East Asian Arch Psychiatry 2011;21:99-107
ORIGINAL ARTICLE
LK Chan, ECS Yu, SY Li
陈立基、余枝胜、李常友
Dr Lap-Kei Chan, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Dr Edwin Chi-Shing Yu, MH, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Dr Seung-Yau Li, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Kwai Chung Hospital, Hong Kong SAR, China.
Address for correspondence: Dr Lap-Kei Chan, Kwai Chung Hospital, Hong Kong SAR, China.
Tel: (852) 2990 3000; Email: clkedmond@gmail.com
Submitted: 14 December 2010; Accepted: 31 March 2011
Abstract
Objectives: To identify the prevalence and correlates of depression among Chinese peritoneal dialysis patients.
Methods: In this cross-sectional study, from October 2007 to June 2008, 141 peritoneal dialysis patients were recruited from a local renal clinic. All participants were interviewed by the first author using the Chinese bilingual version of the Structured Clinical Interview for DSM-IV (Axis I) to identify patients suffering from major depressive disorders and psychiatric illnesses associated with elevated depressive symptoms. Socio-demographic and clinical data were collected. Co-morbid medical illnesses and perceived social support were assessed by standardised questionnaires, namely: the Cumulative Illness Rating Scale, and the Chinese version of Multidimensional Scale of Perceived Social Support (MSPSS- C).
Results: The point prevalence of a current major depressive episode was 16%; another 21% had had at least 1 past episode of major depression. Low MSPSS-C score, muscle cramps, chronic back pain, joint stiffness, and receipt of Social Security Allowance were independent correlates of elevated depressive symptoms.
Conclusions: The prevalence of depression was higher in Chinese patients receiving peritoneal dialysis. Independent correlates are useful to help physicians identify patients suffering from depressive disorders in busy renal clinics.
Key words: Depression; Peritoneal dialysis; Prevalence
摘要
目的:检视腹膜透析患者其抑鬱症的现患率和相关因素。
方法:这项横断面研究於2007年10月至2008年6月期间,纳入本地一间肾科诊所的141名腹膜透析患者。研究以中文及双语版DSM-IV(轴I)临床面谈辨识抑鬱症患者;研究并收集社会人口学和临床数据,又以标準评估工具——疾病累计评分表(CIRS)和中文版社会支持感知量表(MSPSS-C)分别评估患者共存的疾病和感知社会支持。
结果:抑鬱症的时点现患率为16%,另有21%患者曾患上至少1次抑鬱症。MSPSS-C低分、肌肉痉挛、慢性背痛、关节僵硬和接受公共福利津贴与抑鬱症病徵呈独立相关性。
结论:华籍腹膜透析患者的抑鬱症现患率风险较高。在繁忙的肾科诊所运作中,上述的独立相关因素有助医护人员辨识可能患有抑鬱症的患者。
关键词:抑鬱症、腹膜透析、现患率
Introduction
End-stage renal disease (ESRD) is a chronic condition in which the kidneys can no longer regulate electrolytes and acid-base balance, and excrete waste products at a level necessary for day-to-day life.1 In 2005 the incidence of dialysis-dependent ESRD in Hong Kong was 173 per million inhabitants, while the prevalence of ESRD was 965 per million.2 The Hospital Authority of Hong Kong provides treatment for 95% of these dialysis patients. About 81% of them receive peritoneal dialysis (PD) and the rest receive haemodialysis (HD). Although PD is a life-saving treatment, it is only a partial replacement for the excretory function of the kidneys. Patients are faced with complicated and demanding treatment regimens, which include dietary and fluid restrictions, together with complex medication schedules. Prolonged survival in patients with ESRD is associated with various functional impairments in almost all body systems. These lead to negative effects on quality of life.3 Epidemiological and clinical studies worldwide have revealed a higher prevalence of depression in PD patients than in the general population.4-6 It is important to identify depression in these patients because it is associated with impaired quality of life as well as reduced survival.7 Yet in this group, depression is commonly unrecognised and underdiagnosed.8 Moreover, there has been no local study examining the prevalence of depression in PD patients by standardised psychiatric interview. This study therefore aimed to explore the prevalence of depression among local Chinese patients receiving PD and investigate the corresponding correlates of depression.
