East Asian Arch Psychiatry 2012;22:12-7
ORIGINAL ARTICLE
Cognitive Function, Functional Performance and Severity of Depression in Chinese Older Persons with Late-onset Depression
华裔老年晚发性抑鬱症患者的认知功能、功能特性和抑鬱症严 重程度研究
谭焕芝、林翠华
Dr Cindy Woon-Chi Tam, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, North District Hospital, Hong Kong SAR, China.
Prof Linda Chiu-Wa Lam, FHKCPsych, FHKAM (Psychiatry), Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong SAR, China.
Address for correspondence: Dr Cindy Woon-Chi Tam, Department of Psychiatry, Psychiatric Outpatient Department, North District Hospital, 9 Po Kin Road, Sheung Shui, New Territories, Hong Kong SAR, China.
Tel: (852) 2683 7620; Fax: (852) 2683 7616; Email: tamwoonchi@hotmail.com
Submitted: 19 September 2011; Accepted: 11 November 2011
Abstract
Objectives: The relationship between cognitive status and depressive symptoms and their liability to cause functional decline are of clinical and public health importance as it appears to be common, frequently coexists, and may be treatable. This study examined the relationship of depression severity and cognitive performance and the impact of such an interaction on functional ability in Chinese elderly subjects with late-onset depression.
Methods: A total of 105 non-demented elderly patients with late-onset depression were recruited. Impairment in instrumental activities of daily living and severity of depression were respectively assessed with the Disability Assessment for Dementia scale and the 24-item Hamilton Depression Rating Scale. Various cognitive domains were assessed including global cognitive function, delayed episodic memory, and executive functions. The relationship between specific cognitive impairment and mood symptom severity was assessed. The clinical correlates of functional performance were also examined.
Results: Increasingly severe depression was associated with lower scores in the Mini-Mental State Examination, delayed recall, and poorer performance in the Trail Making Test–Part A (after adjusting for the effect of age and education). The severity of apathy correlated negatively with the Mini-Mental State Examination scores only. Among the depressed subjects, greater levels of depression and apathy, poorer performance in Trail Making Test–Part B, and mild parkinsonian signs were associated with lower functional scores.
Conclusions: Lack of interest and motivation, depressive mood, compounded by behavioural abnormalities resulting from executive dysfunction, accounted for functional disability in elderly subjects with late-onset depression. These relationships may provide the background for developing interventions targeting functional deficits associated with specific cognitive dysfunctions and depression.
Key words: Age of onset; Cognition disorders; Depression
摘要
目的:功能衰退和抑鬱症是普遍且经常并存,却可以医治的疾病。因此,认知状态和抑鬱症症状之间的关係,以及他们对功能衰退的影响具重要的临床和公共卫生价值。本文检视抑鬱症严重程度与功能表现的关係,以及这种关係对华裔老年晚发性抑鬱症患者其功能性能力的影响。
方法:以105例认知正常的老年晚发性抑鬱症患者为研究对象,并分别以脑退化症失能量表和汉密尔顿抑鬱量表,评估他们的工具性日常生活活动能力障碍和抑鬱症严重程度,并观察整体认知功能、延宕事件记忆和执行功能等各种认知域。研究也对特定认知缺损和情绪症状严重程度进行评估,以及检视功能表现的临床相互关係。
结果:严重抑鬱症与简易精神状态量表、延宕记忆测试,以及经调整年龄和教育程度後的连线测试A表现较差相关;而冷漠感严重程度则与简易精神状态量表得分呈负相关。在这组患者当中,较严重的抑鬱症和冷漠感、连线测试B表现较差的,以及出现轻度帕金逊症症状的患者均与功能得分较低相关。
结论:缺乏兴趣和动力、抑鬱情绪,加上因执行功能障碍导致的行为异常可导致老年晚发性抑鬱症患者的功能性失能。它们之间的关係或有助针对与特定认知缺损和抑鬱症相关的功能缺损的治疗方案发展。
关键词:发病年龄、认知障碍、抑鬱症
Introduction
Depression in late life is associated with significant morbidity, including deficits in a range of cognitive functions and considerable functional impairment and disability. The relationship between cognitive status and depressive symptoms and their effects on functional decline are of significant clinical and public health importance, because both are common, frequently coexist, and may be treatable.
