East Asian Arch Psychiatry 2010;20:15-22
ORIGINAL ARTICLE
Dr KY Cheung, MBBS, MRCPsych, FHKCPsych, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, Hong Kong.
Dr Eva LW Dunn, MBBS, MRCPsych, FHKCPsych, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, Hong Kong.
Address for correspondence: Dr KY Cheung, Department of Psychiatry, Pamela Youde Nethersole Eastern Hospital, 3 Lok Man Road, Chai Wan, Hong Kong.
Tel: (852) 2595 6111; Fax: (852) 2595 9721; Email: cheuky02@msn.com
Submitted: 23 April 2009; Accepted: 25 June 2009
Abstract
Objectives: To study the characteristics of a cohort of first-episode manic patients treated in a regional psychiatric unit in Hong Kong, to explore the predictors of re-admission, and to investigate their functional outcomes 4 years after first hospitalisation.
Methods: This was a medium-term follow-up study, using retrospective review of hospital records and clinical interviews at follow-up. Forty-four Chinese patients diagnosed as having their first-episode mania were discharged from a gazetted psychiatric ward in Hong Kong between January 1999 and June 2002. Their clinical characteristics on admission and prescribed medications on discharge were investigated. Their re-admission status was charted. The patients were contacted for follow-up assessment of their functional outcome at 4 years after their first hospitalisation.
Results: In our cohort of 44 patients, their first-episode mania mostly presented in young adulthood, as significantly disturbed behaviour deemed to require compulsory admission. Nineteen (43%) of the patients were re-admitted at least once within 4 years of being discharged, 6 of whom were re-admitted more than once. Compulsory admission at the first-episode mania predicted future re-admission. Alcohol and substance abuse were associated with earlier re-admission after the first-episode mania. None of the patients died. For those who were reassessed (28 patients), most lived with family members. In all, 21 patients were able to sustain open employment at 4 years after discharge. About half (n = 14) of the traceable patients were able to continue in full-time employment at 4 years, while 7 were doing part-time work. The median Global Assessment of Functioning score of the traceable group was 88.
Conclusion: The results of this local study on patients with their first-episode of hospitalisation for mania were comparable to findings reported in western studies.
Key words: Bipolar disorder; Hospitalization; Treatment outcome
摘要
目的:研究於一所本港地区精神科治疗中心接受治疗的首发躁狂症患者群组的特徵和再度入院的预测因子,并检视他们在首次住院後4年的功能状态。
方法:这项中期随访研究是透过医院记录和随访期间临床面谈的方法进行,包括1999年1月至 2002年6月期间,从宪报认可精神科病房出院的44名华籍首发躁狂症患者。研究分析他们入院时的临床症状和出院时获处方的药物,并以表格形式记录他们再度入院的状态。在首次住院後 4年患者会获安排进行随访评估以检视他们的功能状态。
结果:44名首发躁狂症患者以年轻人为主,而行为紊乱的患者也须被强制入院。19名患者(43%)在出院4年内须再度入院,当中16名多於1次。因首发躁狂症被强制入院预示了再度入院的可能性,而酗酒和滥药更是加速再度入院的显著相关因素;研究中没有患者死亡。在28名接受随访跟进的患者中,大多与家庭成员居住;当中21名患者在出院4年後能公开就业,大约半数(14名)可持续全职工作,7名则维持兼职工作,而整体功能评估分数的中位数为88。
结论:这项有关因首发躁狂症住院的患者研究结果跟外国相若。
关键词:躁狂症、住院、治疗效果
Introduction
In contrast to schizophrenia, first-episode mania is a relatively neglected topic despite its important clinical significance to sufferers and their families.1 Outcome studies of first-episode mania in our locality are lacking.
