East Asian Arch Psychiatry 2013;23:65-70
ORIGINAL ARTICLE
Ms Shivani Santosh, MPhil, Psychology Research Unit, Indian Statistical Institute, Kolkata, India.
Dr Debdulal Dutta Roy, PhD, Psychology Research Unit, Indian Statistical Institute, Kolkata, India.
Dr Partha Sarathi Kundu, MD, DNB, West Bengal Heath Services, Kolkata, India.
Address for correspondence: Ms Shivani Santosh, Psychology Research Unit, Indian Statistical Institute, 203 B. T. Road, Kolkata 700108, West Bengal, India. Tel: (91) 9874550333; Email: shivanipsy@gmail.com
Submitted: 19 March 2013; Accepted: 16 May 2013
Abstract
Objectives: To explore the relationship between cognitive functions, social functioning, and psychopathology in schizophrenia.
Methods: Patients diagnosed with schizophrenia, according to the ICD-10 criteria, were enrolled from the Department of Psychiatry of 2 postgraduate hospitals in Kolkata, India. The Positive and Negative Syndrome Scale for Schizophrenia, Schizophrenia Research Foundation India–Social Functioning Index, and a cognitive test battery were administered.
Results: Regarding the 100 patients recruited into the study, 4 subtests (self-care, occupational role, social role, and family role) of the social functioning were found to be significantly correlated with cognitive functions. Cognitive function battery performance scores were more inversely correlated with negative symptoms than with positive symptoms.
Conclusion: Positive and negative symptoms along with verbal fluency were able to predict social functioning.
Key words: Cognition; Schizophrenia; Social behavior
摘要
目的:检视精神分裂症患者的认知功能、社会功能与精神病理学间的关係。
方法:研究对象为印度加尔各答研究生医院精神病学部门,经ICD-10确诊的精神分裂症患者,并使用精神分裂症阳性及阴性症状量表、印度精神分裂症研究基金会社会功能指数,以及认知 测试进行分析。
结果:共纳入100名患者。4个社会功能的子测验结果(自我照顾、职业角色、社会角色和家庭角色)均显示与认知功能显著相关。认知测试分数与阴性症状的负相关较与阳性症状明显。
结论:言语流畅度以及阳性和阴性症状均有助预测患者的社会功能状态。
关键词:认知、精神分裂症、社会行为
Introduction
Schizophrenia is a severe mental disorder characterised by a variety of signs and symptoms. The clinical phenomena associated with schizophrenia can be grouped into positive and negative clusters.1 The positive cluster includes phenomena that are not present in a healthy individual such as hallucinations, delusions, and disorganised speech. The negative cluster describes the absence of certain functions that are present in healthy individuals such as apathy, avolition, and poverty of speech. The ability to attend to things in a selective and focused way, to concentrate over a period of time, to learn new information and skills, to plan, to determine strategies for actions and to execute them, to comprehend language and to use verbal skills for communication and self-expression, and to retain information and manipulate it to solve complex problems are examples of mental processes that are referred to as cognitive function.2
Cognitive functions enable humans to perform in everyday life in the spheres of personal, social, and occupational activities.3 In other words, cognitive function is the intellectual process by which one becomes aware of, perceives, or comprehends ideas. Cognitive function involves all aspects of perception, thinking, reasoning, and remembering. While almost all of these aspects are taken for granted by most people, they become impaired in schizophrenia. Approximately 85% of schizophrenic patients have severe cognitive impairment. On average, schizophrenia patients’ performance deficits in different domains of cognitive function are 1.5 to 2.0 standard deviations (SDs) below those of the healthy population. These impairments also affect patients’ social functioning.4
Social functioning can be defined as a person’s ability to work, to engage in social relationship, to attend to self- care, and to participate in recreational and community activities. Since the earliest descriptions of schizophrenia, impairments in social functioning contributing to poor quality of life were noted to be the rule rather than the exception.5,6
By definition, social impairments characterise schizophrenia, given that current diagnostic criteria require a disturbance or deficit in one or more major areas of functioning such as work, interpersonal relationships, or self-care.7 Social dysfunction is a hallmark characteristic of schizophrenia that has important implications for the development, course, and outcome of this illness.8 Impaired social functioning often worsens the course of the disease and contributes to relapse.9
Impairments in both cognitive and social functions are well documented in the literature,10,11 and there is growing evidence that these 2 functions are correlated.12-15 However, there is no consensus as to which aspect of cognition is most closely related with social functioning. The effectiveness of cognitive remediation to improve social functioning will be enhanced if cognitive functions responsible for mediation of these functions are identified and targeted for cognitive remediation. To date, little is known about which cognitive deficits compromise social functioning in patients with schizophrenia, and it is not clear which cognitive function should be targeted for rehabilitation.16 The study therefore aimed to examine the relationship between psychopathology, cognitive functions, and social functioning in patients with schizophrenia.
