East Asian Arch Psychiatry 2013;23:13-20
ORIGINAL ARTICLE
Dr Justina Yat-Wa Liu, RN, PhD, School of Nursing, Hong Kong Polytechnic University, Hong Kong SAR, China.
Prof. Claudia Lai, RN, PhD, School of Nursing, Hong Kong Polytechnic University, Hong Kong SAR, China.
Dr David Dai, MBBS, FHKAM (Medicine), Department of Medicine and Therapeutics, Prince of Wales Hospital, Hong Kong SAR, China.
Ms Sylvia Ting, RN, MScN, School of Nursing, Hong Kong Polytechnic University, Hong Kong SAR, China.
Dr Kin Choi, MFM, FRCPI, FHKAM (Medicine) (Family Medicine), DGM, PDGM, PDCPM, Former President, The Hong Kong Medical Association, Hong Kong SAR, China.
Address for correspondence: Dr Justina Yat-Wa Liu, School of Nursing, Hong Kong Polytechnic University, Hong Kong SAR, China.
Tel: (852) 2766 4096; Fax: (852) 2364 9663; email: justina.liu@polyu.edu.hk
Submitted: 23 October 2012; Accepted: 27 December 2012
Abstract
Objective: To explore by postal survey the different attitudes towards management of patients with dementia in physicians with and without dementia training.
Methods: A questionnaire was sent to 7669 members of the Hong Kong Medical Association, which represents 61% of all locally registered medical practitioners.
Results: In all, 448 questionnaires were returned (response rate: 6%). Among these, there were 34 questionnaires with missing data or the respondents indicated that they were either retired or not in practice. Therefore, only 414 questionnaires were used in analysis. Among these, 82 (20%) had received dementia training, 310 (75%) had not, and 22 (5%) did not indicate their choice. Twelve statements were used to explore various attitudes about dementia care. Exploratory factor analysis showed that there were 2 strong factors: confidence and negative views. The mean scores of these 2 factors were significantly different in physicians with and without dementia training. With respect to management of patients with dementia, dementia-trained physicians had significantly greater confidence (mean [standard deviation (SD)] = 5.21 [1.34]) than those who were non-trained (mean [SD] = 3.57 [1.40]; p < 0.001). Conversely, non-trained physicians had significantly stronger negative views (mean [SD] = 3.89 [1.24]) on dementia care than those who were trained (mean [SD] = 3.12 [1.36]; p < 0.001).
Discussion: These findings suggest that providing a certain level of dementia care training for physicians is an effective way to improve confidence in managing patients with dementia, and thereby decrease possible negative attitudes towards such care.
Key words: Data collection; Dementia; Education, medical, continuing
摘要
目的:以邮寄问卷方式,检视并比较曾接受认知障碍症治疗专科训练和没有接受训练的医生对认知障碍症患者的治疗态度。
方法:问卷寄往7669名香港医学会会员(占本港註册医生61%)。
结果:共收回448份问卷(回应率:6%);由於其中34份问卷的数据不完整或被访者已退休或已没行医,最终只有414份问卷被用作分析。当中,82名(20%)医生表示曾接受认知障碍症治疗训练,310名(75%)表示没有,其馀22名(5%)没有给予答案。问卷包括12项有关对治疗认知障碍症态度的声明。探索性因素分析显示2项关键因素:信心和负面观点。这 2项因素的平均得分於上述2组医生间有明显差别。曾接受训练的医生(平均得分:5.21,标準差:1.34)在治疗认知障碍症方面较没有训练的医生(平均得分:3.57,标準差:1.40; p < 0.001)更有信心;而後者(平均得分:3.89,标準差:1.24;p < 0.001)也较前者(平均得分:3.12,标準差:1.36)对治疗持负面态度。
结论:研究结果认为,为医生提供治疗认知障碍症的相关训练,有助改进其治疗的信心,从而减少对治疗态度的负面观点。
关键词:数据收集、认知障碍症、持续医疗教育
Introduction
Dementia is known to have a high prevalence worldwide. The alarming rate at which populations are ageing and the longer lifespans evident around the world will make it a dominant issue in the coming decades. There is speculation that this will intensify the problems associated with dementia care. Thus, the screening and management of patients with dementia (PWD) should be within the scope of general practitioner (GP) services. General practitioners play a fundamental role in diagnosing and managing dementia, and only refer patients to specialists for managing complicated cases.1,2 However, there is ample evidence showing that patients and families are unsatisfied with the process of seeking a diagnosis and getting subsequent care and treatment from family physicians.3,4 Suboptimal dementia care is partly contributed to by inadequate knowledge regarding appropriate management, often because physicians fail to recognise dementia-related symptoms,4-6 and are unaware of support for PWD available in the community.7 Several studies have shown that GPs lack competence and confidence in diagnosing and managing dementia.8,9 For example, one-third of the participants in the survey by Turner et al7 revealed that they lacked confidence when confirming the diagnosis, and two-thirds lacked confidence in managing PWD, especially their behavioural and functional problems. In part, suboptimal care is also due to their negative attitude towards dementia. Many GPs believe that treatment options for dementia are limited,10 are sceptical about the advantages of dementia medications,11 consider making a diagnosis to be difficult,3,12 and feel that making such a diagnosis could do more harm than good.13,14