Literature Review
Little data are available for the prevalence of depression, specifically in patients receiving PD. Most studies focused on the point prevalence of depression in ESRD patients receiving various types of renal replacement therapy. A recent systematic review of 60 such studies indicated that the prevalence of depression varied widely from 5% to 58%, with an average of 27%.9 The disparity in reported prevalence rates may be partially explained by the difference in instruments used to detect depression. It is also important to distinguish between the diagnosis of major depressive disorder and the symptoms of depression or a high level of depressive affect. In a study in the United States, about half of the dialysis patients were categorised as depressed using the Beck Depression Inventory (BDI), compared with 17% using the Multiple Affect Adjective Check List, but only in 5% of those sampled by clinical interview using the DSM-III criteria.10 Other confounding factors that may explain prevalence differences include: the types of renal replacement therapy the subjects were receiving, sampling methods, and the variability of medical service provision. Standardised assessment tools such as the Structured Clinical Interview for the DSM-IV (SCID) may partially resolve problems of great disparity in the prevalence rate of depression in medically ill patients, because they can enhance the reliability of the diagnoses.
Literature review indicates that most studies used self-rating scales to identify depression in ESRD patients; only a few employed standardised psychiatric interviews. If the prevalence of depression was to be re-evaluated with the data from these studies,10-12 rates of depression in ESRD patients would be in the range of 5% to 34%. Among these 4 studies, only 2 included PD patients, while the other 2 only recruited those having HD.7,10 If only the 2 studies with PD patients were considered, the prevalence of depression was relatively lower.
Only 2 studies (from overseas) examined depression specifically in PD patients. Einwohner et al6 examined 66 PD patients using the Zung Self-Rating Depression Scale and identified depressive symptoms in 32% of them. Another American study used the BDI to screen for depression followed by clinical interviews in 320 PD patients.5 Among these, 134 (42%) scored ≥ 11; of whom 69 agreed to further evaluation. Sixty patients were diagnosed with depression after a further clinical interview.
The data on the prevalence of depression in PD patients in Hong Kong are even more limited. One study used the Hospital Anxiety and Depression Scale to examine the prevalence of psychological problems in Chinese PD patients, and reported that 46% of the patients had elevated depressive symptoms.13 Another 2 studies conducted in China used the Hamilton Depression Scale to study the rate of depression in PD patients,14,15 both of which noted a prevalence rate of about 56%.
Methods
This was a cross-sectional study conducted in collaboration with the Renal Unit of the Department of Medicine and Geriatrics of Princess Margaret Hospital (PMH), Hong Kong. Approval of its protocol was obtained from the Clinical Research Ethics Committee of the Kowloon West Cluster of the Hong Kong Hospital Authority. Assessment of subjects took place in the specialist dialysis outpatient clinic from October 2007 to June 2008.
Sampling Method
When only studies on ESRD patients which included PD patients and using standardised clinical interviews were included, the prevalence of current major depression ranged from 5% to 8%.7,10 With 0.05 as the desired precision and a 95% confidence interval (CI), the required sample size ranged from to 73 to 115. A similar local study on HD patients had a response rate of 83%.12 When these data were taken into consideration with other potential causes of patient loss during the recruitment process, 175 was determined to be the number needed for the sample.
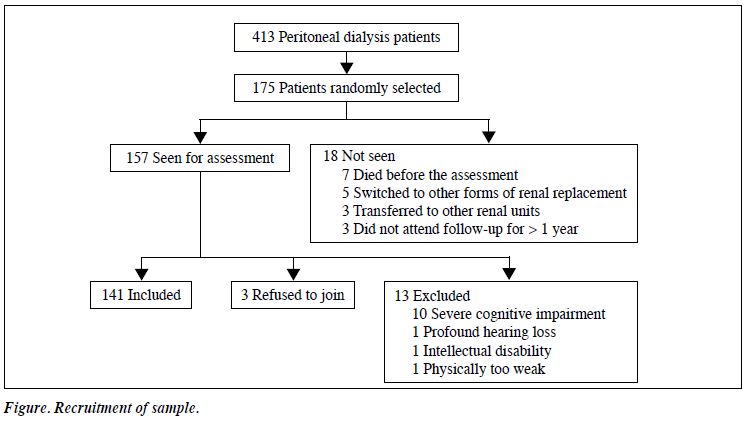
A list of 413 patients receiving PD in PMH was generated on 2 October 2007. Of these, 383 were receiving continuous ambulatory peritoneal dialysis (CAPD) while 30 were receiving automated peritoneal dialysis (APD). The method of random sampling was adopted to select 175 subjects out of these 413 patients. In all, 175 random numbers (in the range 1 to 413) were generated by computer software. The initial target subjects were then selected from the full patient list, according to the random numbers generated. Corresponding patients were then interviewed to identify those who met the following inclusion criteria: (1) age ≥ 18 years; and (2) currently receiving PD as an outpatient of PMH. Those who were: (1) non-Chinese; (2) unable to communicate in Cantonese; (3) having severe communication difficulties (e.g. profound hearing impairment); (4) having significant cognitive deficits (e.g. dementia and intellectual disability); and (5) physically too weak to complete the assessment interview, were excluded.
