East Asian Arch Psychiatry 2011;21:108-114
ORIGINAL ARTICLE
Miss Das Priscilla, MSc, Department of Community Health, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia.
Dr Awang Hamidin, MBBS, Department of Psychiatry, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia.
Prof Mohd. Zain Azhar, MD, Department of Psychiatry, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia.
Prof Khin Ohnmar Naing Noorjan, MBBS, Department of Psychiatry, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia.
Dr Mohd. Said Salmiah, MD, Department of Community Health, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia.
Dr Khalid Bahariah, MBBS, Department of Medicine, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia.
Address for correspondence: Ms Priscilla Das, Department of Psychiatry, Faculty of Medicine and Health Sciences, University Putra Malaysia, 43400 Serdang, Selangor Darul Ehsan, Malaysia.
Tel: (60) 017-2043 187; Fax: (60) 0389414629; Email: daspriscilla@yahoo.com
Submitted: 1 February 2011; Accepted: 24 May 2011
Abstract
Objectives: To determine the relationship between major depressive disorder, anxiety disorders and the quality of life of haematological cancer patients.
Methods: This cross-sectional study was conducted at Ampang Hospital Kuala Lumpur, Malaysia, a tertiary referral centre hospital for haematological cancer. The Mini-International Neuropsychiatric Interview was used for the diagnosis of major depressive disorder and anxiety disorders. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire was utilised to measure patients’ quality of life.
Results: A total of 105 haematological cancer patients were included in the study with response rate of 100%. Major depressive disorder correlated with almost all domains of the quality of life, except the pain scores. Logistic regression showed that insomnia and financial difficulties were related to major depressive disorder. Different anxiety disorders also correlated with quality of life in specific domains. The leading anxiety disorders that correlated mostly with quality-of-life scales were generalised anxiety disorder, followed by obsessive-compulsive disorder, social anxiety disorder, as well as post-traumatic stress disorder and panic disorder with agoraphobia (p < 0.05).
Conclusions: Psychological treatment along with medication and intervention should be implemented to improve the overall quality of life and psychiatric disorder symptoms among the haematological cancer patients.
Key words: Anxiety; Depression; Hematologic neoplasms; Quality of life
摘要
目的:检视抑鬱症和焦虑症与血液癌症患者生活素质之关係。
方法:这项横断面研究於马来西亚吉隆坡安邦医院进行,这是一所针对血液癌症患者的大学转介医院。研究以简明国际神经精神访谈诊断抑鬱症和焦虑症,并以欧洲癌症研究和治疗组织癌症患者生活素质问卷调查为患者评估其生活素质。
结果:共105名血液学癌症患者参与研究,回应率为100%。除了疼痛,抑鬱症与大部份生活素质範畴皆呈相关。逻辑迴归分析显示与抑鬱症相关的因素包括失眠和财政困难。在特定範畴内,不同焦虑症也与生活素质相关。至於与生活素质最相关的主要焦虑症类别顺序为:广泛性焦虑症、强迫症、惊恐症伴随惧旷症、社交焦虑症和创伤後应激障碍(p < 0.05)。
结论:心理治疗加上药物和介入治疗应到位,以改善血液癌症患者的整体生活素质和精神病情。
关键词:焦虑、抑鬱症、血液肿瘤、生活素质
Introduction
In 2008, it was estimated to have as many as 12.7 million newly diagnosed cancer cases and nearly 7.6 million cancer deaths reported worldwide.1 The scenario is almost the same in Malaysia, as cancer is classified as one of the major health problems,2 where the annual cancer incidence was 30,0003; 21,773 cancer cases were reported in Peninsular Malaysia alone.4 Cancer was the fourth leading cause of death in Malaysia in 1998.5
The present study mainly concentrated on haematological cancers such as leukaemia, lymphoma, and myeloma.6 Statistics showed that lymphomas was 1 of the 10 leading cancers in Peninsular Malaysia (prevalence, 3.2%). In addition, a comparison by gender showed that 2 of the 10 most frequent cancers in males were lymphomas (4.2%) and leukaemias (3.6%), whereas lymphomas (2.4%) is one of the 10 most common cancers in females.4
There is growing research on both the psychological and physical state of haematological cancer patients.7-10 A study by Prieto et al11 reported a 44% prevalence of psychiatric morbidity which met the DSM-IV criteria for a psychiatric diagnosis among haematological cancer patients. Depression7 and anxiety10,11 are the most common psychiatric disorders diagnosed among cancer patients. In addition, the causes of poor quality of life among the cancer patients have been widely investigated, and depression and anxiety were found to be possible predictors.12
To the best of our knowledge, there is no published research on the association of major depressive disorder (MDD) and anxiety with quality of life in Malaysia. This study was therefore designed to investigate any correlations between MDD / anxiety and quality of life among haematological cancer patients seen at a Malaysian hospital, and to find out significant predictors of MDD.
