East Asian Arch Psychiatry 2013;23:45-55
ORIGINAL ARTICLE
Dr Natasha Kate, MBBS, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Dr Sandeep Grover, MD, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Prof. Parmanand Kulhara, MD, FRCPsych, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Dr Ritu Nehra, PhD, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Address for correspondence: Dr Sandeep Grover, Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh 160012, India.
Tel: (91-172) 2756 807; email: drsandeepg2002@yahoo.com
Submitted: 21 January 2013; Accepted: 26 April 2013
Abstract
Objective: To study the positive aspects of caregiving and its correlates in primary caregivers of patients with schizophrenia.
Methods: A total of 100 patients with schizophrenia and their primary caregivers were evaluated. Regarding the caregivers, their positive aspects of caregiving were assessed on the Scale for Positive Aspects of Caregiving Experience (SPACE). To examine the correlates of positive aspects of caregiving, they were also assessed on the Family Burden Interview (FBI) Schedule, the Involvement Evaluation Questionnaire (IEQ), coping checklist, the Social Support Questionnaire, the World Health Organization Quality of Life–BREF (Hindi version), the WHO Quality of Life–Spirituality, Religiousness and Personal Beliefs Scale, as well as the General Health Questionnaire–12. The patients were assessed on the Positive and Negative Syndrome Scale (PANSS) and the Global Assessment of Functioning Scale.
Results: On the SPACE, the highest mean score was seen in the domain of motivation for the caregiving role (2.7), followed by that of caregiver satisfaction (2.4) and caregiver gains (2.3). The mean score was least for the domain of self-esteem and social aspect of caring (1.9). The SPACE domain of caregiver satisfaction correlated negatively with many aspects of burden as assessed by FBI Schedule and coping as assessed by the coping checklist; whereas the self-esteem and social aspect of caring domain correlated positively with worrying-urging II domain and the total IEQ score. No significant correlations between the SPACE and socio-demographics as well as most of the clinical variables were noted. Motivation for the caregiving had a positive correlation with the PANSS negative symptom scale. Multiple correlations were found between the SPACE and quality of life, suggesting that higher positive caregiving experience was associated with better quality of life in caregivers.
Conclusion: Caregivers of patients with schizophrenia do enjoy positive aspects of caregiving while taking care of their ill relatives. In these caregivers, the positive aspects of caregiving were associated with better quality of life.
Key words: Caregivers; Schizophrenia; Social support
摘要
目的:检视精神分裂症患者的主要照顾者其积极感受和相关因素。
方法:纳入共100例精神分裂症患者和其主要照顾者,并以正向照顾经验估量表(SPACE)评估照顾者的积极感受。研究使用的评估工具包括家庭负担访谈量表(FBI)、情感参与评估问卷(IEQ)、因应量表、社会支持问卷、世界卫生组织生活质量简化版量表(印地语版)、世卫组织生活质量——心灵/宗教/个人信念量表,以及一般健康问卷。患者则以阳性和阴性症状量表(PANSS)和全球功能评估量表则用作对患者的评估。
结果:SPACE显示平均得分最高是照顾者的角色(2.7),其次是他们的满意度(2.4)和得著(2.3);而平均得分最低为自尊和社会层面的关怀(1.9)。照顾者的满意度与FBI多个细项和因应量表呈负相关,而自尊和社会层面的关怀则与担忧和衝动细项和总IEQ得分呈正相关。SPACE和社会人口以至大部份临床变量间没有显著相关性。照顾的动机与PANSS阴性症状呈正相关,而SPACE与生活质量也有多重相关性,显示有积极感受的照料经验与照顾者更好生活质量相关。
结论:纵使精神分裂症患者的照顾者要照顾患病亲人,但仍可体会正面的感受。这些照顾者的积极感受与更好生活质量相关。
关键词:照顾者、精神分裂症、社会支持
Introduction
It is increasingly recognised that caring for an ill relative can also be a source of positive change in a person’s life. Although such studies are few (compared with those on caregiver burden), they suggest that caregiving also has the potential to be a source of positive transformations in people’s lives1 and can give rise to a sense of satisfaction.2 These positive changes in the lives of caregivers are understood as positive aspects of caregiving (PAC), and these take into consideration the interaction between patient’s illness and caregiver’s appraisal, perceived gains, satisfaction derived from caregiving, and the positive caregiving experiences.
Regrettably, there is no standardised formal definition of PAC. Various authors have understood PAC as caregiver gains, satisfaction, and caregiving experience.3-5 Other researchers have assessed PAC in the domains of duty / obligation, companionship, fulfilment, reward, quality of life (QOL), enjoyment, meaning,6 caregiver esteem,7,8 uplift from caregiving,9,10 finding or making meaning through caregiving,11-15 and caregiver appraisal.16 In some studies, assessment of PAC included improved relationships, feeling appreciated, pleasure, and prevention of further deterioration.2,17,18 Depending on their focus, different researchers have designed instruments to evaluate the PAC. However, till recently none of these instruments assessed the various positive aspects comprehensively. Of late, the Scale for Positive Aspects of Caregiving Experience (SPACE)19 was developed to evaluate the various domains of positive caregiving experiences. This scale is based on the review of literature assessing various PAC.