Procedures
After obtaining their written consent, the targeted subjects were assessed in a single interview by the first author. For all patients, the Chinese version of the Mini-Mental State Examination was performed to detect any cognitive impairment. The cut-off scores were ≤ 18 for those who had not received any formal education, ≤ 20 for those with 1 or 2 years of education, and ≤ 22 for those with more than 2 years of education.16 Those who scored below the cut-off point were excluded. Background information including socio- demographic variables, medical history, and psychiatric history were recorded. The Cumulative Illness Rating Scale (CIRS) was used to rate the severity of co-existing medical illnesses.17 The Chinese bilingual version of the Structured Clinical Interview for DSM-IV (Axis I) [CB-SCID-I] was administered by the first author to look for the presence of any psychiatric diagnosis.18 Finally, the Chinese version of the Multidimensional Scale of Perceived Social Support (MSPSS-C) was used to assess each subject’s perceptions about the level of social support by family, friends, and significant others.19
Statistical Analyses
Data were analysed using the Statistical Package for the Social Sciences, Windows version 15.0. Descriptive statistics were used to show the socio-demographic and clinical profile of the sample. Independent variables were compared between subjects with elevated depressive symptoms (EDS) and non-depressed (ND) subjects. The Pearson Chi-square test was performed for categorical variables. The Fisher’s exact probability test was used for 2 x 2 tables when the cells had expected counts of less than Independent sample t tests were used to compare groups with continuous variables. The odds ratios (OR) of each of the independent variables were calculated to determine the direction and magnitude of their association with depressive symptoms. Two-tailed analyses were used in all tests. In the second stage, variables with a p value < 0.1 in the bivariate analysis were adopted as potential independent correlates and entered into the logistic regression analysis. Multicollinearity among the potential independent correlates was checked. Logistic regression analysis was then employed to examine the impact of different variables on the development of depressive symptoms. The statistical significance level was set at p < 0.05, unless otherwise specified.
Results
Of the 175 PD patients randomly selected as the initial target sample, 18 were excluded (7 had died; 5 had switched to other forms of renal replacement; 3 were transferred to other hospitals; 3 had defaulted regular follow-up). From the remaining 157 patients, a further 13 were excluded (10 for severe cognitive impairment; and 1 each due to profound hearing loss, intellectual disability, and physical weakness), whilst 3 others declined to participate in this study. Therefore, the final sample consisted of 141 patients, which accounted for 81% of the original randomly selected target sample (Fig).
Comparison of Recruited and Non-recruited Subjects
No difference was found in terms of gender (p = 0.44) and age (p = 0.26) between the patients who were recruited and not recruited.
Socio-demographic Characteristics
The mean (standard deviation [SD]) age of the sample was 57 (13) years, of whom 42% (n = 60) were female. The majority were married (67%). More than half had attained secondary school education or above (54%), and most lived in public housing (57%). Only a minority (14%) were in active employment, and 42 (30%) were receiving Social Security Allowance.
Medical and Psychiatric Background
In all, 127 (90%) of the patients in the sample were receiving CAPD and the remainder received APD. The mean (SD) duration of PD that the patients had received at the time of assessment was 3.6 (3.2) years.
Hypertension was the most prevalent co-morbid chronic disease, and affected 85% of the sample. Cardiovascular complications were common; about 20% had a history of stroke and / or ischaemic heart disease. As expected, visual impairment and sexual dysfunction were also common as they were closely related to the cardiovascular risk. Most subjects (70%) had at least 3 chronic physical illnesses other than renal disease, and more than 20% had at least 5 chronic physical co-morbidities.