Neurocognitive deficit involving executive dysfunction is common when first onset of depression occurs in late life. A number of clinical factors might be linked to neuropsychological decline in late-onset depression.1-3 Even after controlling for the effects of demographic variables, there is still an effect of depressive severity on cognitive function.
The relationship between disability and depression is even more complex and probably bidirectional. In a systematic review of variables predicting functional decline in community-dwelling older adults, depression was one of the key risk factors identified.4 Beekman et al5 reported that both major and minor depression were associated with disability. Lyness et al6 reported that functional outcomes associated with subsyndromal or minor depression were not as poor as for those among patients with major depression, but poorer than observed for those who were non-depressed.
Previous studies of clinically non-demented community-dwelling Chinese elderly in Hong Kong found that executive dysfunction, depressive symptoms, apathy, and mild parkinsonian signs (MPS) were associated with functional disability.7-9 However, information about the functional correlates in Chinese elderly with late-onset depression was limited. Chan et al10,11 found that depressed Chinese elderly had poorer self-perceived quality of life and that quality of life correlated with the level of depression and functional limitations. It would be important to investigate how the severity of mood symptoms and physical health affects cognitive and functional performance in this group with significant mood disturbances.
In the current cross-sectional study, we aimed to investigate the relationship between cognitive performance and severity of depression in Chinese elderly subjects with late-onset depression. The second aim was to examine the impact of cognitive function and mood symptoms on functional performance in depressed Chinese elderly. Investigating the relationship between these factors might provide insight into the underlying pathology of late-onset depression and help identify those at high risk and greater disability for further investigation.
Methods
Sample
Patients aged ≥ 60 years who fulfilled DSM-IV criteria12 for major or minor depression were recruited from psychiatric outpatient clinics and the inpatient psychiatric unit in the New Territories East Cluster hospitals in Hong Kong from year 2007 to 2009. The onset of the first depressive episode had to be at the age of 50 years or older.
Each depressed subject was evaluated by a qualified psychiatrist to establish eligibility for inclusion in the study, a clinical diagnosis, and a clinical staging assessment using the Clinical Dementia Rating (CDR) scale.13 Subjects with a global CDR score of 0 or 0.5 were recruited.
Subjects with a history of degenerative neurological disorder, dementia, cortical strokes, severe or unstable physical illness (i.e. those who had been hospitalised in the last 3 months), and a history or current substance / alcohol abuse were excluded. Subjects who had had electroconvulsive therapy in the past 3 months were also excluded. The psychiatrists explained the procedure and obtained written consent from the participants or their caregivers. This study was approved by the Joint CUHK-NTEC Clinical Research Ethics Committee. An experienced research assistant performed the cognitive and functional assessment.
Assessments
All depressed patients underwent a comprehensive psychiatric, cognitive and functional assessment. Depression was diagnosed according to DSM-IV criteria and symptom severity was rated using the 24-item Hamilton Depression Rating Scale (HDRS).14
Cognitive Tests
Global cognitive assessment was estimated using the Cantonese version of the Mini-Mental State Examination (CMMSE)15 and the Chinese version of the Alzheimer’s Disease Assessment Scale–Cognitive subscale (ADAS- Cog).16 To test for episodic memory, subjects were also examined using a 10-minute delayed recall of a word list from the ADAS-Cog. Digit span and visual span tests were carried out to test attention and working memory. The Category Verbal Fluency Test (CVFT)17 and Trail Making Test (TMT) were performed as executive function tests.18 In the CVFT, subjects were asked to generate exemplars in the categories of animals, fruit, and vegetables within 1 minute. Combined scores were then computed. Trail Making Test– Part A (TMT-A) was used to assess processing speed. Trail Making Test–Part B (TMT-B) additionally measured mental set shifting and response inhibition. We modified TMT by changing the sequence of alphabets to Chinese writing of
numbers with ascending order, as most subjects had not received an English language education.
Disability Assessment for Dementia Scale
The Disability Assessment for Dementia scale (DAD) is a validated measure of activities of daily living (ADL) designed specifically for use in patients with dementia. The Chinese version of DAD has been validated in Chinese subjects.19 It evaluates instrumental ADL (meal preparation, telephoning, going on an outing, finance, medication, leisure, and housework) and basic ADL (hygiene, dressing, undressing, continence, and eating) through the caregiver observations of the subject’s actual performance in the previous 2 weeks.