Methods
Sampling was performed at Ampang Hospital in Kuala Lumpur, Malaysia. Patients with haematological malignancies (non-Hodgkin’s lymphoma, acute myelogenous leukaemia, acute lymphoblastic leukaemia, Hodgkin lymphoma, and others) were referred to this tertiary referral centre. Data collection occurred from May 2009 to December 2009. A cross-sectional study design was used in this study. All admitted haematological cancer patients were approached based on fulfilment of eligibility criteria consisting of: (1) a confirmed haematological cancer diagnosis; (2) knowledge of English, Malay, Mandarin or Tamil language; (3) age ≥ 15 years; and (4) sufficient cognition to be interviewed. Consent was obtained from the patients. Socio-demographic and clinical data were retrieved from respective medical records. The Ministry of Health and the Faculty of Medicine and Health Sciences, University Putra Malaysia Ethical Committees approved this study.
The study used the Mini-International Neuro- psychiatric Interview version 6.0.0, a questionnaire to diagnose MDD and anxiety disorders.13 The following of its modules were used: ‘A’ for MDD; ‘D’ for panic disorder; ‘E’ for agoraphobia; ‘F’ for social anxiety disorder (SAD); ‘G’ for obsessive-compulsive disorder (OCD); ‘H’ for post- traumatic stress disorder (PTSD); and ‘N’ for generalised anxiety disorder (GAD). Each question entailed a ‘Yes’ or ‘No’ response. The entire questionnaire was based on DSM-IV and ICD-10 criteria, and had good sensitivity and specificity for the diagnosis of disorders such as MDD (96% sensitivity; 88% specificity).14
Quality of life among cancer patients was evaluated using the validated 30-question European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30).15,16 It consists of 15 scales, including: physical functioning, role functioning, cognitive functioning, emotional functioning, social functioning, fatigue, pain, nausea / vomiting, dyspnoea, insomnia, appetite loss, constipation, diarrhoea, financial difficulties, and global health status. Each question was rated from 1 to 4 with scores corresponding to ‘not at all’, ‘a little’, ‘quite a bit’ and ‘very much’, except that questions 29 and 30 were rated 1 to 7 (‘very poor’ to ‘excellent’ for global health status).15 Each rated scale was used to compute a score ranging from 0 to 100 according to the scoring manual of EORTC QLQ-C30. Higher scores for the functioning scale and global health status indicated better functioning and better global health status, respectively; higher scores on the other scales indicated more symptoms.17
The Statistical Package for the Social Sciences version 17.0 was used to analyse the results. Non-parametric, point- biserial Spearman’s rho correlation was used to determine the correlation between psychiatric disorders and the quality of life with one-tailed significance test (p < 0.05). Predictors of MDD by quality-of-life domains and other factors, such as socio-demographic and clinical factors, were also determined.
Results
A total of 105 respondents (100% response rate) with a mean (range) age of 40 (15-78) years were included in the study; 52% were female. The study included patients with various haematological cancers, including non-Hodgkin’s lymphoma (24%), acute myelogenous leukaemia (23%), acute lymphoblastic leukaemia (14%), and Hodgkin’s lymphoma (11%). In this sample, the prevalence of MDD was 25% and the overall prevalence of anxiety disorders was 31% (n = 32); breakdown by type of anxiety disorders ranged from 1% to 25% (Table 1).