Literature Review
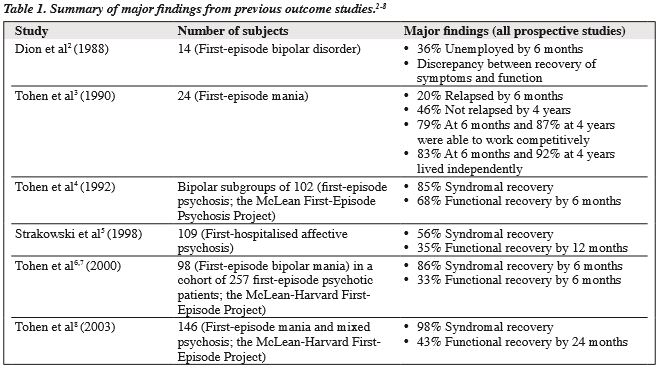
There were a number of outcome studies of first-episode mania, as shown in Table 1,2-8 but their findings were inconsistent. Discrepancies between studies might have been due to differences in sampling and methodology. Some studies suggest that the first-episode mania did not lead to complete recovery as Kraepelin9 had anticipated, and that a substantial proportion of the patients experienced unfavourable psychosocial and clinical outcomes.
Attempts to investigate socio-demographic and clinical factors to predict the outcome in first-episode mania have been presented in numerous studies. Clinical factors that were explored included: (1) socio-economic status3,5,6; (2) age of onset6,10,11; (3) presence of psychotic features12-15; (4) adherence to treatment5; (5) psychiatric co-morbidity3,6,16-19; and (6) medication.20,21
Methods
This study was conducted at the Pamela Youde Nethersole Eastern Hospital (PYNEH) in Hong Kong. From the Clinical Management System (CMS), a list of all patients discharged from the psychiatric ward of PYNEH from 1 January 1999 to 31 June 2002 with a diagnostic label of manic episode, hypomanic episode or bipolar affective disorder was drawn up. Admissions for hypomanic episode and bipolar affective disorder were traced because of the possibility of first-episode mania being given such a diagnosis. For the sake of completeness, the admissions for schizoaffective disorder were also traced for inspection because of the high level of symptom overlap. Eligible cases were identified by examination of case files of the listed patients. Cases were selected according to the following inclusion / exclusion criteria. The inclusion criteria were: (1) first psychiatric hospitalisation; (2) age 15 to 65 years (at the index admission); (3) Chinese ethnicity; (4) first onset of mental illness (symptoms presenting < 1 month before the index admission); and (5) satisfactory diagnosis of a manic episode, with or without psychotic features, according to the diagnostic criteria of the 10th revision of the International Classification of Diseases (ICD- 10). Cases were excluded if there was evidence of: (1) organic mental illness; (2) drug intoxication; (3) mental retardation (intelligence quotient score of less than 70), in whom outcomes are inherently different; (4) a previous depressive episode / illness; or (5) prior use of antipsychotics or mood stabilisers. Diagnosis depended on blinded examination of the case files by another qualified psychiatrist and agreement between the 2 was 100%.
Data on the first (index) psychiatric admission were collected for each subject from the hospital case files and CMS. Information about the ongoing condition of each subject, during the observation period of 4 years after discharge from the index admission, was obtained from the outpatient psychiatric records of the corresponding psychiatric centres, the CMS, and interview of the subjects. Each subject was traced by telephone and then invited to a face-to-face interview. For patients who declined face-to- face interviews, information was gathered by telephone. Written consent was obtained during face-to-face interviews and verbal consent during phone interviews. Data were recorded on a checklist specifically designed for the study. Socio-demographic characteristics (on the index admission) including age, gender, marital status, living environment, education level, and employment status were charted. The onset characteristics of the index admission were also recorded. Various outcome variables were studied, including: re-admission status, mortality, and the follow- up assessments (living condition, employment status, follow-up services used), and the Global Assessment of Functioning (GAF) score. This project was approved by the Ethics Committee of the Hong Kong Hospital Authority.
Statistical Analysis
The data were processed and analysed using the Statistical Package for the Social Sciences Windows version 11.5 (SPSS Inc., Chicago [IL], US). The significance level was set at 5% and 95% confidence intervals were calculated. Descriptive statistics were used for patient characteristics and clinical features. For continuous variables approximating to a normal distribution, mean and standard deviation (SD) values were derived. Parametric methods such as t tests were adopted for analysis. Median and range values were utilised for non-normal continuous and non-parametric data. The Mann-Whitney U test was used to compare 2 groups with continuous non-normal distributions. Categorical variables were described by frequency distribution with proportions and percentages. Cross-tabulation was performed for individual categorical variables and the significance of differences tested by Chi-square tests; Fisher’s exact test was used if assumptions for the Chi-square test were violated. Survival analysis was performed to analyse the data dealing with the time to first re-admission. Univariate Cox regression analysis was performed to investigate the association between the clinical variables and the time to re-admission.