Neuropsychiatric Symptoms
Neuropsychiatric symptoms were identified using the Chinese version of Neuropsychiatric Inventory (NPI)
Motor Signs
Motor symptoms including axial dysfunction, bradykinesia, rigidity and tremor were assessed by the Unified Parkinson’s Disease Rating Scale–motor subscale.22 The MPS score was calculated by summing up the scores in this scale.
Medical illness burden was assessed by the Cumulative Illness Rating Scale (CIRS).23 The CIRS is a measure of physical illness in which a cumulative score is derived from ratings of severity of impairment in each of 13 organ systems. In addition, presence of cardiovascular risk factors and vascular diseases including hypertension, diabetes mellitus, hyperlipidaemia, heart disease, arrhythmia, and cerebrovascular accidents were recorded. A combined cardiovascular risk score was calculated by summing up the total number of these risk factors.
Statistical Analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS 17.0; SPSS Inc., Chicago [IL], US). Spearman correlation analyses were performed to assess the association between functional disability and mood scores. Factors that correlated with the DAD scores at p < 0.05 were entered as explanatory variables. Multiple linear regression analyses were performed to examine the predictors for DAD scores.
Results
A total of 105 subjects were recruited. The demographic characteristics of the subjects are summarised in Table 1. The mean depressive score reflected that they suffered from mild-to-moderate depression.
Factors Affecting Cognitive Performance in Depressed Subjects
Relationship between Clinical Characteristics and Cognitive Test Scores
Neither medical nor cardiovascular risk burden correlated significantly with cognitive test scores. Nor did age of onset of depression or duration of the current episode correlate with cognitive test scores.
Relationship between Mood Symptoms and Cognitive Test Scores
The HDRS and NPI-depression scores correlated with cognitive scores involving multiple domains, while NPI- apathy scores mainly correlated with executive test scores (Table 2).
Table 3 shows the correlations between cognitive test scores and mood symptom severity after controlling for age and education, in which case the severity of depression nevertheless correlated significantly with CMMSE scores, the forward visual span test scores, TMT-A scores, and negatively with CMMSE score after controlling for age and education. The extent of correlation between mood symptoms and cognitive test scores decreased after adjusting for age and education, except that between the severity of depression and TMT-A scores.
Factors Affecting Functional Performance in Depressed Subjects
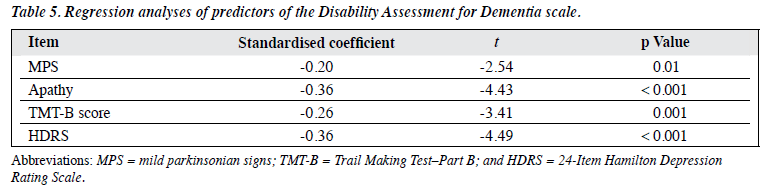
Table 4 shows the relationship between clinical and cognitive correlates and functional scores. The predictors for DAD scores are shown in Table 5. Apathy, performance in the executive test (TMT-B), depression severity, and MPS were independent predictors of functional performance among depressed subjects.
Discussion
According to our results, the severity of depression correlated with impairment in working memory, episodic memory, and slowing of processing speed among the elderly with late-onset depression. Apathy did not correlate with performance in the executive function test after controlling for age and education. Baudic et al24 also found that deficits in executive function and memory correlated with the depression severity in the elderly. They suggested that memory failure in these patients might reflect impairment in retrieval processes, which in turn depends on executive function. Sheline et al3 suggested that changes in processing speed fully mediated the influence of depression severity on all other cognitive domains (executive function, language and working memory). It was also proposed that frontostriatal limbic abnormalities predispose to both depressive symptoms and executive dysfunction in older adults.25
Sheline et al3 found significant associations between vascular burden and cognitive performance, which could not be replicated in our study. The fact that our subjects had a relatively low cumulative medical and cardiovascular risk burdens might explain this observation.