Schizophrenia is an illness leading to considerable emotional, practical, and financial demands on those close to the sufferer. These demands generally persist over prolonged periods, and advice, help and support may not be readily available.20 Thus, caregiving places a great degree of burden and stress on the family and especially the primary caregiver. Caregivers also experience stigma, worry, guilt, shame,21 distress, burnout, mental morbidity, neglect of health of self, and higher risk of mortality.21-25 However, few studies have evaluated the positive impact of caregiving to patients with schizophrenia. Tarricone et al26 studied 2 cohorts of caregivers of patients with psychosis using the Experience of Caregiving Inventory (ECI), and found that the caregivers in both samples valued the good aspects of relationship slightly more than the positive personal experiences in the positive domains of caregiving. In a longitudinal study, Addington et al27 reported that caregivers prized the positive personal experiences more than the good aspects of the relationship during each assessment. In a comparative study,28 it was noted that caregivers of psychosis patients valued the positive personal experiences more than the good aspects of the relationship with their patient, and vice versa for caregivers of patients with anorexia nervosa. Studies from our centre, based on the ECI, have shown that caregivers of patients with schizophrenia valued the good aspects of the relationship more than the positive personal experiences.29,30 Chen and Greenberg31 assessed caregivers of patients with schizophrenia spectrum disorders through telephone interview on the Caregiving Gains Scale developed by Pearlin,32 and found that although the experience of gains was quite prevalent, not all respondents (40%) had positive experiences with all aspects of gains. Almost 70% of the caregivers reported that they had become more sensitive to persons with disabilities. More than 50% reported that caring for their relative helped them greatly in clarifying their priorities in life and engendered a greater sense of inner strength.
There are also studies looking at various correlates of PAC. By using ECI, caregivers who appraise the caregiving experience more negatively also appraised the same more positively.27,33,34 However, some have not reported any relationship between positive and negative caregiving experience as assessed by the ECI.35 Other studies have examined the relationship of PAC with socio- demographic variables of patients and caregivers,31,33,34,36 clinical variables,31,33,34,36-38 level of psychopathology,31,33,37 level of caregiver involvement,39,40 as well as coping and social support.27,29,38,40-43 However, the findings of these studies cannot be generalised as the PAC were not assessed comprehensively in these studies.
India still has a traditional family structure. Social support for persons with schizophrenia comes mainly from the family; support from the government and non- governmental organisations is limited. Thus, it is important to understand the PAC in addition to the burden. To our knowledge, this is the first local study to explore the PAC and its correlates (socio-demographic, clinical variables, level of psychopathology, burden, coping, social support) in primary caregivers of patients with schizophrenia in India.
Methods
Patients with schizophrenia along with their caregivers were selected by purposive random sampling. The former were included for the study if they had a diagnosis of schizophrenia as per the DSM-IV criteria44 (as assessed by MINI45), aged 20 to 60 years, and an illness of 2 to 10 years. Those with co-morbid chronic physical, other psychiatric or substance dependence (except tobacco dependence) disorders and organic brain syndromes were excluded. Patients who had a family member with a diagnosed chronic physical illness or psychiatric disorder staying in the same dwelling unit were also excluded.
In this study, a primary caregiver was defined as a person living with the patient and intimately involved in his or her care for at least 1 year, i.e., looking after his / her daily needs, supervising medications, bringing the patient to the hospital, staying with the patient during inpatient stays and maintaining liaison with hospital staff. To be included in the study, the caregivers were also required to be older than 18 years, free from any diagnosed physical or psychiatric disorder (other than tobacco dependence), and were able to read Hindi and / or English.
The study was approved by the Ethics Review Committee of our institute. Patients and the caregivers were recruited from inpatient or outpatient services after obtaining written informed consent.
Instruments
The Mini-International Neuropsychiatry Interview46 was used to confirm the diagnosis of schizophrenia and rule out co-morbid psychiatric disorders. The psychopathology of the patients was rated according to the Positive and Negative Syndrome Scale (PANSS) for schizophrenia.45
Scale for Positive Aspects of Caregiving Experience
The SPACE25 consists of 44 items assessing various aspects of positive caregiving experience which covers 4 domains, including caregiver gains, motivation for caregiving role, caregiver satisfaction, as well as self-esteem and social aspect of caring. Each item is rated on a 5-point rating scale (0-4). The scale has good internal consistency (Cronbach’s alpha = 0.923), test-retest reliability (intraclass correlation coefficient of 0.81-0.99 for different items), cross-language reliability (intraclass correlation coefficient of 0.47-0.97 for different items), split-half reliability (Guttmann split-half coefficient = 0.834), and face validity (> 90%).25 The mean score of each domain was obtained by dividing the total score of the domain by the number of items included in the domain.
Family Burden Interview Schedule
The Family Burden Interview (FBI) Schedule is a well- established tool developed by Pai and Kapur47 which has been extensively used by Indian researchers. Its reliability and validity are greater than 0.87 and 0.72, respectively.47
Involvement Evaluation Questionnaire
The Involvement Evaluation Questionnaire (IEQ) consists of interconnected domains that represent the possible consequences of caring for a family member with severe mental illness.48,49 It consists of 31 items, each rated on 5-point Likert scale.50 Our previous study50 adapted and translated the IEQ into Hindi and evaluated its psychometric properties. The Hindi version (Hindi-IEQ) has been found to have significant Pearson’s correlation coefficients (p < 0.05) and intraclass correlation coefficients for each item and the subscales, indicating a satisfactory level of agreement between the Hindi and English versions.50 Test-retest reliability (intraclass correlation coefficient of 0.76-1.00) and split-half reliability (Spearman-Brown coefficient of -0.68) of the Hindi-IEQ have been found to be satisfactory. Factor analysis of the scale yielded 4 subscales covering 29 items. These 4 factors were tension (10 items), worrying-urging I (10 items), worrying-urging II (6 items), and supervision (3 items).50
Global Assessment of Functioning Scale
The Global Assessment of Functioning (GAF) Scale51 provides measures of overall functioning relating to psychiatric symptoms. It is a clinician-rated, 100-point scale based on all available information with a clear description of each of the 10-point intervals.