Table 2 illustrates the relationship between MDD and quality of life. Major depressive disorder had a weak negative relationship with the majority of the quality-of- life scales, including: global health status (r = –0.33; p = 0.001), physical functioning (r = –0.25; p = 0.01), role functioning (r = –0.23; p = 0.01), cognitive functioning (r = –0.22; p = 0.01), and social functioning (r = –0.35; p < 0.001). However, a more significant negative relationship was found in emotional functioning (r = –0.45; p < 0.001). The depressed patients had more impaired global health status and reduced functioning (negative correlation) compared with non-depressed subjects. In terms of symptom scales for the quality of life, all of the relationships were weakly positive with MDD, including: fatigue (r = 0.29; p = 0.001), nausea and vomiting (r = 0.31; p = 0.001), insomnia (r = 0.31; p = 0.001), appetite loss (r = 0.21; p = 0.02), diarrhoea (r = 0.21; p = 0.02), and financial difficulties (r = 0.36; p < 0.001). Positive but very weak associations between MDD and dyspnoea (r = 0.17; p = 0.04) and constipation (r = 0.18; p = 0.04) were also found. The positive relationship means that the depressed patients had more symptoms than the non-depressed.
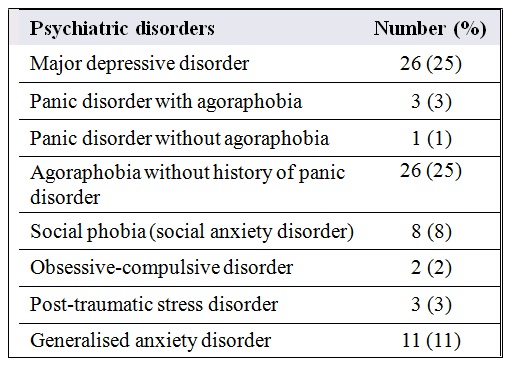
Table 2 also shows that anxiety disorders such as panic disorder with agoraphobia (current), SAD, OCD (current), PTSD, and GAD correlated with certain quality- of-life scores. Panic disorder without agoraphobia did not correlate with any quality-of-life domain. Current panic disorder with agoraphobia correlated negatively with cognitive functioning (r = –0.22; p = 0.01) and positively with symptoms of dyspnoea (r = 0.21; p = 0.02). These relationships were all weak, except in the case of pain which showed a very weak negative association with MDD (r = –0.17; p = 0.05). This result explains why patients with panic disorder with agoraphobia had impaired cognitive functioning, more symptoms of dyspnoea and, interestingly, less pain when compared with patients without the disorder.
There was a negative correlation between SAD and emotional functioning (r = –0.39; p < 0.001), cognitive functioning (r = –0.29; p = 0.001), and social functioning (r = –0.21; p = 0.02), whereas there was a positive correlation with financial difficulties (r = 0.23; p = 0.01). Thus, patients
Table 2. Correlation between major depressive disorder (MDD), anxiety disorders and quality of life.*

Abbreviations: SAD = social anxiety disorder; OCD = obsessive-compulsive disorder; PTSD = post-traumatic stress disorder; GAD = generalised anxiety disorder.
* Figures in bold denote statistical significance. with SAD had impaired emotional functioning, cognitive functioning, social functioning, and more financial difficulties when compared with those without SAD.
Current OCD yielded very weak negative correlations with global health status (r = –0.16; p = 0.05), role functioning (r = –0.16; p = 0.05), and cognitive functioning (r = –0.18; p = 0.03), and a weak negative correlation with emotional functioning (r = –0.21; p = 0.02). Nausea and vomiting (r = 0.20; p = 0.02), appetite loss (r = 0.20; p = 0.02) and constipation (r = 0.16; p = 0.05) correlated positively with OCD but very weakly.
Post-traumatic stress disorder had a weak negative association with social functioning (r = –0.17; p = 0.04), cognitive functioning (r = –0.13; p = 0.01) and a weak positive correlation with dyspnoea (r = 0.25; p = 0.01) compared with other patients without the disorder. Finally, a moderate negative relationship was found between GAD and emotional functioning (r = –0.51; p < 0.001), whereas it had a weak relationship with role functioning (r = –0.25; p = 0.01), cognitive functioning (r = –0.21; p = 0.02), physical functioning (r = –0.18; p = 0.03), and social functioning (r = –0.16; p = 0.05).
Patients with GAD also had weak positive correlations with insomnia (r = 0.21; p = 0.02), constipation (r = 0.25; p = 0.01), and financial difficulties (r = 0.23; p = 0.01). Thus, patients with GAD had reduced emotional, role, cognitive, physical and social functioning, as well as more symptoms of insomnia, constipation, and financial difficulties when compared with non-GAD patients.