According to our results, the severity of depression, and the presence of apathy, MPS, and executive dysfunction were independent predictors of functional performance in depressed subjects. The findings were similar to those reported for community-dwelling Chinese elderly with questionable dementia.7-9 Age, education level, medical burdens, and cardiovascular risk burden were not significant predictors of functional ability. The findings also echoed the observations by Alexopoulos et al26 that patients with depression-executive dysfunction (DED) syndrome had reduced fluency, impaired visual naming, loss of interest in activities, psychomotor retardation, poor understanding of their disease, and pronounced disability. Major contributors to disability in patients with DED syndrome were psychomotor retardation, depressive symptomatology, and loss of interest in activities. Executive dysfunction is strongly related to instrumental ADL (IADL) impairment in depressed elderly patients.27 Kiosses and Alexopoulos28 found that impairment in initiation / perseveration had the most prominent effect in the presence of depressive symptoms and affected IADL in such elderly. Sanders et al29 found associations between components of executive dysfunction (Trial B, Mattis-IP scores) and functional disability that were independent of depression. Since both geriatric depression and executive dysfunction often occur in patients with frontostriatal impairment, these observations raise the question of whether disability is an early indicator of impairment of the frontal and prefrontal areas.
Based on our findings, 2 mechanisms were proposed to explain the functional disability among depressed subjects. First, depressed elderly were apathetic and lacked interest in participating in joyful activities. They were unlikely to initiate or persist with complex and cognitively demanding tasks or hobbies. Secondly, they had executive dysfunctions and difficulties in planning, organisation, active problem- solving, anticipation of possible consequences, monitoring the accuracy and the effectiveness of their own behaviour. Executive processes are fundamental to the daily functioning of depressed older adults, and dysfunction may lead to a lack of compensatory strategies that improve outcomes in late-life depression and increase dependency. Clinicians should be aware that both executive deficits and depression correlate with poorer overall functioning and should consider incorporating more thorough cognitive and functional assessments into their evaluations of older patients who are depressed. Specific interventions targeting executive dysfunction and functional impairment might benefit specific subgroups of late-onset depression.
The strengths of this study were the inclusion of a heterogeneous sample of elderly with late-onset depression to maximise the generalisability of findings, and the use of established and validated measures of depression, cognitive function, and functional ability. However, we recruited a clinical sample with mild-to-moderate depressive syndromes. The generalisability of the results to community- dwelling elderly with subsyndromal depression in primary care needs to be confirmed in other studies. Our cross- sectional analyses only allowed us to examine associations between factors but we could not confirm the underlying causal relationship. Moreover, the correlations between mood symptoms, cognitive test scores and functional scores were only modest.
Our study highlighted the importance of multidimensional evaluation of geriatric depressed patients. Treatment should also aim at remission of depressive symptoms, and amelioration of cognitive impairment and functional disability. Future research about the trajectory of depression remission and functional decline could enrich knowledge about the bidirectional relationship between depression and functional disability.
In conclusion, late-onset depression affects mood, cognition and functional ability in the elderly. Our observations supported the functional importance of executive dysfunction and depression in the depressed elderly. Lack of interest and motivation, depressive mood, compounded by behavioural abnormalities (resulting from executive dysfunction), may account for functional disability in elderly subjects with late-onset depression.
References
- Boone KB, Lesser IM, Miller BL, Wohl M, Berman N, Lee A, et al. Cognitive functioning in older depressed outpatients: relationship of presence and severity of depression to neuropsychological test scores. Neuropsychology 1995;9:390-8.
- Lichtenberg PA, Ross T, Millis SR, Manning CA. The relationship between depression and cognition in older adults: a cross-validation study. J Gerontol B Psychol Sci Soc Sci 1995;50:P25-P32.
- Sheline YI, Barch DM, Garcia K, Gersing K, Pieper C, Welsh-Bohmer K, et al. Cognitive function in late life depression: relationships to severity, cerebrovascular risk factors and processing speed. Biol Psychiatry 2006;60:58-65.
- Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review: Soc Sci Med 1999;48:445-69.
- Beekman AT, Deeg DJ, Braam AW, Smit JH, Van Tilburg W. Consequences of major and minor depression in later life: a study of disability, well-being and service utilization. Psychol Med 1997;27:1397-409.
- Lyness JM, Heo M, Datto CJ, Ten Have TR, Katz IR, Drayer R, et al. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Ann Intern Med 2006;144:496-504.
- Lam LC, Tam CW, Chiu HF, Lui VW. Depression and apathy affect functioning in community active subjects with questionable dementia and mild Alzheimer’s disease. Int J Geriatr Psychiatry 2007;22:431-7.