Results
Patient Characteristics on Index Admission
Forty-four patients (20 females and 24 males) with a first psychiatric admission for first-episode mania were identified. The age of onset of these subjects ranged from 15 to 62 years, with a median age of 28 (mean [SD], 32 [13]) years. Sixteen patients (36%) were aged 20 to 29 years, the age-group with the largest proportion. The median age of onset in females was 30 years and that for males was 25 years. In all, 28 (64%) were single, 12 (27%) were married, and 4 (9%) were divorced or separated. Most of the patients (91%) lived with family members. Seven subjects (16%) had received education up to a tertiary level, 24 (55%) up to an upper secondary level, 8 (18%) to a lower secondary level, whereas 5 (11%) had received only primary level or no education. In the year prior to the index admission, 27 (61%) of the patients were engaged in gainful employment, 6 (14%) were homewives / househusbands or students, 4 (9%) had part-time gainful employment, and 7 (16%) were unemployed. Six patients (14%) had a history of substance misuse; 2 with cannabis, 1 abused ecstasy, 1 both ecstasy and methylamphetamine, 1 heroin, and 1 took a weight- reducing agent. Only 2 patients (5%) had a history of alcohol abuse. Thirteen patients (30%) had a positive family history of mental illness.
Clinical Features of Index Admission
Thirty patients (68%) were admitted to the psychiatric ward on a compulsory basis, and 14 (32%) were admitted voluntarily. Nine patients (20%) did not present with any psychotic symptoms, while 35 (80%) displayed psychotic symptoms. Thirty-four patients (77%) presented with disturbing behaviour in public; 6 (14%) displayed promiscuous behaviour at presentation, while 17 (39%) displayed overspending. Five patients (11%) presented with suicide attempts or gestures; 3 of whom gestured jumping from a height and 2 had expressed suicide ideation. Thirteen patients (30%) showed aggressive behaviour before admission. The varieties of aggressive behaviour included: fisting, slapping, or beating up; smashing a windowpane, hitting furniture; threatening others with a knife; and chasing father with a knife. The potential victims were mostly family members.
Treatment Characteristics
The duration of stay (DOS) during the index admission ranged from 0 day (1 patient was discharged on the day of admission) to 305 days; the mean (SD) was 57 (53) days and the median was 49 days. The frequency distribution of DOS was not normal. Only 4 patients (9%) were discharged against medical advice. Concerning the use of medications on discharge after the index admission, 38 patients (86%) were prescribed antipsychotics, while 17 (39%) received a mood stabiliser. Among these patients 25 (57%) were given an antipsychotic alone, 13 (30%) a combination of a mood stabiliser and an antipsychotic, and 4 (9%) took a mood stabiliser. Haloperidol was the most commonly prescribed antipsychotic (45%, n = 20). Lithium was the most commonly prescribed mood stabiliser (25%, n = 11), while valproic acid was prescribed in 7 patients (16%). On discharge, 2 patients (5%) were treated with 2 mood stabilisers in combination (lithium and valproic acid; lithium and carbamazepine), and 1 was prescribed an antidepressant (fluvoxamine). No patient received electroconvulsive therapy during the index admission.