These observations imply that continued dementia training for GPs is necessary to improve their knowledge, and thereby also their competence and confidence in management of the condition. Thus, more positive experiences in managing PWD may eventually shift their negative attitudes towards dementia.5,7,15 Although education and training were identified in a number of studies as a means of developing confidence and positive attitudes towards dementia management, there are no studies on how dementia training affects the confidence and attitudes of physicians. Studies generally explored GPs’ understanding or opinions on dementia management instead of attributes related to the receipt of special training in dementia care. This survey therefore highlights different attitudes towards dementia management among physicians who had or had not undergone dementia training. These findings were extracted from a larger survey aimed at exploring factors associated with the observed gap between the prevalence (which is fairly widespread) and treatment of dementia (which is relatively minimal in terms of the percentage of those afflicted). The detailed findings of the entire survey will be reported elsewhere.
Methods
This was a postal survey of physicians in Hong Kong and was conducted from December 2010 to March 2011. A questionnaire was designed based on a review of the literature and clinician expertise in relevant specialties. The questionnaire comprised 4 sections. Section 1 collected respondents’ demographic information. Section 2 included 14 questions to explore physicians’ diagnoses and dementia management patterns. Respondents were also asked whether or not they chose to manage PWD. The design of section 3 was adapted from the instrument developed by Turner et al7 with approval. The original instrument7 contained 10 statements which aimed to evaluate GPs’ confidence in treating PWD, which was slightly different from the objectives of this survey. Therefore, 2 of these statements about family concerns were deleted and with addition of 4 new statements, this section contained a total of 12 statements which aimed to investigate respondents’ attitudes towards treating PWD. Statements 1 to 3 related to exploring physicians’ perceptions on treating PWD. Statements 4 and 5 related to investigating physicians’ activeness in making the diagnosis and treating PWD were added in the new scale for the present study. The respondents were requested to rate their level of acceptance to each statement on a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). Section 4 consisted of 7 questions about respondents’ training experience in dementia management. The content validity index of the questionnaire was 3.24 out of 4, as assessed by a panel of experts in the field. A pilot survey was conducted on a convenience sample of 10 GPs. No particular concerns were raised during the pilot study. This paper reports the differences of attitudes in the management of PWD in physicians with and without special training in dementia care. Ethics approval was obtained from the Human Subjects Ethics Sub-committee of The Hong Kong Polytechnic University. Other findings from this survey, such as physicians’ patterns of treating PWD, will be reported elsewhere.
An invitation letter accompanying the questionnaire explained the purpose of the survey and was disseminated to 7669 active members of the Hong Kong Medical Association (HKMA). This represented 61% of all registered medical practitioners in Hong Kong. Four weeks after sending out the initial postal questionnaire, a reminder was sent to all non-respondents. To maintain anonymity, mailing of the questionnaire was arranged by the staff of HKMA not involved in the survey. The research team had no access to HKMA members’ information.