- Tam CW, Lam LC, Chiu HF, Lui VW. Characteristic profiles of instrumental activities of daily living in Chinese older persons with mild cognitive impairment. Am J Alzheimers Dis Other Demen 2007;22:211-7.
- Tam CW, Lam LC, Lui VW, Chan WC, Chan SS, Chiu HF, et al. Clinical correlates of functional performance in community- dwelling Chinese older persons with mild cognitive impairment. Int Psychogeriatr 2008;20:1059-70.
- Chan S, Jia S, Chiu H, Chien WT, R Thompson D, Hu Y, et al. Subjective health-related quality of life of Chinese older persons with depression in Shanghai and Hong Kong: relationship to clinical factors, level of functioning and social support. Int J Geriatr Psychiatry 2009;24:355-62.
- Chan SW, Chiu HF, Chien WT, Goggins W, Thompson D, Hong B. Predictors of change in health-related quality of life among older people with depression: a longitudinal study. Int Psychogeriatr 2009;21:1171-9.
- American Psychiatric Association Committee on Nomenclature and Statistics. Diagnostic and statistical manual of mental disorders (DSM- IV), 4th ed. Washington, D.C.: American Psychiatric Association; 1994.
- Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. Br J Psychiatry 1982;140:556- 72.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62.
- Chiu HF, Lee HC, Chung WS, Kwong PK. Reliability and validity of the Cantonese version of the Mini-Mental State Examination — a preliminary study. Journal of Hong Kong College of Psychiatrists 1994;2:25-8.
- Chu LW, Chiu KC, Hui SL, Yu GK, Tsui WJ, Lee PW. The reliability and validity of the Alzheimer’s Disease Assessment Scale Cognitive Subscale (ADAS-Cog) among the elderly Chinese in Hong Kong. Ann Acad Med Singapore 2000;29:474-85.
- Lam LC, Ho P, Lui VW, Tam CW. Reduced semantic fluency as an additional screening tool for subjects with questionable dementia. Dement Geriatr Cogn Disord 2006;22:159-64.
- Reitan RM, Wolfson D. Category Test and Trail Making Test as measures of frontal lobe functions. Clin Neuropsychol 1995;9:50-6.
- Mok CC, Siu AM, Chan WC, Yeung KM, Pan PC, Li SW. Functional disabilities profile of Chinese elderly people with Alzheimer’s disease — a validation study on the Chinese version of the disability assessment for dementia. Dement Geriatr Cogn Disord 2005;20:112- 9.
- Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 1994;44:2308- 14.
- Leung VP, Lam LC, Chiu HF, Cummings JL, Chen QL. Validation study of the Chinese version of the neuropsychiatric inventory (CNPI). Int J Geriatr Psychiatry 2001;16:789-93.
- Stern MB. The clinical characteristics of Parkinson’s disease and parkinsonian syndromes: diagnosis and assessment. In: Stern MB, Hurtig HI, editors. The comprehensive management of Parkinson’s disease. New York: PMA Publishing Corp.; 1988: 34-9.
- Conwell Y, Forbes NT, Cox C, Caine ED. Validation of a measure of physical illness burden at autopsy, the Cumulative Illness Rating Scale. J Am Geriatr Soc 1993;41:38-41.
- Baudic S, Tzortzis C, Barba GD, Traykov L. Executive deficits in elderly patients with major unipolar depression. J Geriatr Psychiatry Neurol 2004;17:195-201.
- Alexopoulos GS. Frontostriatal and limbic dysfunction in late-life depression. Am J Geriatr Psychiatry 2002;10:687-95.
- Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. ‘Vascular depression’ hypothesis. Arch Gen Psychiatry 1997;54:915-22.
- Kiosses DN, Klimstra S, Murphy C, Alexopoulos GS. Executive dysfunction and disability in elderly patients with major depression. Am J Geriatr Psychiatry 2001;9:269-74.
- Kiosses DN, Alexopoulos GS. IADL functions, cognitive deficits, and severity of depression: a preliminary study. Am J Geriatr Psychiatry 2005;13:244-9.
- Sanders ML, Lyness JM, Eberly S, King DA, Caine ED. Cerebrovascular risk factors, executive dysfunction, and depression in older primary care patients. Am J Geriatr Psychiatry 2006;14:145-52.