Tracing of Subjects for Follow-up Assessment
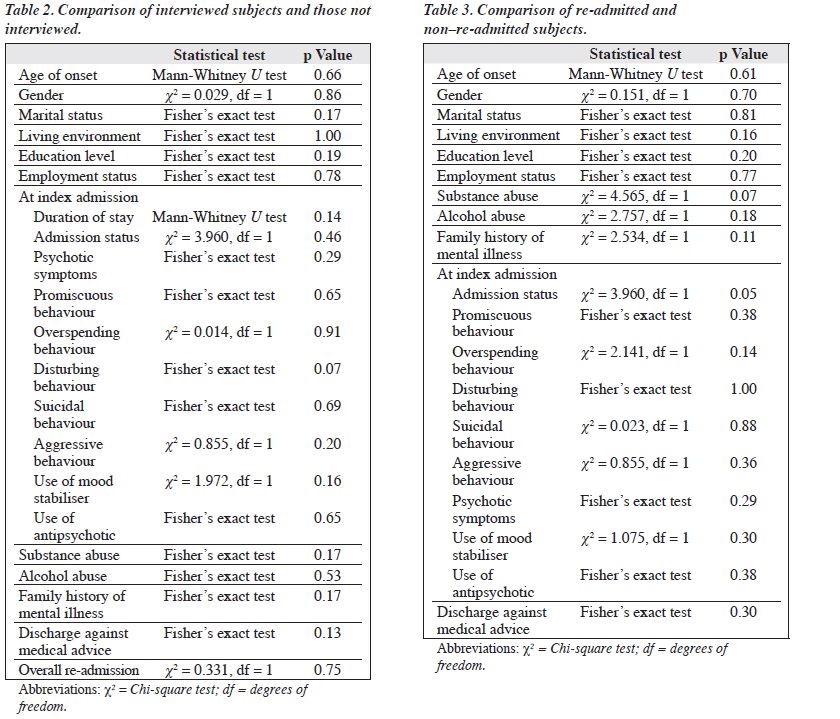
Among the 44 subjects identified, 14 (32%) could not be traced for interview. Among the 30 who could be traced, 2 refused to be interviewed. Thus, 28 patients were involved in the follow-up assessment of outcome after first-episode mania: 3 had a face-to-face interview, and 25 via phone by the same interviewer. A comparison of the demographics and other characteristics of the interviewed and not-interviewed subjects was carried out and yielded no statistically significant differences (Table 2).
Outcome Assessments
Re-admission
The records of all 44 identified subjects were reviewed over a 4-year observation period after discharge from their index admission. During that period, 25 (57%) were not re-admitted, whereas 19 (43%) had at least 1 re-admission, 6 of whom were re-admitted more than once (5 and 1 re- admitted twice and 4 times respectively).
Factors Predicting Re-admission
Only the admission status (ie compulsory admission at the index hospitalisation) was found to be a statistically significant predictor of subsequent re-admission over 4 years. A higher proportion having compulsory index admissions were subsequently re-admitted than those who were admitted voluntarily (53% vs. only 21%). Substance abuse was not found to be a significant variable in predicting re-admission (p = 0.07) [Table 3].
Time to First Re-admission
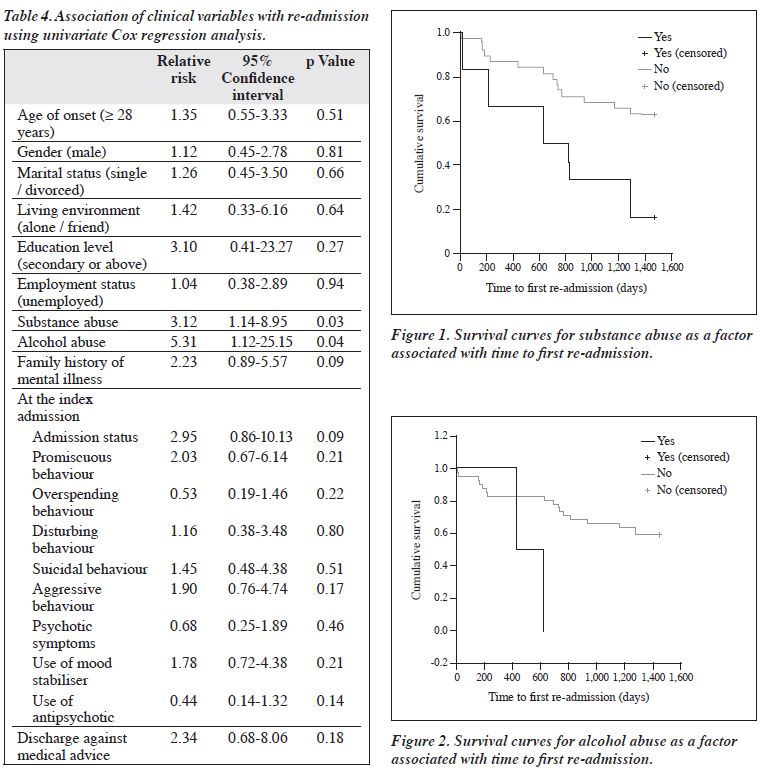
The time to re-admission ranged from 5 to 1,280 days, with a median value of 626 (mean [SD], 583 [94]) days. To allow for a clear analysis in the Cox regression, some of the categorical variables (age of illness onset, marital status, living environment, education level, and employment status) were dichotomised. The results of the univariate Cox regression analysis are shown in Table 4. Only 2 variables (history of substance abuse and alcohol abuse) were significant. The history of substance abuse was associated with a 3-fold increased risk of early re-admission. Patients with a history of alcohol abuse had a higher risk of re-admission (5 fold) than those without such a history. The p values of family history of mental illness and admission status at the index admission were not quite significant.