Further analysis of the data was performed by binary logistic regression to determine quality-of-life domains and other variables that may act as predictors of MDD (Table 3). The putative predictors started with social functioning, nausea and vomiting, insomnia, and financial difficulties. The rationale for selecting these 4 independent variables was because they showed significance (p < 0.05) in the binary logistic regression model. The final model Nagelkerke R2 value showed that about 41.4% of the variation in the MDD outcome was explained by the logistic model. Correlations between the predictors did exist but were weak to moderate (r = –0.07 to –0.45). The overall accuracy of this model was 80% with the sensitivity (42%) and specificity (92%) sufficient to predict patients having MDD with a predicted probability of ≥ 0.5. Among the independent variables, social functioning (odds ratio = 0.98; p = 0.01), insomnia (odds ratio = 1.02; p = 0.03), and financial difficulties (odds ratio = 1.02; p = 0.02) were found to be significant and were related to MDD.
Discussion
This study was designed to assess the relationship of MDD
Table 3. Logistic regression model of major depressive disorder with quality of life.
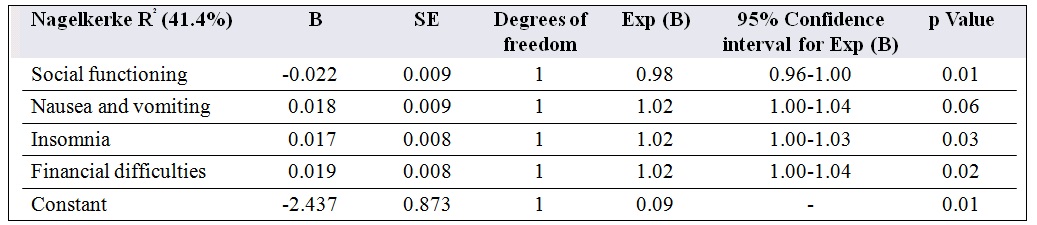
Abbreviations: SE = standard error; B = values for logistic regression equation for predicting the dependent variable from the independent variable.
and anxiety to the quality of life. Negative relationships were found between MDD and all 5 functioning aspects of quality of life, including emotional, physical, role, cognitive, and social functioning. Global health status also correlated negatively with MDD. These results are in agreement with those of other studies, which found that depression was associated with poorer physical,10,18,19 role,10 cognitive,10,18 emotional,10,18,19 and social functioning,10,18,19 as well as global health status.10,18 The inverse correlation between the quality-of-life score with depression and anxiety was noted in a previous study of leukaemia and lymphoma patients.20
Regarding symptoms, MDD had positive relationships with most domains except pain. Symptoms such as fatigue,18 sleep disturbance,19 appetite loss,19 financial difficulties,19 and nausea18 were also associated with depression among the cancer patients. Symptoms of vomiting were reported as distressing by the patients when they occurred.21 Other symptoms, such as constipation, were predictors for depression among incurable cancer patients.19
It seems possible that these results could be due to side-effects of treatment, since these haematological cancer patients under active treatment have limitations in physical functioning, poor appetite, and fatigue compared with other patients.9 Another study reported that cancer patients appeared to have poor quality of life even prior to high-dose chemotherapy treatment.21 The results of logistic regression indicated that patients’ social functioning, insomnia, and financial difficulties were significantly associated with MDD. This study produced results which corroborate the finding that insomnia is a predictor for depression among the incurable cancer patients.19 The diminished quality of life among the haematological cancer patients caused by depression or anxiety are important risk factors.20
The prevalence of anxiety among the cancer patients varies from 10% to 50%. Anxiety disorder can be described as a form of response to any treatment.22 Panic disorder with agoraphobia is associated with cognitive functioning, dyspnoea, and pain symptoms. The present findings seem to be consistent with other studies among the haematological cancer patients10 and advanced cancer patients,18 which found that anxiety is associated with impairment in cognitive functioning. Poor cognitive functioning and dyspnoea were reported predictors for anxiety among the cancer patients.19
Even though patients showed only low levels of pain, among advanced cancer patients this symptom correlated with emotional and physical functioning.18
Post-traumatic stress disorder is associated with social functioning and dyspnoea domains. Anxiety has a relationship with social functioning among cancer patients10,18 and dyspnoea is one of the predictors of anxiety in cancer patients.19
In this study, patients with SAD had impaired emotional, cognitive, and social functioning, as well as more financial difficulties compared with those without the disorder. Anxiety causes emotional distress and interferes with their functioning, besides affecting patient compliance. Cancer patients with anxiety often respond to the diagnosis of cancer, its treatment, its remissions and its relapses. The anxiety of cancer patients often contributes to delays in diagnosis and affects survival in about 10% to 20% of patients (including long-term survival).22 This finding supports previous research that cancer patients with anxiety experience impaired emotional, cognitive and social functioning.10,18
Reduced emotional, cognitive and social functioning were also predictors for anxiety in cancer patients.19
Our study also revealed that patients with OCD correlated with impaired global health status, role functioning, cognitive functioning, emotional functioning, nausea and vomiting, appetite loss, and constipation. These findings are consistent with research showing impairment in quality of life,19 role functioning,10,18 cognitive functioning,10,18 emotional functioning,10,18,19 and nausea18 among patients with anxiety. In a previous study,19 these 3 types of functioning were also predictive of anxiety among cancer patients.