Data Analysis
Predictive Analytics Software (PASW) 18.0 was used to manage the data. Descriptive statistics were used to describe the general survey findings. Comparisons between groups (i.e. physicians with / without dementia training) were tested using the t test for continuous data and the Z test for categorical data. Principal component factor analysis was carried out on the results obtained from the attitude scale (Section 3). All statistical tests were 2-tailed and a probability of 0.05 was considered significant.
Results
Sample
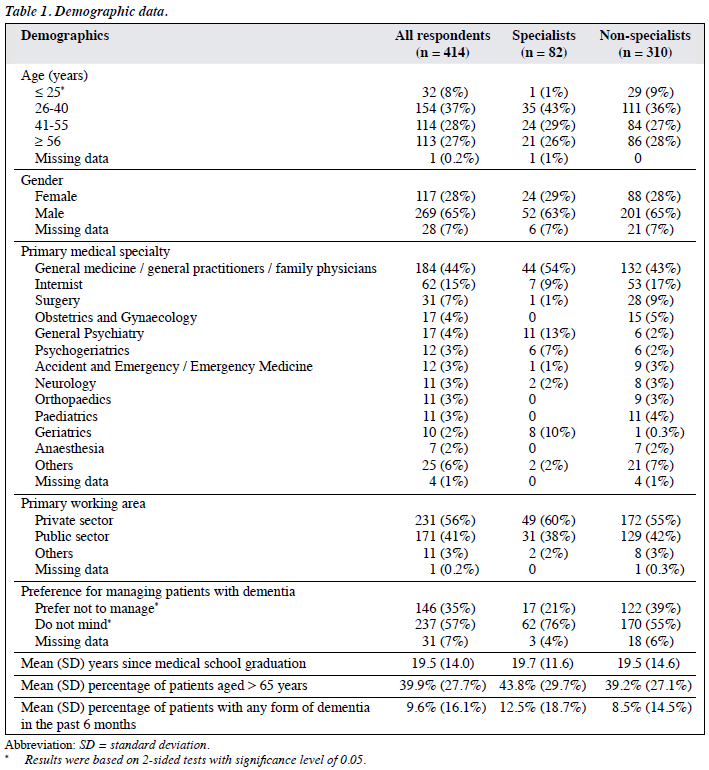
Of 7669 questionnaires sent, 448 were returned (response rate, 6%). Among these, 370 were fully completed, 12 respondents indicated that they were either retired or not in practice, and 66 questionnaires were only partially completed. Of the partially completed questionnaires, 22 were excluded from the analysis as they did not give their answers to key questions or their answers were not discernible. Finally, 414 questionnaires were used in the analysis. Detailed demographic data of the 414 respondents are presented in Table 1. Among all respondents, only 38 (9%) held a diploma in geriatric medicine, while 56 (14%) had received other specialised training in dementia care. Overall, 82 respondents (20%) were classified as physicians with special training in dementia care if they answered “yes” to either or both of these questions. Conversely, 310 respondents (75%) answered “no” to these 2 questions were defined as physicians with no specific training in dementia care. Also, 22 respondents (5%) did not indicate whether or not they had received any training in dementia care. There was no difference between them for most of their demographic characteristics, except that a significantly larger percentage of physicians aged ≤ 25 years had received no special dementia training. Physicians who had received dementia training had treated a significantly greater percentage of PWD in the previous 6 months (12.5% vs. 8.5%). In addition, a significantly higher percentage of physicians without special training preferred not to manage PWD compared with those with such training. About 39% (n = 122) of physicians without special training but only 21% (n = 17) of those with such training opted out of managing PWD.