Social Support and Coping
Social support was assessed using the Hindi adaptation52 of Social Support Questionnaire (SSQ) by Pollack and Harris.53 Caregiver coping was assessed using the modified Hindi version54 of the coping checklist of Scazufca and Kuipers.55
World Health Organization Quality of Life–BREF
The World Health Organization (WHO) Quality of Life– BREF is the only QOL instrument designed as a multilingual instrument of which a self-administered Hindi version is available. It places emphasis on subjective evaluation of respondent’s health and living conditions. Four domains of QOL are measured — physical health, psychological health, social relationships, and environment; additionally the scale has a general health domain. The scale has 26 items scored from 1 to 5 with a total score range of 26 to 130. Its psychometric properties are comparable to those of the full version (WHOQOL-100).56 The scale has good discriminant validity, concurrent validity, internal consistency, and test- retest reliability.56
World Health Organization Quality of Life– Spirituality, Religiousness and Personal Beliefs Scale
The WHO Quality of Life–Spirituality, Religiousness and Personal Beliefs Scale (WHOQOL-SRPB)57 is based on the generic WHOQOL-100.56 In the latter, the spirituality domain comprised a facet that addressed issues relating to the meaning of life and personal beliefs. In the WHOQOL-SRPB, there are additional 32 questions related to spirituality, religiousness, and personal beliefs making a total of 8 facets. The instrument has been developed from an extensive pilot test of 105 questions in 18 centres all over the world. Cronbach’s alpha for the SRPB facets was strong, ranging from 0.77 (meaning and purpose in life) to 0.95 (faith). The SRPB domain of the WHOQOL- SRPB (i.e. WHOQOL-100 with SRPB) was translated into Hindi according to the WHO translation methodology and was shown to have good reliability.58 In the present study, only these 32 translated questions pertaining to spirituality, religiousness, and personal beliefs were used.
General Health Questionnaire
A Hindi-translated version59 of the General Health Questionnaire (GHQ-12)60 was used to assess psychological morbidity. A score of < 2 indicates that the subject is free from any psychiatric illness.61
Procedure
Patients with a diagnosis of schizophrenia, attending the outpatient services with a caregiver or admitted to the inpatient unit, were approached. They were asked to participate in the investigation after explaining the nature of the study, and those meeting the inclusion and exclusion criteria were recruited by purposive random sampling. The patients were assessed using the PANSS and GAF, whereas the caregivers were assessed using the FBI Schedule. The latter were then requested to complete the scales for the SPACE, Hindi-IEQ, coping checklist, SSQ, WHOQOL- BREF, WHOQOL-SRPB, and GHQ-12. Caregivers who scored a GHQ-12 score of ≥ 2 were advised to seek a formal psychiatry consultation.
Statistical Analysis
Data were analysed using the Statistical Package for the Social Sciences (SPSS 14; Chicago [IL], US). Descriptive analysis was carried out using mean and standard deviation (SD) with range for continuous variables, including socio-demographics, clinical features, and scores for the PANSS, FBI Schedule, SSQ, coping checklist, Hindi IEQ, WHOQOL-BREF, WHOQOL-SRPB, and GHQ-12. Descriptive analyses were computed in terms of frequencies and percentages pertaining to discontinuous socio- demographic and clinical variables. Pearson’s product moment correlation was used to assess the association between the PAC and continuous variables. Spearman’s rank correlation was used to assess the association between the PAC and discontinuous variables.
Results
For this study, initially 239 patients and their caregivers were approached by convenience sampling, 2 of whom refused to participate. The other 17 patients and caregiver pairs were excluded because they were unable to read Hindi and / or English. Another 15 pairs were also excluded because of the duration of illness over 10 years, and 5 patients had other psychiatric co-morbidity. This resulted in a sample of 200 patients and caregivers. From this sample, 100 were selected based on the randomisation table generated using the SPSS prior to any analysis.
Socio-demographic Profile
The mean (SD) age of the patients was 31 (10) years (range, 18-58 years); 56 were males and 57 were unmarried. There was nearly an equal distribution of patients from nuclear (n = 49) and non-nuclear families (n = 51), as well as urban (n = 53) and rural (n = 47) localities. Majority of the patients were Hindu (n = 85) and not on any paid employment (n = 80). The mean (SD) duration of education of these patients was 13 (4) years (range, 6-22 years). The mean (SD) monthly income of their families was 15,840 (11,420) Indian Rupees (range, 3,000-70,000 Indian Rupees).
The mean (SD) age of the caregivers was 46 (12) years (range, 24-71 years) with a male predominance (65%). Most of them (90%) were married. Their mean (SD) duration of education was 15 (3) years (range, 6-22 years). Nearly three quarters (n = 73) of these caregivers were employed, about half were parents (51%), while 22% were spouses and 20% were siblings. As primary caregivers, they had been performing that role for a mean of 5 (range, 1-10) years, and a mean of 3 hours daily in providing care to the patient. Caregivers accompanied their patients during 93% of the follow-up visits in the previous 3 months, and 73% supervising their patient’s medications.
Clinical Profile of the Patients
Half of the patients were diagnosed with paranoid schizophrenia (n = 50). In the non-paranoid group, the commonest subtype was undifferentiated schizophrenia (n = 41) followed by catatonic schizophrenia (n = 6), hebephrenic schizophrenia (n = 2), and the remaining diagnosed with residual schizophrenia. The mean (SD) age of onset of their illness was 25 (9) years (range, 13-53 years), with a mean (SD) duration of 6 (3) years (range, 2-10 years). They had a mean (SD) of 2 (2) hospital visits 3 months prior to recruitment into the study (range, 1-9 visits). The mean (SD) PANSS positive symptom score was 13 (5), the mean (SD) negative symptom score was 14 (5), and the mean (SD) general psychopathology score was 27 (6). The mean (SD) total PANSS score was 54 (13), indicating that the sample was moderately ill at the time of assessment. On the GAF scale, the mean (SD) score was 52 (15).