In 10 (7%) of the patients, there was a psychiatric history before starting PD; 2 had attempted suicide in the past, 9 had a family history of mental illness, and 4 had received active psychiatric treatment for their mental illness (1 was receiving specialist psychiatric care).
Prevalence of Current and Past Depressive Disorders
With the use of CB-SCID-I, the prevalence of patients meeting the criteria for a current major depressive episode was 16%. Another 29 (21%) of the patients had at least 1 past episode of major depression but did not meet the criteria for current depression. Therefore, the lifetime prevalence of major depressive disorders among the sample was 37%. A further 7 (5%) patients were diagnosed with psychiatric conditions associated with EDS (Table 1).
Associated Factors of Depression
Considering the small number of patients in each subgroup of the depression-related diagnosis, it was not appropriate to conduct a separate analysis on such subjects. Patients with current major depression, past major depression in partial remission, and psychiatric conditions associated with depressive features were grouped together, and collectively called the EDS group. This group of patients was compared with the remaining patients, which was called the ND group in this study.

Bivariate Analysis
Socio-demographic Variables
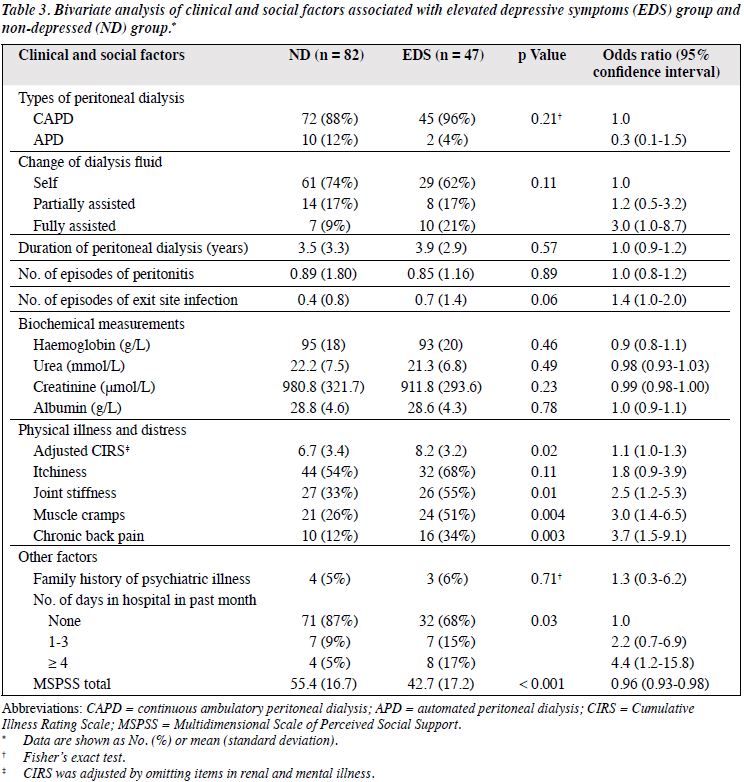
There were 47 patients in the EDS group, as opposed to 82 in the ND group. The EDS patients were less likely to have a religion (OR = 2.5, 95% CI = 1.1-5.5), and more were associated with receipt of Social Security Allowance (OR = 2.2, 95% CI = 1.0-4.6) [Table 2].
Clinical Variables
The EDS patients were more likely to be suffering from distressing muscle cramps (OR = 3.0) and chronic back pain (OR = 3.7), and endured longer recent hospital stays and lower MSPSS-C scores. They also scored higher in the adjusted CIRS (OR = 1.1, 95% CI = 1.0-1.3) and were more likely to be suffering from joint stiffness (OR = 2.5, 95% CI = 1.2-5.3) [Table 3].
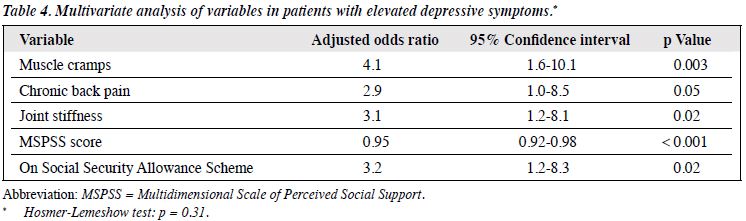
Multivariate Analysis
In the second stage of the statistical analysis, all variables with a p < 0.1 in the bivariate analysis were entered into the logistic regression analysis, with EDS and ND as dependent variables. Physical distress from muscle cramps, chronic back pain, joint stiffness, low MSPSS-C scores, and receipt of Social Security Allowance were the correlates of EDS; respective adjusted ORs were: 4.1, 2.9, 3.1, 0.95, and 3.2 (Table 4). Both multivariate models showed a good fit according to the Hosmer-Lemeshow test (p > 0.31).