Attitudes to Dementia Care
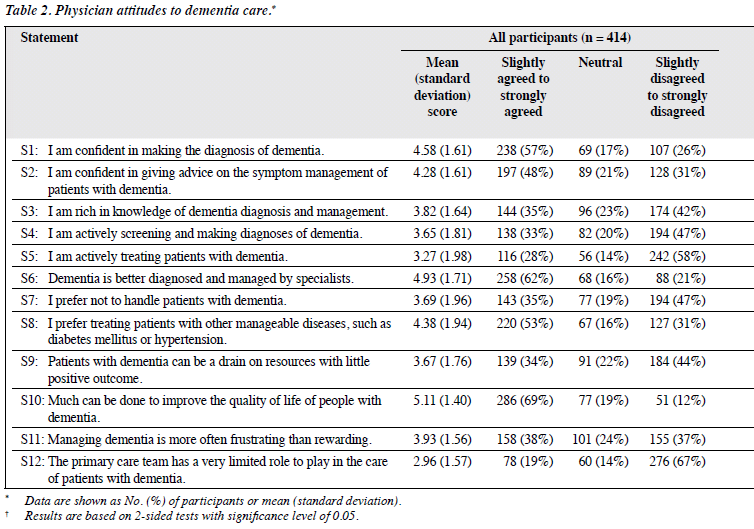
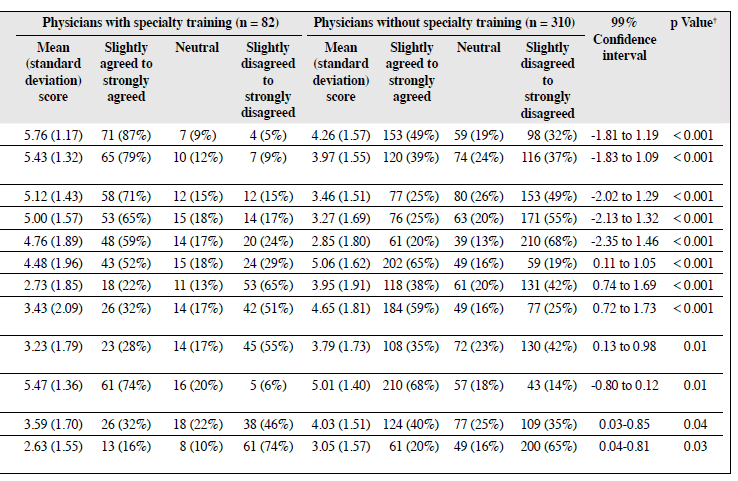
Details of physicians’ attitudes towards dementia care are shown in Table 2. The statements on improving the quality of life of PWD (5.11), dementia better diagnosed and managed by specialists (4.93), and their confidence in diagnosing dementia (4.58) elicited the most agreement among all respondents; whereas statements on activeness of screening and diagnosing dementia (3.65), activeness of treating PWD (3.27), and the belief that primary care team has limited role in the care of PWD (2.96) attained the lowest mean scores.
When comparing mean scores of all statements rated by physicians with and without special dementia training, there were significant differences (Table 2). The top 4 statements with which larger proportions of physicians with dementia training agreed included confidence in diagnosing dementia (87%), confidence in giving advice on symptom management of PWD (79%), knowledgeability of dementia diagnosis and management (71%), and improvement in the quality of life of PWD (74%). Interestingly, the former 3 were all about the confidence and knowledge related to dementia care. Regarding physicians without such training who agreed with these 3 statements, the percentages were between 25% and 49%. Not only the statement on improving the quality of life of PWD agreed by the majority of physicians with dementia training, but also scored the largest percentage of agreement among those without dementia training (68%). The second and third largest percentage of agreement among physicians without dementia training were for dementia better diagnosed and managed by specialists (65%) and their preference of treating patients with other manageable diseases (59%).
The statement that elicited the most disagreement by the physicians with dementia training was their belief that the primary care team has limited role in the care of PWD (74%), when compared with 65% in those without such training. In other words, both groups believed that the primary care team has an important and extended role to play in dementia care. The items with the second and third largest number of physicians with dementia training disagreed to were unwillingness to treat PWD (65%) and PWD as a drain on resources (55%), respectively. Disagreement to activeness of treating PWD (68%) elicited the greatest proportion by physicians without dementia training, whereas disagreement to screening and making diagnoses (55%) came third.
