in hippocampal volume on magnetic resonance imaging and cognitive decline among older depressed and nondepressed subjects in the neurocognitive outcomes of depression in the elderly study. Am J Geriatr Psychiatry 2011;9:4-12.