Survival curves for the 2 significant variables (substance abuse and alcohol abuse) are shown in Figures 1 and 2. Both showed that such abuse was associated with increased risk of early re-admission when compared with non-abusers.
Total Duration of Hospitalisation
For the 19 subjects with subsequent re-admissions, the total duration of hospitalisation over the observation period ranged from 2 to 208 days, with a mean (SD) of 79 (67) days and a median of 62 days. The frequency distribution of such periods of hospitalisation was not normal. The proportion of time spent in hospital over the 4-year observation period ranged from 0.14% to 14%, with a median value of 4% (mean, 5%).
Death
To our knowledge, no subjects were dead at the time of follow-up assessment.
Follow-up Assessments
Living Condition
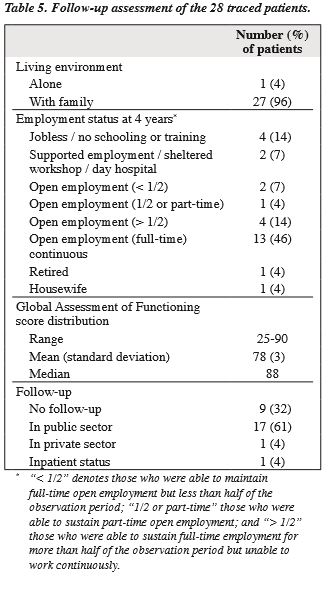
Of the 28 patients interviewed, 27 (96%) were living with family members at the time of assessment and 1 was lived alone; none were institutionalised or homeless (Table 5).
Employment Status at Four Years
Only a minority of the reassessed patients (4/28) did not engage in any work-related activity (job, training, schooling, housework), 1 of whom was physically disabled after a traffic accident. Thirteen patients (46%) were rated as continuously employed over the year preceding the assessment. Two patients were receiving training in a day hospital (1 of whom had his diagnosis revised to schizophrenia). One patient was retired and 1 carried out housework. Most of the subjects were engaged in a certain level of gainful employment (any level of full-time or part- time employment, including being a housewife), ie 21/28 patients (75%). Seven (25%) were unable to undertake gainful employment, 14 (50%) had full-time continuous jobs (housewife being regarded as full-time employment), and 7 (25%) had jobs not involving continuous full-time work (Table 5).
Global Assessment of Functioning
For the 28 subjects who were successfully interviewed, the GAF score in the last 1 year ranged from 25 to 90; the frequency distribution of these scores was not normal, the median being 88.
Outpatient Clinic Follow-up
At the time of assessment, 17 patients (61%) were receiving outpatient public-sector psychiatric care (in psychiatric centres of the Hospital Authority), 1 (4%) was an inpatient, and 1 (4%) was continuing treatment in the private sector; 9 others (32%) were not receiving any form of psychiatric treatment. Thus, 19 patients were receiving some form of psychiatric treatment and 9 were not. There was no statistically significant association between re-admission and follow-up status at 4 years (Fisher’s exact test).