Methods
Participants
Patients diagnosed with schizophrenia, according to the ICD-10 criteria, were enrolled from the Department of Psychiatry of 2 postgraduate hospitals in Kolkata, West Bengal, India. All participants provided written informed consent before taking part in this study. At the time of the study, none of the participants had any active psychopathology and all were taken from outpatient department (OPD) of the hospitals. Other inclusion criteria were age between 18 and 50 years and completed at least 7 years of full-time education (i.e. primary education). Exclusion criteria included any co-morbid psychiatric disorder, neurological disorder or significant medical condition; mental retardation or substance dependence except for nicotine and caffeine; and electroconvulsive therapy in the previous 6 months.
Socio-demographic characteristics of the sample were collected through specially designed socio-demographic data sheet. Their mean (± SD) age was 32 ± 8 years, with a mean duration of illness of 3.0 ± 1.4 years. In all, 74% were men; 67%, 28%, and 5% of them had 7 to 11 years, 12 to 14 years, and 15 to 17 years of full-time education, respectively. Besides, 45% were in paid employment; 55% of patients had paranoid schizophrenia while the other 45% were diagnosed undifferentiated schizophrenia. Also, 31% of patients had a family history of mental disorder. In all, 12% presented with abrupt-onset, 47% acute-onset, and 41% insidious-onset schizophrenia.
Procedure
The present study was conducted at government-sponsored hospitals of Kolkata, a metropolitan city in east India. Hospitals with a psychiatric department were asked for permission to collect data from their OPD patients. Once diagnosed by the psychiatrists, the patients were then contacted for informed consent. Of 170 diagnosed patients, 100 gave the informed consent. After initial introduction, the following instruments were administered to all enrolled patients.
Instruments
Socio-demographic and Clinical Data Sheet
A semi-structured checklist was used to record the patients’ socio-demographic details, along with clinical variables such as diagnosis, duration of illness, age at onset, mode of onset, their relevant history of psychiatric illness, and the family history.
Schizophrenia Research Foundation India–Social Functioning Index
The Schizophrenia Research Foundation India–Social Functioning Index (SCARF-SFI)17 is an interview-based scale intended for administration on people with psychiatric illnesses, and the items are rated on a 5-point scale, with a higher score indicating better social functioning. Social functioning is measured over 4 domains of self-care (4 items), occupational role (4 items), family role (4 items), and social role (5 items), so the maximum score is 85. Information was obtained from the subject and / or informant, and a Global Assessment of Social Functioning score was computed and categorised into mild (> 60), moderate (30-60), and severe (< 30).
Positive and Negative Syndrome Scale for Schizophrenia
The Positive and Negative Syndrome Scale (PANSS) for Schizophrenia18 is a 30-item scale (7 items each for positive and negative symptoms and 16 for general psychopathology) with 7-point rating categories ranging from absent (1) to extreme (7). The scale was used to assess the severity of positive and negative symptoms and general psychopathology. A higher score represents greater severity. The PANSS was specifically developed to assess individuals with schizophrenia and is widely used in research settings.