Positive Aspects of Caregiving
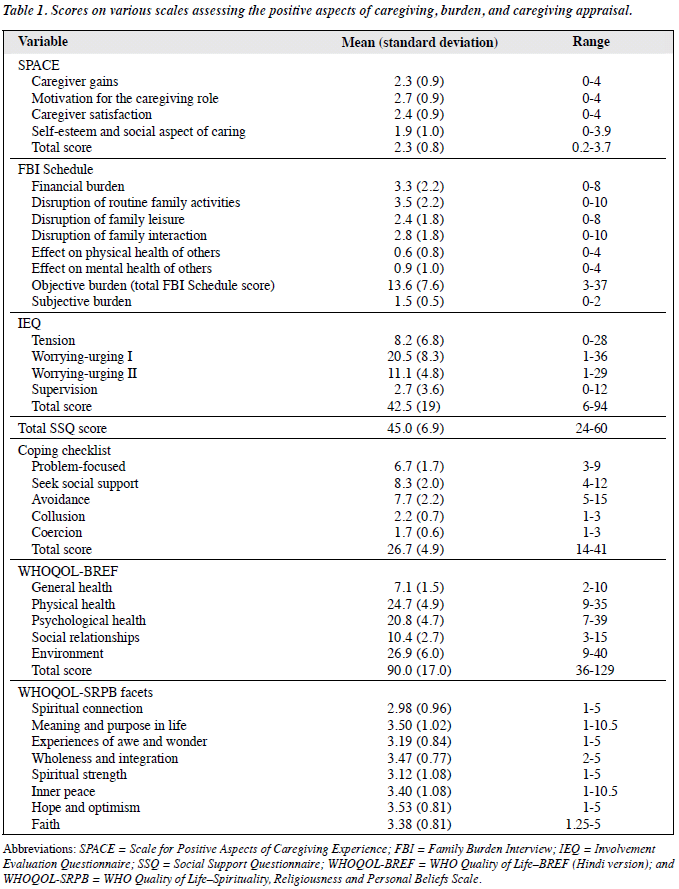
As assessed by the SPACE shown in Table 1, the highest score was seen in the domain of motivation for the caregiving role, followed by that of caregiver satisfaction and caregiver gains. The mean score was least for the domain of self- esteem and social aspect of caring.
Burden, Caregiving Consequence, Coping, and Social Support
In Table 1, on FBI Schedule the maximum burden was perceived in the domain of disruption of routine family activities. In terms of severity of burden, 2 caregivers reported no burden (rated as 0), 47 reported a moderate level of burden (rated as 1), and 51 reported a severe subjective burden (rated as 2). The mean (SD) clinician rating for global objective burden was 1.3 (0.5) [range, 0-2]. In terms of severity, clinicians rated no burden in 2 cases, moderate burden for two-thirds of the sample (n = 66) and a severe burden in 32. Regarding the IEQ, mean scores were highest for the worrying-urging I domain followed by the worrying- urging II domain. The mean total SSQ score was 45 (range, 24-60), indicating a moderate level of social support. With regard to coping, the mean score on seeking social support was 8.3 (range, 4-12), use of collusion had a mean score of 2.2 (range, 1-3), whereas coercion as a coping strategy had a mean score of 1.7 (range, 1-3).
Quality of Life
The mean scores on various WHOQOL-BREF domains are shown in Table 1. The mean (SD) total WHOQOL score was 90.0 (17.0) [range, 36-129]. On WHOQOL-SRPB scale, highest scores were obtained in the domain of hope and optimism, closely followed by that of meaning and purpose in life, as well as wholeness and integration. Least score was obtained in the domain of spiritual connection.
Psychological Morbidity in Caregivers
Of these 100 caregivers, about one-third (36%) had a GHQ-12 score of ≥ 2, the mean (SD) score being 3.7 (2.6) [range, 2-10] indicating a fair level of morbidity.
Correlates of Positive Aspects of Caregiving
There were no significant correlations between the SPACE and socio-demographic variables of both the patients and caregivers. Also, no significant correlation emerged between the SPACE and other variables of caregiving, such as relationship with patient, time spent in caregiving per day, duration since in caregiver role, percentage of visits with the caregivers, and supervision of medications.
With regard to clinical variables, there were also no significant correlates emerged except for a positive correlation between the motivation for the caregiving domain and PANSS negative symptom scale (Pearson product moment correlation = 0.224, p = 0.03).
No correlations emerged between the SPACE and IEQ domains, except for a positive correlation between the self-esteem and social aspect of caring domain of SPACE and the worrying-urging II domain (Pearson product moment correlation = 0.254, p = 0.01) and the total IEQ score (0.236, p = 0.02).
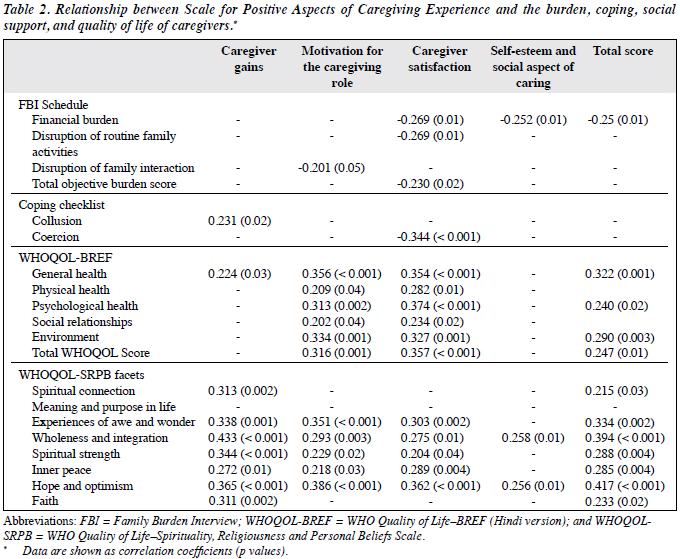
As shown in Table 2, a significant negative correlation was noted between motivation for the caregiving role and disruption of family interaction. Financial burden also had negative correlations with the caregiver satisfaction, self- esteem and social aspect of caring, and total SPACE score. Caregiver satisfaction also had a negative correlation with disruption of routine family activities and the total objective burden score.