Discussion
The median age of illness onset in our cohort was 28 years. The reported median age of onset of mania in previous studies was variable but generally accepted to be in the early adulthood.22 In our cohort, those with a history of alcohol abuse was 38 years as opposed to 27 years in those without. Though this difference was not significant, it seemed to support the postulation that alcohol might have an inducing effect on bipolar disorder, as suggested by Strakowski et al16 based on a cohort of 59 first-episode manic patients. This hypothesis was also supported by other studies, including that by DelBello et al23 who observed that those with a history of alcohol abuse had a lower rate of familial affective illness than those without. In our cohort, antipsychotic use was common; 86% of the patients were prescribed antipsychotic medications. This proportion is higher than that in some western studies; Zarate and Tohen24 reported a rate of 77% of a group of 129 first-episode manic patients. Only 17 patients (39%) in our cohort received a mood stabiliser on discharge, while Tohen et al3 reported a rate of 87%. The reason for concerns about the choice of psychotropic treatment (especially typical antipsychotics) were manifold, and include bipolar disorder known to be susceptible to tardive dyskinesia,25 and the observation that typical antipsychotics may induce depression.26 However, the significance of early mood stabiliser use as a means of achieving better long-term outcomes in patients with first- episode mania remains unclear.
Association between Patient Characteristics and Clinical Outcomes
In our cohort, compulsory admission status was associated with subsequent hospitalisation. One possible explanation could be that such patients were having more severe symptoms and this might predict future episodes. Alternatively, compulsorily admitted patients had poorer insight or poor social support to adhere to treatment, resulting in subsequent re-admission.
History of alcohol and substance abuse yielded statistically significant associations with earlier first re- admission. This adds to the evidence demonstrating the negative influence of co-morbidity on the outcome of mania. Others have reported that first-episode manic patients with a diagnosis of alcohol abuse had a poorer initial outcome,17 lower and more delayed rates of recovery,5 and shorter remissions.13
Functional Outcome at Four Years after First- episode Mania
Most of the traceable subjects lived with a family, which was consistent with having a certain level of social support. However, it might also reflect inability to live independently. About three-quarters of the traceable patients maintained a certain level of gainful employment. Among the 4 patients who were not employed, 1 was physically disabled and 1 was retired. However, of those in gainful employment, one- third did not have continuous full-time employment but only part-time or intermittent jobs. Given the fact that about 70% of our cohort were educated up to upper secondary level or higher, and that nearly 80% were employed prior to their illness, this is an important observation. The median GAF score of the traceable subjects 4 years after discharge was 88, which is not low, implies that they had relatively good global functioning.
Comparison of Local Findings with Those of the Western Countries
In the present study, 80% of the cohort presented with psychotic features, which is similar to rates of 63% to 88% reported from elsewhere.3,27,28 Only 5% of our cohort had a history of alcohol abuse and 14% of substance abuse, the figures of which were smaller than those reported by others; alcohol abuse being diagnosed in 24% to 39% of patients, and drug abuse in 16% to 35%.16,17,29,30 In our cohort, alcohol and substance abuse also yielded statistically significant associations with earlier first re-admission. This is in agreement with previous experience3,6,16-19 demonstrating the negative influence of psychiatric co-morbidity on the outcome of mania. In our cohort, about half of the patients had at least 1 re-admission within 4 years of being discharged, which was very comparable to the approximately 50% relapse rate over 4 years findings reported by Tohen et al.3,13
Concerning functional outcomes, Tohen et al13 identified 87% of a cohort of first-episode manic patients with relatively good functioning at 4 years who were able to work competitively. The present study findings were comparable, in that about three-quarters of the subjects were able to work in the community at a certain level. By contrast others reported less favourable outcomes,5,6 where only about one-third of patients had functional recovery. However, such findings need cautious interpretation because they entailed shorter follow-up periods (6 and 12 months).5,6 After all, patients suffering from first-onset mania are overwhelmed with difficulty in the initial adaptation period that may be compounded by loss of relationships or jobs during the early phase. Certainly, more focus on the early phase of the bipolar illness is recommended.