Discussion
In the present study, 16% of the sample met the DSM-IV criteria for a current major depressive episode, and a further 21% had a history of major depression. Therefore, the lifetime prevalence of major depressive disorders was 37%. This prevalence rate of current major depression is in the lower quartile of the wide range of 5% to 58% reported in the literature.9 However, caution is needed before a direct comparison is made between studies, as there are variations in the definition of depression, sampling methods, and diagnostic tools. If only studies using standardised diagnostic tools are included, the prevalence rates in ESRD patients appear to be lower (5-34%).10-12 In this sense, the prevalence rate of major depression in this study is in the middle of the reported rates.

Since this study had no matched control group from the general population, no definite conclusion can be drawn regarding the relative risk of depressive disorder in PD patients. However, the lifetime prevalence rate of major depression in our sample was much higher than that reported in an epidemiological study in the general population in Hong Kong (1.3% for men and 2.4% for women).20 Another more recent local study reported the 12-month prevalence of major depression among Hong Kong adults to be 8.4%, which was also lower than the rate of current major depression in our sample.21 Therefore, it is postulated that the prevalence of depressive disorder in local PD patients is higher than that in the general population, though further research using matched controls is needed to confirm this assertion.
Correlates of Depression
In this study, several independent factors associated with EDS in PD patients were identified. The negative association between perceived social support and depression is consistent with the findings in the existing literature,22,23 while associations between depression and specific physical symptoms as well as utilisation of social security assistance were seldom mentioned in previous studies.
Perceived Social Support
The relationship between perceived social support and stress has long been researched in various studies worldwide.24 A major finding was that perceived availability of social support provides a buffer against stressful events through its interaction between the stressors and stress reactions.24 Our study confirmed the importance of perceived social support in PD patients, showing that a lower MSPSS-C score was associated with an increased likelihood of depression. This is understandable because PD patients often suffer from physical co-morbidities like visual impairment and stroke, that make them at least partially dependent on others for both the treatment and activities of daily living. As demonstrated in this study, the great majority of patients were either unemployed or retired, and hence also largely financially dependent on their families. Their treatment and physical disabilities significantly decreased their social network. Emotional support from family and friends are therefore of paramount importance.
A number of studies on ESRD patients have demonstrated that greater levels of social support were associated with reduced depressive affect, less suicidal ideation, and higher satisfaction with life.22,23 In predicting adjustment to stressful life events, Callaghan and Morrissey25 found that perceived social support is more important than actually receiving such support, which is also in line with findings of the current study.
Physical Distress
In the present study, physical distress significantly associated with EDS included: muscle cramps, chronic back pain, and joint stiffness. Studies concentrating on the relationship between physical symptoms and depression in PD patients are limited. A recent cross-sectional study that examined common physical complaints in PD patients concluded that such symptoms and depression are strongly associated with quality of life.26 Regarding specific physical symptoms in dialysis patients, there was only 1 study that reported joint stiffness and muscle cramps as common stressors,27 but without any attempt to establish the relationship with the depressive symptoms.
Chronic back pain was identified as a significant correlate for EDS, which relationship has long been documented.28 The presence of chronic pain in medically ill patients was reported to be associated with more depressive symptoms and worse depression outcomes, including: lower quality of life, decreased work function, and increased health care utilisation.29 On the other hand, depression in patients with pain is associated with more pain complaints.30 Well- established evidence suggests that depression is strongly associated with chronic back pain,30 whilst the present study confirms the relationship specifically in PD patients.