Cognitive Function Battery
The following cognitive function tests were adopted in this study. The Trail Making Test (TMT)19 measures psychomotor speed, visual search, sustained attention, and cognitive shifting. Originally, it was part of the Army Individual Test Battery19 and subsequently was incorporated into the Halstead-Reitan Battery.20 The TMT consists of 2 parts: TMT-A requires an individual to draw lines sequentially connecting 25 encircled numbers distributed on a sheet of paper; task requirements are similar for TMT-B except that the person was required to recite the numbers and letters, alternating between numbers and letters (e.g. 1-A, 2-B, 3-C, etc.). The score on each part represents the time required to complete the task.
The Stroop Test places demands on cognitive flexibility by requiring shifting of perceptual set in accordance with changing demands, as well as inhibition of an over-learned or habitual response in favour of a novel response. The Victorian version by Regard21 consists of 3 parts. In part 1, the subject was required to name the colour of 24 dots printed in blue, green, red, or yellow as quickly as possible. Part 2 required the subject to name the colour in which stimuli words were printed and disregard their verbal content; the stimuli words were common words (when, hard, and over) printed in lower case. In part 3, the subjects were required to recognise the coloured stimuli words printed in non-corresponding colours. It gives score in total time taken to complete the task in seconds.
The Digit Span Test22 is commonly used in which the Digit Span Forward is for testing attention and the Digit Span Backward for working memory.
The Verbal Fluency Test (phonological / letter), taken from the NIMHANS Neuropsychological Battery,23 consists of three 1-minute trials. In each trial, the participants were asked to generate as many words as possible that started with a certain letter (Pa, Ka, and Ma), avoiding names, words in non-regional language, and derivatives of the same word. The mean number of correct responses generated in 3 trials was scored.
In the Verbal Fluency Test (semantic / category),23 participants were asked to name as many different animals or fruits as possible in 60 seconds. The total number of correct responses was scored.
Statistical Analysis
Data were analysed using the SPSS 16 Windows version. Association between psychopathology, cognitive functions, and social functioning was computed through Pearson correlation coefficient. Then, multiple regression was done to study variables which were able to predict social functioning in schizophrenia.
Results
Psychopathology
The overall mean PANSS score was 2.62 ± 0.70. The score for positive symptoms was 2.69 ± 0.92, for negative symptoms it was 3.08 ± 1.14, and for general psychopathology it was 2.47 ± 0.68. All the scores fell around a mild level of severity.
Social functioning
The mean ratings for the SCARF-SFI indicated rare to occasional lapses in the different domains of social functioning: self-care, 3.17 ± 1.05; occupational role, 2.29 ± 1.05; family role, 2.23 ± 1.05; social role, 2.48 ± 0.91; and overall score, 2.54 ± 0.85.
Cognitive Functioning
For executive functions, the mean time taken on TMT-B was 189.79 ± 115.2 seconds, and that on Stroop Test was 45.19 ± 22.14 seconds. For verbal working memory, the mean performance on Digit Span Backward was 2.56 ± 1.43. For psychomotor speed / visual scanning, the mean time taken on TMT-A was 1.09 ± 55.03 seconds. The mean attention score on Digit Span Forward was 5.08 ± 1.49. Verbal fluency had a mean score of 11.01 ± 4.96 for semantic type and 3.48 ± 3.48 for phonological type.