There was no relationship between social support and the SPACE. With regard to coping, use of coercion as a coping strategy led to poor caregiver satisfaction as noted by their negative correlation. Use of collusion as a coping strategy was associated with more caregiver gains as reflected by their positive correlation (Table 2).
Motivation for the caregiving role and caregiver satisfaction correlated positively with all the WHOQOL- BREF domains and its total score. Similarly, the total SPACE scores correlated with the domains of general health, psychological health, environment, and the total WHOQOL-BREF score. A positive correlation between caregiver gains and the WHOQOL-BREF general health score was also noted.
The caregiver gains and total SPACE score correlated positively with all the WHOQOL-SRPB facets, except for the meaning and purpose of life. Motivation for the caregiving role and caregiver satisfaction also correlated positively with 5 of the WHOQOL-SRPB domains (Table 2). Self-esteem and the social aspect of caregiving correlated positively with the WHOQOL-SRPB facets of wholeness and integration as well as hope and optimism.
Relationship between the Positive Aspects of Caregiving and Psychological Morbidity
No correlations emerged between the total GHQ-12 score and the SPACE. When the scores on various domains and total SPACE score were also compared in those who were GHQ-12 positive and GHQ-12 negative using the t test, no significant difference emerged between the 2 groups.
Discussion
Positive Aspects of Caregiving
As there are no previous studies using this scale, findings of the present study cannot be compared with the existing literature. However, some important facts emerge. Caregivers had a highest score for motivation for the caregiving role, followed by their satisfaction and gains, whereas the mean score was least for the self-esteem and social aspect of caring.
The present study shows that motivation for the caregiving is the most important aspect of taking up that role. This domain included statements like “You have felt good about yourself”; “You have contributed to your ill relative’s wellbeing”; “You have felt reassured knowing that as long as you are helping your ill relative, [he / she] is getting proper care”, etc., suggesting that personality factors or intrinsic factors play an important motivating factor in taking up and continuing as a caregiver.
Caregiver satisfaction is understood as “the benefits accruing to the caregiver through his or her own efforts”16 or as “subjectively perceived gains from desirable aspects of or positive affective returns from caregiving”5 or as “the result of caregiving experiences that give life a positive flavor”.62 Caregiver gains are understood as “the extent to which the caregiving role is appraised to enhance an individual’s life space and be enriching”18 or as “the caregiver’s perceived personal growth and enhanced interpersonal relationships”.31 Caregiver esteem is understood as the extent to which performing caregiving enhances the caregiver’s self-esteem or simply as the confidence one has for oneself.62 On the SPACE, the caregiver self-esteem and social aspect of caring are clubbed under one heading. Taking this into consideration, it can be hypothesised that most people possibly take up the caregiving role because of the feelings for their ill relatives and social reasons, which may also include social obligation. This caregiver role is not only approved by the society in general, but also appreciated by the treating team and at the same time makes the caregiver feel worthy and resultantly boost their self-esteem. This increased self-esteem also helps in identifying the caregiver’s personal gains and satisfaction. All these taken together contribute to long-term motivation to continue as a caregiver.
Association of Positive Aspects of Caregiving with Socio-demographics
There is no consensus in the literature with respect to the association between PAC and socio-demographic profile of patients and caregivers. Some studies reported no significant relationship between the caregiving appraisals and age, gender, and employment of the caregiver.31 Findings of the current study are similar. However, they are not in concordance with studies revealing that caregivers who are more educated reported higher levels of positive personal experiences, perception of good aspects of relationship,31 as well as overall positive caregiving experience.31,34 Other studies suggest that more positive caregiving experiences have been noted when the patients are females,2,36 and caregivers of patients who were young33 and unemployed31,33,34 reported less positive experiences. Lack of such associations in the present study suggests that positive caregiving experience is not affected much by the socio-demographics.
Association of Positive Aspects of Caregiving with Clinical Variables
No significant correlations were found between various clinical variables including residual psychopathology and the level of functioning, except a negative correlation between the PANSS negative symptom subscale and SPACE domain of motivation for the caregiving role. Findings of the present study are similar to those reported by others, showing that higher avolition-apathy score on the Scale for the Assessment of Negative Symptoms was associated with lower positive appraisals.31 As the patient and caregiver profiles of the present study suggest that patients were ill for a reasonable period of time, and that caregivers were in such role for prolonged periods, the association between negative symptoms and motivation for caregiving is understandable. This association suggests that persistence of negative symptoms, despite best efforts of the caregivers, leads to a feeling of failure and hence possibly reduces the motivation to care.
One study reported that the caregivers of patients with higher positive symptoms of schizophrenia reported more positive caregiving experience.36 Other studies showed no relationship between relatives’ appraisal of caregiving and symptomatology.33,37 In the present study, lack of an association between PAC and positive symptoms and general psychopathology scores could be due to lower overall mean scores and less severe psychopathology in these domains.