Social Security Assistance
Utilisation of social security assistance was another correlate in our EDS patients. This is an important finding, as the impact of subsistence on social security assistance in depression has seldom been explored. The Comprehensive Social Security Assistance Scheme in Hong Kong provides a safety net for those who cannot support themselves financially. It is designed to bring their income up to a prescribed level to meet basic needs. Although unemployment was a common problem in PD patients,31 the present study demonstrated that neither employment status nor monthly household income was associated with the risk of EDS in these subjects. It is therefore reasonable to believe that the utilisation of social security assistance should not be seen as equivalent to being out of work or having a low household income. Notably, receipt of the assistance also encompasses other meanings, such as the social stigma of being viewed as lazy or weak which might have an adverse psychological impact.32
Implications for Clinical Practice
The present study showed a high prevalence of depression in the sample, while less than 20% of these depressed patients were receiving psychiatric treatment. The correlates of depression we identified can help physicians recognise patients who might benefit from psychiatric treatment. Other than patient’s clinical variables and physical distress, social factors such as lack of perceived social support and utilisation of Social Security Allowance were also shown to correlate significantly with EDS. Thus, apart from clinical information, physicians should also pay attention to the social and family background of their patients, since the amelioration of these factors could well improve psychological well-being and hence clinical outcomes of dialysis patients.
As in many other chronic illnesses, a multidisciplinary approach involving nephrologists, psychiatrists, social workers, and dialysis nursing staff is optimal when dealing with mental illness. A considerable proportion of the PD patients have physical impairments and are therefore reluctant to attend separate clinics for their psychiatric problems. A joint clinic with comprehensive services offered by nephrologists and psychiatrists may enhance compliance to psychiatric treatment.
Limitations and Directions for Further Research
The cross-sectional design of this study did not allow the authors to draw conclusion on the causal relationship between depression and its associated factors. The significant correlates like physical distress and social problems can be the causes or the consequences of depression. Nevertheless, they provide guidance for planning future prospective studies to establish the risk factors for depression in PD patients.
Interviewer bias was possible, since the whole study was designed and conducted by the first author. Such bias was minimised by using the standardised clinical interview to ascertain the psychiatric diagnosis and by blinding the interviewer to the self-rated questionnaire results. Data collection relied heavily on retrospective recall, thus recall bias was unavoidable. Collecting information from patients’ friends and family may help to enhance the information reliability if more resources including time were available.
In addition, it took 9 months to complete the data collection process. Fifteen patients were not interviewed because during the study period they had died, switched to other forms of renal replacement therapy, or were transferred to other medical units. From the data analysis, there was no evidence that they were different in terms of age or gender. However, they may have had a different profile in terms of illness severity or presence of medical co-morbidity. Furthermore, although most dialysis services in Hong Kong are provided by the Hospital Authority, a small proportion of patients receive dialysis in the private sector. Both reasons would affect the generalisability of the findings. Similarly, future studies can also enhance the generalisability of the results by pooling samples from multiple renal centres across Hong Kong.
The present study did not have a matched control group. This made the estimation of the relative risks of depression in PD patients compared to that of the general population and those with other chronic illnesses difficult. We therefore attempted to compare our findings with prevalence rates of depression reported in other local studies. However, the validity of such comparisons is limited by difference in study settings. Furthermore, we could not differentiate whether the increased risk of depression was associated with renal failure per se or PD itself. In future studies, suitable control groups can be recruited to address this issue.
Conclusion
This study showed that patients receiving PD were at higher risk of developing depression. However, physicians often underestimated or even ignored this possibility. Chronic physical distress, receiving Social Security Allowance, and low perceived social support were noted to be associated with depression. The presence of these correlates should alert physicians to pay extra attention to such high-risk patients and hence increase recognition of this condition. Further research with a prospective design is needed to examine the causal relationship for depression in PD patients and its associated risk factors.
References
- Kasper DL, Braunwald E, Hauser S, Longo D, Jameson JL, Fauci AS. Harrison’s principles of internal medicine. 16th ed. New York City: McGraw-Hill; 2005.
- Chau KF. Renal Registry. Central Renal Committee. Hong Kong: Hospital Authority; 2006.
- Lew SQ, Piraino B. Quality of life and psychological issues in peritoneal dialysis patients. Semin Dial 2005;18:119-23.
- Wuerth D, Finkelstein SH, Ciarcia J, Peterson R, Kliger AS, Finkelstein FO. Identification and treatment of depression in a cohort of patients maintained on chronic peritoneal dialysis. Am J Kidney Dis 2001;37:1011-7.