Correlation
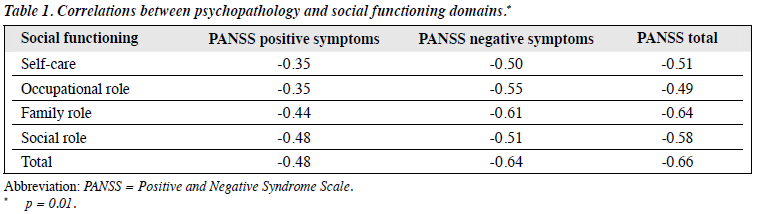
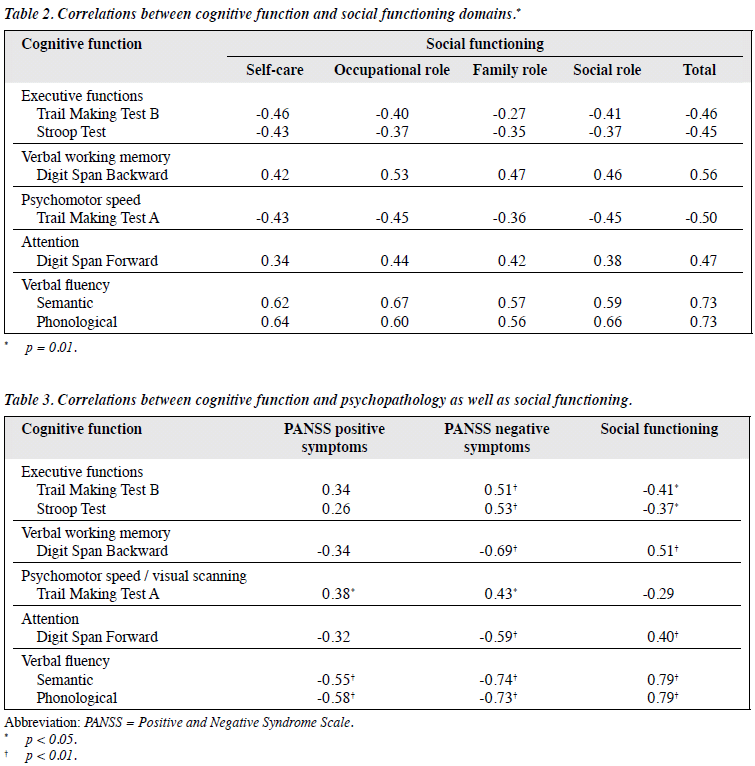
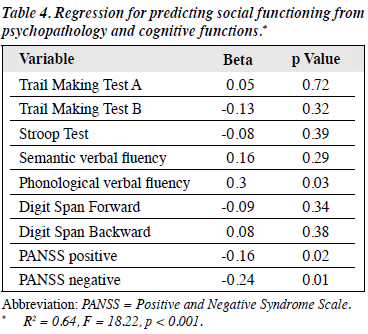
Table 1 shows significant negative correlation of 4 domains of social functioning with the PANSS symptom scales. Table 2 presents the Pearson correlations between various cognitive function tests and social functioning total score and its 4 domains. Among the cognitive test battery, TMT-A, TMT-B, and Stroop Test were significantly negatively correlated with the domains of social functioning; it implied the time taken to complete the task was negatively associated with social functioning. Digit Span Test (forward and backward) and Verbal Fluency Test (semantic and phonological) had significant positive correlations with the social functioning domains. Table 3 shows Pearson correlations between various cognitive function tests and psychopathology. All tests significantly correlated more with the negative symptoms than with positive symptoms. Table 4 shows the results of multiple regression with social functioning as a predicted variable. It shows that among all cognitive test battery, phonological verbal fluency along with positive and negative symptoms was able to predict social functioning.
Discussion
Schizophrenia affects the overall functioning level of patients with this condition. Due to its varied symptoms, every aspect of a patient’s life can be affected. This is become evident from the results of this study. The results have shown impaired social functioning among the study patients, along with the severity of symptoms. The mean rating shows that the patients had rare to occasional lapses in the different domains of social functioning (self-care, occupational role, family role, social role, and overall score). Social functioning was also impaired in an earlier study of patients with schizophrenia, and these deficits included difficulties in the ability to work, to engage in social relationship, to attend to self-care, and to participate in recreational and community activities.24 The domains of social functioning were found to be significantly negatively correlated with the PANSS negative symptom scale, positive symptom scale, and overall symptoms. This implies that the more severe the symptoms become, the greater the impairment to social functioning.