Association of Positive Aspects of Caregiving with Perceived Burden
Few correlations emerged between the SPACE and the burden as assessed by the FBI Schedule. All these were negative correlations, which suggest that an increase in burden in various aspects of life of caregivers leads to reduction in PAC in different domains. Among these, higher financial burden leads to lower PAC in the caregiver satisfaction, self-esteem and social aspect of caring, and overall positive caregiving experience. Further, more disruption in routine family activities and higher objective burden were associated with lower caregiver satisfaction. Some of these correlations are understood in the socio- economic background of patients and caregivers and the services available. Studies from our centre suggest about 95% of the total health care cost of schizophrenia borne by the patient and the family, and they spent about half of their income in taking care of treatment needs by the patients.63 In such a scenario, if the symptoms of patients lead to higher disruption in the family’s day-to-day activities and disruption in financial resources (both in the form of higher expenditure and lower income, because the caregiver has to supervise the patient for longer hours), then it is natural that it leads to lesser caregiver satisfaction and overall positive caregiving experience.
Earlier studies on the relationship between positive and negative aspects of caregiving reported that family caregivers with a more positive interpretation of family caregiving or their relationship with the patient reported lower levels of family caregiver burden.2,64 Our findings also support the same, in that there was an inverse relationship between burden and some aspects of positive caregiving.
Studies of assessing caregiving experience using ECI suggest that caregivers who appraise their experience more negatively also appraised the same more positively.27,33,34 However, our findings do not support this assertion. The lack of concordance between findings of the present study and the literature is possibly due to the type of assessment instrument used. The burden instrument used in the present study is more overloaded towards assessment of objective and lays much less emphasis on subjective burdens, which is more of a caregiving appraisal, whereas the ECI assesses the negative caregiving experience as appraisal, which is a more of subjective caregiving experience rather than the objective burden of caregiving.
Association of Positive Aspects of Caregiving with Involvement Evaluation Questionnaire
The IEQ assessed caregiving experience in the cognitive appraisal context, as it taps more into subjective negative caregiving experience. Most of the association between the IEQ and PAC were positive correlations, suggesting that an increase in positive experience of caregiving was also associated with higher negative caregiving appraisal, which provide credence to findings of studies that have used ECI and have reported that caregivers who appraise the caregiving experience more negatively also appraised the same more positively.27,33,34
Association of Positive Aspects of Caregiving with Coping
In the present study, use of collusion (i.e. agreed / gave in / did not force when patient did things I disliked) as a coping strategy was associated with more caregiver gains. An interesting association was also noted in the present study, in the form of a negative correlation between coercion as a coping strategy and caregiver satisfaction as a positive experience. These findings possibly reflect that an ability to mould oneself and not forcing oneself (one’s opinion) on the patient is associated with more positive caregiver gains. These associations can have important clinical implications and advising the caregivers to use more collusion and less coercion which may result in a better caregiving experience.
Earlier studies suggest that using problem-focused coping strategies and seeking social support as a coping strategy are associated with higher levels of positive personal caregiving experiences.35 However, findings of the present study do not support this.
Association of Positive Aspects of Caregiving with Social Support
There were no associations between social support and any of the SPACE domains. This finding contradicts some reports which have concluded that social support plays an important role in the PAC. The latter noted significant positive associations between the experience of caregiving benefits / gains and family socio-emotional support29 and support received from the patients themselves.43 This difference in the findings could be due to the fact that in the present study, the instrument was used to evaluate social support available to the caregiver in general rather than that from other family members or the patient per se.
Association of Positive Aspects of Caregiving with Quality of Life
In the present study, there were multiple correlations between the SPACE and QOL. All these positive correlations suggest that a higher positive caregiving experience is associated with better QOL of caregivers, and suggests that enhancing such positive caregiving experience can contribute to better QOL. Earlier studies which have evaluated spirituality, religiousness, and personal beliefs of caregivers have done the same in the form of assessments of religious coping strategies, intrinsic and organisational religiosity, or as a positive caregiving experience per se in the form of a subscale (the ultimate meaning subscale) of the Finding Meaning Through Caregiving Scale.13 One study suggests that religious coping strategies frame the caregiving experience in a positive manner.41 The findings of our study were similar. Another study reported that religiosity was associated with better self-esteem and self-care and less of depression among the family caregivers.65 Although in the present study, WHOQOL-SRPB did not assess religiosity and spirituality from the practice or coping point of view, it still suggests a reciprocal positive association between SRPB and PAC.
To further understand the relationship of PAC and WHOQOL-SRPB, it is important to understand the conceptual foundation of WHOQOL-SRPB. The WHOQOL-SRPB was constructed to assess how spirituality, religion, and personal beliefs relate to QOL in health and health care. It is understood that SRPB was added to the WHOQOL-100, because many people from the communities participating in the WHOQOL survey reported spirituality, religiousness, and personal beliefs as core aspects of their QOL. Furthermore, the items included in WHOQOL-SRPB were elicited and recommended by focus groups as being concerned with aspects of SRPB that are integrated with their QOL.66 From this perspective, the WHOQOL-SRPB taps the outcome of a patient’s illness on caregivers. It can therefore be said that those caregivers who appraise caregiving more positively have a better QOL in the WHOQOL-SRPB domains.
Association of Positive Aspects of Caregiving with Psychological Morbidity
Although some of the previous studies on ECI reported a positive association between negative caregiving appraisal and psychological morbidity in caregivers,33,35 no association between positive caregiving appraisal and psychological morbidity in the same group was noted. Similarly, no association was seen between psychological morbidity (as assessed on GHQ-12) and positive caregiving experience in the present study, which supports the literature on the lack of any such relationship.29
Limitations and Future Directions
One limitation of this study was that it included mostly outpatients attending a general hospital psychiatry unit. Therefore, the results cannot be generalised to other patient populations. Second, the sample size was small and cross- sectional evaluation of the caregivers was lacking. Third, the duration of illness was restricted to 2 to 10 years and patients with physical illness and other psychiatric morbidity were excluded. Replication of the study on a larger sample drawn from different settings is therefore needed. Furthermore, longitudinal studies are required to study the changes in the caregiving experience over time and the impact of various types of interventions.