- Wuerth D, Finkelstein SH, Kliger AS, Finkelstein FO. Chronic peritoneal dialysis patients diagnosed with clinical depression: results of pharmacologic therapy. Semin Dial 2003;16:424-7.
- Einwohner R, Bernardini J, Fried L, Piraino B. The effect of depressive symptoms on survival in peritoneal dialysis patients. Perit Dial Int 2004;24:256-63.
- Craven JL, Rodin GM, Johnson L, Kennedy SH. The diagnosis of major depression in renal dialysis patients. Psychosom Med 1987;49:482-92.
- Wang PL, Watnick SG. Depression: a common but underrecognized condition associated with end-stage renal disease. Semin Dial 2004;17:237-41.
- Murtagh FE, Addington-Hall J, Higginson IJ. The prevalence of symptoms in end-stage renal disease: a systematic review. Adv Chronic Kidney Dis 2007;14:82-99.
- Smith MD, Hong BA, Robson AM. Diagnosis of depression in patients with end-stage renal disease. Comparative analysis. Am J Med 1985;79:160-6.
- 1 O’Donnell K, Chung JY. The diagnosis of major depression in end- stage renal disease. Psychother Psychosom 1997;66:38-43.
- Chau OL. Psychiatric morbidity in patients receiving hemodialysis. Hong Kong: Kwai Chung Hospital; 2002.
- Lai KY, Chan HS, Leung VK, Mok LY, Chow KM, Szeto CC. Prevalence of psychological problems in Chinese peritoneal dialysis patients. Hong Kong J Nephrol 2005;7:82-9.
- Han Q, Dong J, Fan M. Anxiety and depression of patients in peritoneal dialysis. Chin Ment Health J 2004;18:24-6.
- Liu ZZ. Depressive state complicated with chronic renal failure treated by continuous ambulatory peritoneal dialysis [in Chinese]. Zhonghua Shen Jing Jing Shen Ke Za Zhi 1989;22:168-70.
- Chiu HF, Lam LC, Chi I, Leung T, Li SW, Law WT, et al. Prevalence of dementia in Chinese elderly in Hong Kong. Neurology 1998;50:1002- 9.
- Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc 1968;16:622-6.
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry 1992;49:624-9.
- Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: a confirmation study. J Clin Psychol 1991;47:756-61.
- Chen CN, Wong J, Lee N, Chan-Ho MW, Lau JT, Fung M. The Shatin community mental health survey in Hong Kong. II. Major findings. Arch Gen Psychiatry 1993;50:125-33.
- Lee S, Tsang A, Kwok K. Twelve-month prevalence, correlates, and treatment preference of adults with DSM-IV major depressive episode in Hong Kong. J Affect Disord 2007;98:129-36.
- Ye XQ, Chen WQ, Lin JX, Wang RP, Zhang ZH, Yang X, et al. Effect of social support on psychological-stress-induced anxiety and depressive symptoms in patients receiving peritoneal dialysis. J Psychosom Res 2008;65:157-64.
- Soykan A, Arapaslan B, Kumbasar H. Suicidal behavior, satisfaction with life, and perceived social support in end-stage renal disease. Transplant Proc 2003;35:1290-1.
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985;98:310-57.
- Callaghan P, Morrissey J. Social support and health: a review. J Adv Nurs 1993;18:203-10.
- Hong E, Bernardini J, Fried L, Samsonov M, Pirain B. The relationship between symptoms, depression, and quality of life in peritoneal dialysis patients. Adv Perit Dial 2006;22:83-7.
- Lok P. Stressors, coping mechanisms and quality of life among dialysis patients in Australia. J Adv Nurs 1996;23:873-81.
- Davison SN, Jhangri GS. The impact of chronic pain on depression, sleep, and the desire to withdraw from dialysis in hemodialysis patients. J Pain Symptom Manage 2005;30:465-73.
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med 2003;163:2433-45.
- Tang NK, Salkovskis PM, Hodges A, Wright KJ, Hanna M, Hester J. Effects of mood on pain responses and pain tolerance: an experimental study in chronic back pain patients. Pain 2008;138:392-401.
- Lye WC, Chan PS, Leong SO, van der Straaten JC. Psychosocial and psychiatric morbidity in patients on CAPD. Adv Perit Dial 1997;13:134-6.
- Walker R. Positive welfare and social exclusion. Centre for research in social policy briefings 1998;12:1-2.