On the other hand, patients with GAD were associated with all the 5 functioning aspects of quality of life, as well as insomnia, constipation, and financial difficulties. Patients with anxiety disorders after a cancer diagnosis might be constructive in solving problems and not necessarily prone to abnormal anxiety. Abnormal anxiety classified as disruptive23 is defined as “symptoms of anxiety that are out of proportion to the level of threat, which persist or deteriorate without intervention and cause distress or disruption of functioning.” The 4 most important situations that may cause anxiety to patients ensue while waiting for the results of their diagnosis, before procedures, prior to major diagnostic tests, and associated with operations.24 Patients with anxiety have associated poor cognitive functioning,10,18 emotional functioning,10,18,19 social functioning,10,18 physical functioning,10 and sleep disturbance.19 These findings further support all the above-mentioned variables as predictors of anxiety in cancer patients.19
The present study contributes additional evidence which suggests that major depressive episodes and anxiety disorders are correlated with quality of life. Psychological treatment, along with medication and intervention, should be implemented as one the best methods to improve quality of life among cancer patients18 and to enhance outcomes in the treatment of cancer.8
Limitations
The self-rated questionnaires were answered by the patients themselves, and some questions were explained to the patients to clarify what was being asked. Thus, the truthfulness of this result depends solely on the patients’ perspectives and memory at the time of the interview. The results for binary logistic regression in the study should be interpreted with caution, because the study did not specify the longitudinal course of the temporal sequence of the psychiatric diagnosis and cancer. Thus, it may be difficult to state the real predictors of the MDD in the study. Finally, the number of patients, especially with panic disorder with agoraphobia, panic disorder without agoraphobia, OCD, and PTSD, were limited, thus the correlation analysis should be interpreted with caution.
Conclusions
These findings suggest that, in general, MDD and anxiety disorders are associated with aspects of quality of life. Major depressive disorder correlates with almost all domains of the quality of life, except the pain scores. The 2 important factors that related to MDD were insomnia and financial difficulties. The anxiety disorder that correlated most with quality of life was GAD, followed by OCD, SAD, PTSD, and panic disorder with agoraphobia.
Acknowledgements
The authors would like to acknowledge University Putra Malaysia for the financial aid under Research University Grant Scheme (RUGS), project no: 04-03-08-0458RU (91463) and Ministry of Science, Technology and Innovation for their National Science Fellowship award. We would like to thank the director of Ampang Hospital, 2 consultant haematologists, Dr Ong Tee Chuan and Dr Chang Kian Meng, the staff of the haematological cancer units, and all of the patients who participated in the study.
References
- Ferlay JS, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008, Cancer incidence and mortality worldwide: IARC CancerBase No. 10. Website: http://globocan.iarc.fr. Accessed 1 Apr 2011.
- Lim GC. Overview of cancer in Malaysia. Jpn J Clin Oncol 2002;32 Suppl:S37-42.
- Lim AK, Lim GC. The burden of advanced cancer in Malaysia. Proceedings of the National Hospice Conference; Penang, Malaysia. Penang: National Cancer Society of Malaysia, Penang Branch; 1993: 13-8.