Methodological Considerations
A limitation of our study design was the sample size, and so it may not have had the power to detect significant associating factors. Its retrospective nature meant that it lacked quality assurance and completeness of data. Clinical diagnoses were not standardised. The samples were biased towards more severe disease, and so the results may not be generalised. The strength of the study was that it was the first local series with a focus on first- episode mania looking at medium-term outcomes. Though small, our cohort was collected over a period of 3.5 years in a major regional psychiatric unit that serves a large population in Hong Kong, which proved to be a challenge owing to the low incidence of first-episode mania (1.7 to 4.5 per 100,000 per year) in our locality. It did succeed in generating preliminary data for further research.
Clinical Implications
Our study showed that if the index admission was compulsory, it predicted the occurrence of subsequent re-admission. Compulsory admission in psychiatric care usually involves patients with poor insight. More effort is needed to manage this patient group, with special emphasis on psycho-education and targeted at insight training to enhance adherence to treatment with a view to improve outcomes. Although the majority of traceable patients were able to attain a certain level of gainful employment, one-third did not have continuous full-time employment 4 years after discharge from their first hospitalisation, which indicates some degree of vocational impairment. Special vocational training therefore appears necessary for these patients, and requires further exploration.
Acknowledgements
I would like to thank Dr Eva Lai-wah Dunn, Dr Patty Heung-wah Yim (SMO, Department of Psychiatry, PYNEH), Dr Orlando Wai-nang Tang (Consultant, Department of Psychiatry, PYNEH), Dr Wah-fat Chan (Consultant, Department of Psychiatry, PYNEH), and Dr Charles Wai- hong Chan. Special thanks to Christo of the Medical Record Office of PYNEH. I would also like to thank Dr TL Lo (COS, Division I, Kwai Chung Hospital); Dr PK Kwong (COS, Division II, Kwai Chung Hospital), Dr Ka-chee Yip (COS, Department of Psychiatry, Kowloon Hospital), Dr GC Yiu (COS, Department of Psychiatry, United Christian Hospital), Dr MC Wong (SMO, Department of Psychiatry, Queen Mary Hospital) for giving permission and assistance in data collection in their respective psychiatric centre. Heartfelt thank goes to Dr Ka-lik Kwan and Dr Quinson Lee. I would like to acknowledge Prof H Chiu for permission of use of the Global Assessment of Functioning (Chinese version).
References
- Conus P, McGorry PD. First-episode mania: a neglected priority for early intervention. Aust N Z J Psychiatry 2002;36:158-72.
- Dion GL, Tohen M, Anthony WA, Waternaux CS. Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hosp Community Psychiatry 1988;39:652-7.
- Tohen M, Waternaux CM, Tsuang MT, Hunt AT. Four-year follow-up of twenty-four first-episode manic patients. J Affect Disord 1990;19:79- 86.
- Tohen M, Stoll AL, Strakowski SM, Faedda GL, Mayer PV, Goodwin DC, et al. The McLean First-Episode Psychosis Project: six-month recovery and recurrence outcome. Schizophr Bull 1992;18:273-82.
- Strakowski SM, Keck PE Jr, McElroy SL, West SA, Sax KW, Hawkins JM, et al. Twelve-month outcome after a first hospitalization for affective psychosis. Arch Gen Psychiatry 1998;55:49-55.
- Tohen M, Hennen J, Zarate CM Jr, Baldessarini RJ, Strakowski SM, Stoll AL, et al. Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry 2000;157:220-8.
- Tohen M, Strakowski SM, Zarate C Jr, Hennen J, Stoll AL, Suppes T, et al. The McLean-Harvard first-episode project: 6-month symptomatic and functional outcome in affective and nonaffective psychosis. Biol Psychiatry 2000;48:467-76.
- Tohen M, Zarate CA Jr, Hennen J, Khalsa HM, Strakowski SM, Gebre-Medhin P, et al. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry 2003;160:2099-107.
- Kraepelin E. Dementia praecox and paraphrenia, together with, manic depressive insanity and paranoia. The Classics of Medicine Library; 1989.
- Carlson GA, Bromet EJ, Sievers S. Phenomenology and outcome of subjects with early- and adult-onset psychotic mania. Am J Psychiatry 2000;157:213-9.