Exploratory factor analysis was conducted to expose the underlying factors within the attitude test, as well as to evaluate construct validity. Tests of the suitability of the data for factor analysis were satisfactory, with the Kaiser-Meyer-Olkin test value of 0.86, exceeding the recommended value of 0.6,16 and Bartlett’s Test of Sphericity17 reaching significance (p < 0.001) after deleting the statements of dementia better diagnosed and managed by specialists and much can be done to improve the quality of life of PWD.
Two sets of items from the attitude test yielded a stronger and more interpretable factor structure by principal axis factoring with varimax rotation. They were named as confidence (factor 1) and negative views (factor 2). These 2 factors explained 60% of the variance of the 10 items. Factor 1 had an initial eigenvalue of 4.69 (variance explained = 38.72%; α = 0.93; mean [standard deviation (SD)] = 3.92 [0.52]; range = 3.22-4.57); whereas Factor 2 had an initial eigenvalue of 2.11 (variance explained = 21.51%; α = 0.78; mean [SD] = 3.72 [0.52]; range = 2.96-4.38). The statements that formed each factor and their factor loadings are listed in Tables 3 and 4.
The mean scores based on the 5 statements under factor 1 and factor 2 (Table 5) were significantly different among physicians with and without dementia training. The former were slightly more confident (mean [SD] = 5.21 [1.34]) in the management of PWD than the latter (3.57 [1.40]; p < 0.001). Also, the non-trained physicians had significantly stronger negative views (mean [SD] = 3.89 [1.24]) on dementia care than those who were trained (mean [SD] = 3.12 [1.36]; p < 0.001).
Discussion
Previous studies have explored factors and challenges that affect the diagnosis, disclosure, and management of dementia by GPs.5,7,12,18 Previous workers have suggested continuous education about various aspects of dementia management as one of the major strategies for improving dementia care.5,7,15 As far as we are aware, this is the first study to investigate and compare attitudes towards dementia care among physicians with and without dementia training.
The attitude test used in this survey showed 2 strong discriminating factors, namely confidence and negative views compared with the factors (i.e. heartsink and heartfelt [sic]) identified in the study by Turner et al.7 The two current factors explained 60% of the variance of the tests after the exclusion of statements 6 and 10. Compared with our study, Turner’s factors7 only explained 47% of the variance out of the 7 statements. Obviously, physicians with specialised training in dementia care were significantly more confident in the management of patients with different manifestations of the problem, including making diagnoses, giving advice, and managing the symptoms. This small group of physicians also viewed themselves as being competent medical practitioners in screening, making diagnoses, and treating PWD. Conversely, only 25 to 49% of physicians without dementia training held similar views. This explains why more than 60% of the physicians without dementia training believed that the diagnosis of dementia was within a specialist’s domain and did not belong to the remit of general practice. Around one-third of physicians with no special dementia training expressed limited confidence in their diagnostic skills and in the management of the symptoms of dementia, which was similar to the findings by Turner et al.7 Almost half of them disagreed that they were rich in knowledge of dementia diagnosis and management, and more than half admitted that they were not actively screening and diagnosing this condition. It seems that the prevailing level of confidence drives from the level of activeness in the management of dementia.
The attitude test also revealed that respondents who had received no dementia training had significantly stronger negative views on dementia care than those who had. Negative physician attitudes may be caused by emotional responses to experiences in treating PWD.19 Exploration of their personal experiences in the process of dealing with dementia patients is beyond the scope of this paper. However, about 60% of physicians who had received no dementia training agreed that they would rather treat patients with other manageable diseases, and 40% of them agreed that dementia management was a frustrating experience. Similarly, 164 GPs in a survey by Harris et al20 felt more confident and were more willing to treat other chronic medical conditions than PWD.
As a means of developing confidence and positive attitudes in understanding and responding to dementia, previous studies as well as the current survey identified the role of education and training. Education improves physician knowledge about dementia, thereby enhancing their confidence in its management, and confidence drives them to take up a more active role in treating such patients. Thus, more education is a fundamental requirement to improve the care of this particular patient group.