Declaration
The authors declared no conflict of interest in this manuscript.
References
- Addington J, McCleery A, Addington D. Three-year outcome of family work in an early psychosis program. Schizophr Res 2005;79:107-16.
- Pickett SA, Cook JA, Cohler BJ, Solomon ML. Positive parent / adult child relationships: impact of severe mental illness and caregiving burden. Am J Orthopsychiatry 1997;67:220-30.
- Szmukler GI, Burgess P, Herrman H, Benson A, Colusa S, Bloch S. Caring for relatives with serious mental illness: the development of the Experience of Caregiving Inventory. Soc Psychiatry Psychiatr Epidemiol 1996;31:137-48.
- Nolan M, Grant G, Keady J. Understanding family care: a multi- dimensional model of caring and coping. Buckingham & Philadelphia: Open University Press; 1996.
- Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two- factor model of caregiving appraisal and psychological well-being. J Gerontol 1991;46:181-9.
- Cohen CA, Colantonio A, Vernich L. Positive aspects of caregiving: rounding out the caregiver experience. Int J Geriatr Psychiatry 2002;17:184-8.
- Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health 1992;15:271-83.
- Nijboer C, Tempelaar R, Triemstra M, van den Bos GA, Sanderman R. The role of social and psychologic resources in caregiving of cancer patients. Cancer 2001;91:1029-39.
- Kinney JM, Stephens MA, Franks MM, Norris VK. Stresses and satisfactions of family and caregivers to older stroke patients. J Appl Geron 1995;14:3-21.
- Wallsten SM, Snyder S. A comparison of elderly family caregivers’ and noncaregivers’ perception of stress in daily experiences. J Comm Psychol 1990;18:228-38.
- Ayres L. Narratives of family caregiving: the process of making meaning. Res Nurs Health 2000;23:424-34.
- Farran CJ. Theoretical perspectives concerning positive aspects of caring for elderly persons with dementia: stress / adaptation and existentialism. Gerontologist 1997;37:250-7.
- Farran CJ, Miller BH, Kaufman JE, Donner E, Fogg L. Finding meaning through caregiving: development of an instrument for family caregivers of persons with Alzheimer’s disease. J Clin Psychol 1999;55:1107-25.
- Farran CJ, Miller BH, Kaufman JE, Davis L. Race, finding meaning, and caregiver distress. J Aging Health 1997;9:316-33.
- Folkman S. Positive psychological states and coping with severe stress. Soc Sci Med 1997;45:1207-21.
- Lawton MP, Kleban MH, Moss M, Rovine M, Glicksman A. Measuring caregiving appraisal. J Gerontol 1989;44:61-71.
- Kramer BJ. Gain in the caregiving experience: Where are we? What next? Gerontologist 1997;37:218-32.
- Carbonneau H, Caron C, Desrosiers J. Development of a conceptual framework of positive aspects of caregiving in dementia. Dementia 2010;9:327-53.
- Kate N, Grover S, Kulhara P, Nehra R. Scale for positive aspects of caregiving experience: development, reliability, and factor structure. East Asian Arch Psychiatry 2012;22:62-9.
- Chakrabarti S. Impact of schizophrenia on caregivers: the Indian perspective. In: Kulhara P, Avasthi A, Grover S. Schizophrenia: The Indian scene. 2nd ed. Barwala, Haryana: PsyPROM, PGIMER, Chandika Press; 2010: 215-62.
- Tennakoon L, Fannon D, Doku V, O’Ceallaigh S, Soni W, Santamaria M, et al. Experience of caregiving: relatives of people experiencing a first episode of psychosis. Br J Psychiatry 2000;177:529-33.
- Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA 1999;282:2215-9.
- Harvey K, Burns T, Fiander M, Huxley P, Manley C, Fahy T. The effect of intensive case management on the relatives of patients with severe mental illness. Psychiatr Serv 2002;53:1580-5.
- Angermeyer MC, Kilian R, Wilms HU, Wittmund B. Quality of life of spouses of mentally ill people. Int J Soc Psychiatry 2006;52:278-85.
- Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. Pharmacoeconomics 2008;26:149-62.
- Tarricone I, Leese M, Szmukler GI, Bassi M, Berardi D. The experience of carers of patients with severe mental illness: a comparison between London and Bologna. Eur Psychiatry 2006;21:93-101.
- Addington J, Coldham EL, Jones B, Ko T, Addington D. The first episode of psychosis: the experience of relatives. Acta Psychiatr Scand 2003;108:285-9.
- Treasure J, Murphy T, Szmukler G, Todd G, Gavan K, Joyce J. The experience of caregiving for severe mental illness: a comparison between anorexia nervosa and psychosis. Soc Psychiatry Psychiatr Epidemiol 2001;36:343-7.
- Aggarwal M, Avasthi A, Kumar S, Grover S. Experience of caregiving in schizophrenia: a study from India. Int J Soc Psychiatry 2011;57:224- 36.
- Grover S, Chakrabarti S, Aggarwal M, Avasthi A, Kulhara P, Sharma S, et al. Comparative study of the experience of caregiving in bipolar affective disorder and schizophrenia. Int J Soc Psychiatry 2012;58:614- 22.
- Chen FP, Greenberg JS. A positive aspect of caregiving: the influence of social support on caregiving gains for family members of relatives with schizophrenia. Community Ment Health J 2004;40:423-35.
- Pearlin LI. Caregiver’s stress and coping study (NIMHR01MH42122). San Francisco, CA: University of California, Human Development and Aging Programs; 1988.