As expected, the cognitive test performance of the participants was also found to be impaired. Heinrichs and Zakzanis25 performed a large-scale comprehensive quantitative meta-analysis of cognitive impairment in schizophrenia, which involved comparison of patients with schizophrenia versus the controls, and found more impairment in cognitive functions of the former. In the present study, it was observed that cognitive function test scores on attention, verbal fluency, and working memory shared a significant positive relationship with all the domains of social functioning.
Executive functions and psychomotor speed / visual scanning had a significant negative correlation with all social functioning domains. These results imply that cognitive function affects all the domains of social functioning. A previous study26 investigating the relationship between symptoms, cognitive function, and the ability to perform basic activities of daily living in patients with schizophrenia also found that cognitive function predicted both concurrent symptoms and ability to perform basic activities of daily living. Cognitive function also predicted more than 40% of the variance in scores for functional need. Green et al27 described how specific neuropsychological defects are predictive of general functioning in schizophrenia. They found that the affected neuropsychological domains in schizophrenia patients included verbal memory, vigilance, and executive function.
Results of the present study showed that attention, verbal fluency, working memory, executive functions, and psychomotor speed are closely linked with social functioning. To improve social functioning, cognitive remediation therapies should target these areas.
Among all cognitive test battery, only psychomotor speed and visual scanning were found to be significantly positively correlated with positive symptoms, which implies that the greater the severity of symptoms, the longer a patient takes to finish the task, suggesting greater dysfunction. Verbal fluency was significantly negatively correlated with positive symptoms, which implies that the greater the severity of symptoms, the less verbal fluency a patient has, therefore greater dysfunction. Besides, all the cognitive function battery shared significant relationship with negative symptoms, implying that the greater the severity of negative symptoms, the greater the cognitive deficits are; the results also suggest that negative symptoms are related to cognitive function to a greater extent than positive symptoms and cause more disability. Greenwood et al28 also investigated whether cognitive impairment differs according to the symptomatology, and found that negative and disorganised dimensions were associated with distinct frontal cognitive impairments.
In order to understand further the relationship between psychopathology, cognitive functions, and social functioning, multiple regression was done with social functioning as a predicted variable. Results showed that among the cognitive test battery, only phonological verbal fluency tests along with positive symptoms and negative symptoms were able to predict the social functioning (R2 = 0.64, F = 18.22, p < 0.001). Verbal fluency is the basic requirement for an individual to function in social setting. It further implies that pharmacotherapy and cognitive remediation for cognitive function in schizophrenia can lead to improvements, not only in cognition and symptoms but also in social functioning. A number of intervention studies, primarily of cognitive remediation, also have shown that some executive and memory improvements are associated with subsequent social functioning change.29-33
The treatment goal is to improve overall functioning of patients with schizophrenia. It is therefore important to study the complex relationship of social functioning with psychopathology and cognitive functions. By understanding which cognitive function influences which social functioning domain, focused cognitive remediation therapy can be designed to target a particular function. As cognitive function was found to be significantly associated with social functioning, improvement in cognitive function could lead to better social functioning.
One of the limitations of our study was that it included only 2 types of schizophrenia. Other types and schizophrenia spectrum disorders can be taken in future studies. Gender- based difference also warrants further study.
Conclusion
Cognitive function and social functioning are impaired in schizophrenia. Cognitive function was found to be significantly associated with negative symptoms and all domains of social functioning. Social functioning was also found to be significantly negatively correlated with the negative and positive symptoms of schizophrenia.
References
- Sadock BJ, Sadock VA, Ruiz P. Kaplan and Sadock’s comprehensive textbook of psychiatry. 9th ed. Baltimore: Williams & Wilkins; 2009: 528.