- Tsai SM, Chen C, Kuo C, Lee J, Lee H, Strakowski SM. 15-year outcome of treated bipolar disorder. J Affect Disord 2001;63:215-20.
- Rosen LN, Rosenthal NE, Dunner DL, Fieve RR. Social outcome compared in psychotic and nonpsychotic bipolar I patients. J Nerv Ment Dis 1983;171:272-5.
- Tohen M, Waternaux CM, Tsuang MT. Outcome in mania. A 4-year prospective follow-up of 75 patients utilizing survival analysis. Arch Gen Psychiatry 1990;47:1106-11.
- Albus M, Hubmann W, Wahlheim C, Sobizack N, Franz U, Mohr F. Contrasts in neuropsychological test profile between patients with first-episode schizophrenia and first-episode affective disorders. Acta Psychiatr Scand 1996;94:87-93.
- Fennig S, Bromet EJ, Karant MT, Ram R, Jandorf L. Mood-congruent versus mood-incongruent psychotic symptoms in first-admission patients with affective disorder. J Affect Disord 1996;37:23-9.
- Strakowski SM, Tohen M, Stoll AL, Faedda GL, Goodwin DC. Comorbidity in mania at first hospitalization. Am J Psychiatry 1992;149:554-6.
- Strakowski SM, Tohen M, Stoll AL, Faedda GL, Mayer PV, Kolbrener ML, et al. Comorbidity in psychosis at first hospitalization. Am J Psychiatry 1993;150:752-7.
- Strakowski SM, McElroy SL, Keck PE Jr, West SA. The effects of antecedent substance abuse on the development of first-episode psychotic mania. J Psychiatr Res 1996;30:59-68.
- Tohen M, Tsuang MT, Goodwin DC. Prediction of outcome in mania by mood-congruent or mood-incongruent psychotic features. Am J Psychiatry 1992;149:1580-4.
- Licht RW, Gouliaev G, Vestergaard P, Dybbro J, Lund H, Merinder L. Treatment of manic episodes in Scandinavia: the use of neuroleptic drugs in a clinical routine setting. J Affect Disord 1994;32:179-85.
- Sernyak MJ, Griffin RA, Johnson RM, Pearsall HR, Wexler BE, Woods SW. Neuroleptic exposure following inpatient treatment of acute mania with lithium and neuroleptic. Am J Psychiatry 1994;151:133-5.
- Goodwin FK, Jamison KR. Manic depressive illness. New York: Oxford University Press; 1990.
- DelBello MP, Strakowski SM, Sax KW, McElroy SL, Keck PE Jr, West SA, et al. Familial rates of affective and substance use disorders in patients with first-episode mania. J Affect Disord 1999;56:55-60.
- Zarate CA Jr, Tohen M. Antipsychotic drug treatment in first-episode mania: a 6-month longitudinal study. J Clin Psychiatry 2000;61:33- 8.
- Keck PE Jr, McElroy SL, Strakowski SM, Soutullo CA. Antipsychotics in the treatment of mood disorders and risk of tardive dyskinesia. J Clin Psychiatry 2000;61 Suppl 4:S33-8.
- Tohen M, Zarate CA Jr. Antipsychotic agents and bipolar disorder. J Clin Psychiatry 1998;59 Suppl 1:S38-48.
- Strakowski SM, Williams JR, Fleck DE, Delbello MP. Eight- month functional outcome from mania following a first psychiatric hospitalization. J Psychiatr Res 2000;34:193-200.
- McElroy SL, Strakowski SM, West SA, Keck PE Jr, McConville BJ. Phenomenology of adolescent and adult mania in hospitalized patients with bipolar disorder. Am J Psychiatry 1997;154:44-9.
- Keck PE Jr, McElroy SL, Strakowski SM, West SA, Hawkins JM, Huber TJ, et al. Outcome and comorbidity in first- compared with multiple-episode mania. J Nerv Ment Dis 1995;183:320-4.
- Strakowski SM, Keck PE Jr, McElroy SL, Lonczak HS, West SA. Chronology of comorbid and principal syndromes in first-episode psychosis. Compr Psychiatry 1995;36:106-12.