Physicians’ preference for not managing PWD may be partly due to previous frustrating and unsatisfactory experiences, such frustration being reflected by their negative views and low levels of confidence in their capacity to manage PWD. We asked respondents who expressed their preference for not treating PWD (n = 146, 35%) to provide their reasons. “Dementia is best treated by specialists” and “I am not confident enough to treat PWD” were the 2 major responses. These findings echo the results of the attitude test in this survey, as well as those in several previous studies. Eighteen family physicians were interviewed by Pimlott et al15 and expressed a strong need for expert verification of their diagnoses due to the complexity of dementia. Cody et al12 found that 54% of GPs who had participated in their study reported difficulty establishing a definitive diagnosis of dementia. Time constraint was another major reason for all respondents opting out of the management of PWD. The current study shows that more than one-third of all respondents thought that managing dementia was often more frustrating than rewarding, and that treating PWD can be a drain on social resources with little positive outcome, and 19% thought that there were limited community services for this particular group of patients. Besides the physician’s input for disease management, optimal and comprehensive dementia care should include social services for behaviour management, respite care, and caregiver support. Some respondents may have experienced difficulties in providing patients and caregivers with access to the services provided by community agencies. They may have considered that their ability to manage dementia was limited, which was reflected by their more negative views towards dementia management and their preference not to treat this group of patients.
Dementia is a complex condition, both biologically and psychosocially, and is therefore challenging. This survey revealed that physicians who received dementia training were more positive, active, and ready to manage this complicated disease, which further supports the idea that continuous physician training is the key to improving the care of PWD. Besides equipping physicians with adequate medical knowledge of dementia management, physicians should also involve themselves with different community teams to provide medical advice and social support services that can meet individual patient needs. Physicians must therefore have extraordinarily diverse practical knowledge of issues that extend beyond their common medical knowledge.19 Harris et al20 suggested a broader educational approach to dementia training, emphasising the complexity of the clinical picture, comprehensive biopsychosocial care, and a greater focus on behavioural science. To enhance knowledge of dementia care by physicians, Turner et al7 suggested greater epidemiological knowledge, disclosure of the diagnosis, and management of behaviour problems as topics to target. In addition, it is suggested that physicians should enhance their knowledge of social services provided for PWD and their caregivers.
Although our respondents who had received dementia training were more confident and had fewer negative views towards dementia management, they too experienced difficulties when managing PWD. Moreover, about 30% of these physicians admitted experiencing frustration caused by managing this special patient group. Our respondents identified physicians’ levels of confidence about dementia management, time constraints, inadequate social resources, and limited community services for PWD as the major reasons for their opting out of treating these patients. Harris et al20 found that physicians who experienced less difficulty with dementia management also perceived resources and support for managing PWD to be adequate. Hence, health care systems also need to facilitate physician access to other professionals such as physiotherapists, occupational therapists, community nurses, and various social support services, so as to optimise the management and support provided to PWD and their family caregivers.
Limitations
This study was limited by selection bias and the low response rate. Although the survey included the total population of HKMA members, the respondents tended to have some kind of interest in or be committed to dementia care. Thus, they may have been a biased group. Besides, the small sample of respondents may not adequately reflect current practice with respect to dementia care. We did not have information on the practice characteristics or demographics of the physicians who chose not to participate, which limits the generalisability of the findings. Finally, whether or not they had received special dementia training was based on the respondents’ own perceptions. As this paper does not have a clear definition of dementia training, the readers need to interpret its findings with caution.
Conclusion
To reduce the demand for specialist services for PWD, screening and management of dementia should be included within the scope of GP services. Although GPs play a fundamental role in diagnosing and managing dementia, many express unwillingness to manage this group of patients. Our findings support providing special dementia training for physicians is an effective way to improve their skills, knowledge, and confidence in managing PWD, so as to overcome possible negative attitudes towards dementia care. Physicians with a certain level of dementia care training can play a more active role in managing this group of patients, so as to enable specialist services to concentrate on complicated cases. In conclusion, continuous special training in dementia care could give GPs the skills and confidence they need to be more active in the screening and management of this group of patients.