- Harvey K, Burns T, Fahy T, Manley C, Tattan T. Relatives of patients with severe psychotic illness: factors that influence appraisal of caregiving and psychological distress. Soc Psychiatry Psychiatr Epidemiol 2001;36:456-61.
- Lau DY, Pang AH. Caregiving experience for Chinese caregivers of persons suffering from severe mental disorders. Hong Kong J Psychiatry 2007;17:75-80.
- Martens L, Addington J. The psychological well-being of family members of individuals with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 2001;36:128-33.
- Mo FY, Chung WS, Wong SW, Chun DY, Wong KS, Chan SS. Experience of caregiving in caregivers of patients with first-episode psychosis. Hong Kong J Psychiatry 2008;18:101-6.
- Tang VW, Leung SK, Lam LC. Clinical correlates of the caregiving experience for Chinese caregivers of patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 2008;43:720-6.
- Onwumere J, Kuipers E, Bebbington P, Dunn G, Fowler D, Freeman D, et al. Caregiving and illness beliefs in the course of psychotic illness. Can J Psychiatry 2008;53:460-8.
- López J, López-Arrieta J, Crespo M. Factors associated with the positive impact of caring for elderly and dependent relatives. Arch Gerontol Geriatr 2005;41:81-94.
- Aschbrenner KA, Greenberg JS, Allen SM, Seltzer MM. Subjective burden and personal gains among older parents of adults with serious mental illness. Psychiatr Serv 2010;61:605-11.
- Rammohan A, Rao K, Subbakrishna DK. Religious coping and psychological wellbeing in carers of relatives with schizophrenia. Acta Psychiatr Scand 2002;105:356-62.
- Herrera AP, Lee JW, Nanyonjo RD, Laufman LE, Torres-Vigil I. Religious coping and caregiver well-being in Mexican-American families. Aging Ment Health 2009;13:84-91.
- Horwitz AV, Reinhard SC, Howell-White S. Caregiving as reciprocal exchange in families with seriously mentally ill members. J Health Soc Behav 1996;37:149-62.
- Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision (DSM-IV). Washington DC., American Psychiatric Association; 1994.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22-33.
- Pai S, Kapur RL. The burden on the family of a psychiatric patient: development of an interview schedule. Br J Psychiatry 1981;138:332- 5.
- Schene AH, van Wijngaarden B, Koeter MW. Family caregiving in schizophrenia: domains and distress. Schizophr Bull 1998;24:609-18.
- van Wijngaarden B, Schene AH, Koeter M, Vázquez-Barquero JL, Knudsen HC, Lasalvia A, et al. Caregiving in schizophrenia: development, internal consistency and reliability of the Involvement Evaluation Questionnaire — European Version. EPSILON Study 4. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl 2000;39:s21-7.
- Grover S, Chakrabarti S, Ghormode D, Dutt A, Kate N, Kulhara P. An Indian adaptation of the Involvement Evaluation Questionnaire: similarities and differences in assessment of caregiver burden. East Asian Arch Psychiatry 2011;21:142-51.
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976;33:766-71.
- Nehra R, Kulhara P, Verma SK. Adaptation of Social Support Questionnaire in Hindi: Indian setting. Ind J Clin Psychol 1996;23:33- 9.
- Pollack L, Harris R. Measurement of social support. Psychol Rep 1983;53:446-9.
- Nehra R, Chakrabarti S, Sharma R, Kaur R. Psychometric properties of the Hindi version of the coping checklist of Scazufca and Kuipers. Ind J Clin Psychol 2002;29:79-84.
- Scazufca M, Kuipers E. Coping strategies in relatives of people with schizophrenia before and after psychiatric admission. Br J Psychiatry 1999;174:154-8.
- Saxena S, Chandiramani K, Bhargava R. WHOQOL-Hindi: a questionnaire for assessing quality of life in health care settings in India. World Health Organization Quality of Life. Natl Med J India 1998;11:160-5.
- WHOQOL SRPB Group. A cross-cultural study of spirituality, religion, and personal beliefs as components of quality of life. Soc Sci Med 2006;62:1486-97.
- Shah R, Kulhara P, Grover S, Kumar S, Malhotra R, Tyagi S. Relationship between spirituality / religiousness and coping in patients with residual schizophrenia. Qual Life Res 2011;20:1053-60.
- Gautam S, Nijhawan M, Kamal P. Standardisation of hindi version of goldbergs general health questionnaire. Indian J Psychiatry 1987;29:63-6.
- Goldberg D. Detection of psychiatric illness by questionnaire (Maudsley Monograph). Oxford: Oxford University Press; 1972.
- Cano A, Sprafkin RP, Scaturo DJ, Lantinga LJ, Fiese BH, Brand F. Mental health screening care: a comparison of 3 brief measures of psychological distress. Prim Care Companion J Clin Psychiatry 2001;3:206-10.
- Lawton MP, Rajagopal D, Brody E, Kleban MH. The dynamics of caregiving for a demented elder among black and white families. J Gerontol 1992;47:S156-64.
- Grover S, Avasthi A, Chakrabarti S, Bhansali A, Kulhara P. Cost of care of schizophrenia: a study of Indian out-patient attenders. Acta Psychiatr Scand 2005;112:54-63.
- Hsiao CY, Van Riper M. Individual and family adaptation in Taiwanese families of individuals with severe and persistent mental illness (SPMI). Res Nurs Health 2009;32:307-20.
- Murray-Swank AB, Lucksted A, Medoff DR, Yang Y, Wohlheiter K, Dixon LB. Religiosity, psychosocial adjustment, and subjective burden of persons who care for those with mental illness. Psychiatr Serv 2006;57:361-5.
- Fleck MP, Skevington S. Explaining the meaning of the WHOQOL- SRPB. Rev psiquiatr clín [serial on the Internet]. http://dx.doi.org/10.1590/S0101-60832007000700018.