- Zainal AO, Zainudin MA, Nor Saleha IT. Malaysian Cancer Statistics- Data and Figure Peninsular Malaysia 2006. National Cancer Registry. Ministry of Health Malaysia: Kuala Lumpur; 2006. Website: http:// www.moh.gov.my/v/c_report?mode=public. Accessed 1 Oct 2008.
- Vital Statistics Malaysia. Kuala Lumpur: Malaysia Department of Statistics; 1999.
- Lichtman MA. Battling the hematological malignancies: the 200 years’ war. Oncologist 2008;13:126-38.
- Prieto JM, Atala J, Blanch J, Carreras E, Rovira M, Cirera E, et al. Role of depression as a predictor of mortality among cancer patients after stem-cell transplantation. J Clin Oncol 2005;23:6063-71.
- Prieto JM, Atala J, Blanch J, Carreras E, Rovira M, Cirera E, et al. Patient-rated emotional and physical functioning among hematologic cancer patients during hospitalization for stem-cell transplantation. Bone Marrow Transplant 2005;35:307-14.
- Johnsen AT, Tholstrup D, Petersen MA, Pedersen L, Groenvold M. Health related quality of life in a nationally representative sample of haematological patients. Eur J Haematol 2009;83:139-48.
- Pamuk GE, Harmandar F, Ermantaş N, Harmandar O, Turgut B, Demir M, et al. EORTC QLQ-C30 assessment in Turkish patients with hematological malignancies: association with anxiety and depression. Ann Hematol 2008;87:305-10.
- 1 Prieto JM, Blanch J, Atala J, Carreras E, Rovira M, Cirera E, et al. Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. J Clin Oncol 2002;20:1907-17.
- Ozalp E, Cankurtaran ES, Soygür H, Geyik PO, Jacobsen PB. Screening for psychological distress in Turkish cancer patients. Psychooncology 2007;16:304-11.
- Sheehan D, Janavs J, Harnett-Sheehan K, Sheehan M, Gray C, Lecrubier Y, et al. M.I.N.I: Mini International Neuropsychiatric Interview English version 6.0.0 DSM-IV; 2009. Website: http://www. psy.uwa.edu.au/user/andrew/MINI600.pdf. Accessed 1 Jan 2009.
- Sheehan DV, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Bonara LI, et al. Reliability and validity of the MINI International Neuropsychiatric Interview (MINI): according to the SCID-P. European Psychiatry 1997;12:232-41.
- Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365-76.
- Mustapa N, Yian LG. Pilot-testing the Malay version of the EORTC questionnaire. Singapore Nursing Journal 2007;34:16-20.
- Fayers P, Aaronson NK, Bjordal K, Curran D, Groenvold M; on behalf of the EORTC Quality of Life Study Group. EORTC QLQ-C30 scoring manual. 3rd ed. Belgium, Brussels: EORTC Quality of Life Group; 2001.
- Smith EM, Gomm SA, Dickens CM. Assessing the independent contribution to quality of life from anxiety and depression in patients with advanced cancer. Palliat Med 2003;17:509-13.
- Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, Vlahos L. Assessment of anxiety and depression in advanced cancer patients and their relationship with quality of life. Qual Life Res 2005;14:1825-33.
- Montgomery C, Pocock M, Titley K, Lloyd K. Individual quality of life in patients with leukaemia and lymphoma. Psychooncology 2002;11:239-43.
- Larsen J, Nordström G, Björkstrand B, Ljungman P, Gardulf A. Symptom distress, functional status and health-related quality of life before high-dose chemotherapy with stem-cell transplantation. Eur J Cancer Care (Engl) 2003;12:71-80.
- Liénard A, Merckaert I, Libert Y, Delvaux N, Marchal S, Boniver J, et al. Factors that influence cancer patients’ anxiety following a medical consultation: impact of a communication skills training programme for physicians. Ann Oncol 2006;17:1450-8.
- Franks F, Faux SA. Depression, stress, mastery, and social resources in four ethnocultural women’s groups. Res Nurs Health 1990;13:283-92.
- Ashbury FD, Findlay H, Reynolds B, Mckerracher K. A Canadian survey of cancer patients’ experiences: are their needs being met? J Pain Symptom Manage 1998;16:298-306.