Acknowledgement
The study was funded by Eisai Hong Kong Limited.
References
- Chow TW, Binder C, Smyth S, Cohen S, Robillard A. 100 years after Alzheimer: contemporary neurology practice assessment of referrals for dementia. Am J Alzheimers Dis Other Demen 2009;23:516-27.
- Thomas H. Attitudes of primary care team to diagnosing dementia. Nurs Older People 2010;22:23-7.
- Connell CM, Boise L, Stuckey JC, Holmes SB, Hudson ML. Attitudes towards the diagnosis and disclosure of dementia among family caregivers and primary care physicians. Gerontologist 2004;44:500-7.
- Teel CS, Carson P. Family experiences in the journey through dementia diagnosis and care. J Fam Nurs 2003;9:38-58.
- Cahill S, Clark M, O’Connell H, Lawlor B, Coen RF, Walsh C. The attitudes and practices of general practitioners regarding dementia diagnosis in Ireland. Int J Geriatr Psychiatry 2008;23:663-9.
- Knopman D, Donohue JA, Gutterman EM. Patterns of care in the early stages of Alzheimer’s disease: impediments to timely diagnosis. J Am Geriatr Soc 2000;48:300-4.
- Turner S, Iliffe S, Downs M, Wilcock J, Bryans M, Levin E, et al. General practitioners’ knowledge, confidence and attitudes in the diagnosis and management of dementia. Age Ageing 2004;33:461-7.
- Boise L, Neal MG, Kaye J. Dementia assessment in primary care: results from a study in three managed care systems. J Gerontol A Biol Sci Med Sci 2004;59:M621-6.
- Boustani M, Callahan CM, Unverzagt FW, Austrom MG, Perkins AJ, Fultz BA, et al. Implementing a screening and diagnosis program for dementia in primary care. J Gen Intern Med 2005;20:572-7.
- Milne AJ, Hamilton-West K, Hatzidimitriadou E. GP attitudes to early diagnosis of dementia: evidence of improvement. Aging Ment Health 2005;9:449-55.
- Hansen EC, Hughes C, Routley G, Robinson AL. General practitioners’ experiences and understandings of diagnosing dementia: factors impacting on early diagnosis. Soc Sci Med 2008;67:1776-83.
- Cody M, Beck C, Shue VM, Pope S. Reported practices of primary care physicians in the diagnosis and management of dementia. Aging Ment Health 2002;6:72-6.
- De Lepeleire JA, Heyrman J, Baro F, Buntinx F, Lasuy C. How do general practitioners diagnose dementia? Fam Pract 1994;11:148-52.
- van Hout H, Vernooij-Dassen M, Bakker K, Blom M, Grol R. General practitioners on dementia: tasks, practices and obstacles. Patient Educ Couns 2000;29:219-25.
- Pimlott NJ, Persaud M, Drummond N, Cohen CA, Silvius JL, Seigel K, et al. Family physicians and dementia in Canada: Part 2. Understanding the challenges of dementia care. Can Fam Physician 2009;55:508-9.e1-7.
- Kaiser H. An index of factorial simplicity. Psychometrika 1974;3:31-6.
- Bartlett MS. A note on the multiplying factors for various chi square approximations. J R Stat Soc 1954;16 Series B:296-8.
- Maeck L, Haak S, Knoblauch, A, Stoppe G. Primary care physicians’ attitudes related to cognition enhancers in early dementia: a representative eight-year follow-up study in Lower Saxony, Germany. Int J Geriatr Psychiatry 2008;23:415-21.
- Foster NL. Barriers to treatment: the unique challenges for physicians providing dementia care. J Geriatr Psychiatry Neurol 2001;14:188-98.
- Harris DP, Chodosh J, Vassar SD, Vickrey BG, Shapiro MF. Primary care providers’ views of challenges and rewards of dementia care relative to other conditions. J Am Geriatr Soc 2009;57:2209-16.