- Bellack AS. Cognitive rehabilitation for schizophrenia: is it possible? Is it necessary? Schizophr Bull 1992;18:43-50.
- Kuperberg G, Heckers S. Schizophrenia and cognitive function. Curr Opin Neurobiol 2000;10:205-10.
- Mahurin RK, Velligan DI, Miller AL. Executive-frontal lobe cognitive dysfunction in schizophrenia: a symptom subtype analysis. Psychiatry Res 1998;79:139-49.
- Bleuler E. Dementia praecox or the group of schizophrenias (trans. Zinkin J). New York, NY: International Universities Press; 1950: 251.
- Kraepelin E. Dementia praecox and paraphrenia. In: Robertson GM, editor. The 8th German Edition of the textbook of psychiatry vol III, part 2, endogenous dementias (trans. Barclay RM). Edinburgh: Livingstone; 1919: 145-61.
- Diagnostic and Statistical Manual of Mental Disorders. 4th ed., revised. Washington, DC: American Psychiatric Association; 1994.
- Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull 2006;32 Suppl 1:S44-63.
- Pinkham AE, Penn DL, Perkins DO, Lieberman J. Implications for the neural basis of social cognition for the study of schizophrenia. Am J Psychiatry 2003;160:815-24.
- Chan RC, Wang YN, Cao XY, Chen EY. Contribution of working memory components to the performance of the Tower of Hanoi in schizophrenia. East Asian Arch Psychiatry 2010;20:69-75.
- Solanki RK, Singh P, Midha A, Chugh K, Swami MK. Disability and quality of life in schizophrenia and obsessive compulsive disorder: a cross-sectional comparative study. East Asian Arch Psychiatry 2010;20:7-13.
- Addington J, Addington D. Neurocognitive and social functioning in schizophrenia: a 2.5 year follow-up study. Schizophr Res 2000;44:47- 56.
- Basso MR, Nasrallah HA, Olson SC, Bornstein RA. Neuropsychological correlates of negative, disorganized and psychotic symptoms in schizophrenia. Schizophr Res 1998;31:99-111.
- Bellack AS, Morrison RL, Wixted JT, Mueser KT. An analysis of social competence in schizophrenia. Br J Psychiatry 1990;156:809-18.
- Blanchard JJ, Panzarella C. Affect and social functioning in schizophrenia. In: Mueser KT, Tarrier N, editors. Handbook of social functioning in schizophrenia. Needham Heights, MA: Allyn & Bacon; 1998: 181-96.
- Green MF, Nuechterlein KH. The MATRICS initiative: developing a consensus cognitive battery for clinical trials. Schizophr Res 2004;72:1-3.
- Padmavathi P, Thara R, Srinivasan L, Kumar S. SCARF Social Functioning Index. Indian J Psychiatry 1995;37:161-4.
- Kay SR, Opler LA. The positive-negative dimension in schizophrenia: its validity and significance. Psychiatr Dev 1987;5:79-103.
- Army Individual Test Battery. Manual for directions and scoring. Washington, DC: War Department, Adjutant General’s Office; 1944.
- Reitan RM, Wolfson D. The Halstead-Reitan Neuropsychological Test Battery: therapy and clinical interpretation. Tucson, AZ: Neuropsychological Press; 1985.
- Regard M. Cognitive rigidity and flexibility: a neuropsychological study. In: Spreen O, Strauss E, editors. A compendium of neuropsychological tests. Oxford, MA: Oxford University Press; 1998.
- Wechsler D. Wechsler Adult Intelligence Scale (3rd ed). San Antonio, TX: Psychological Corporation; 1997.
- Rao SL, Subbakrishna DK, Gopakumar K. NIMHANS Neuropsychological Battery. Bangalore: NIMHANS Publications; 2004.
- Leary J, Johnstone EC, Owens DG. Social outcome. Br J Psychiatry Suppl 1991;(13):13-20, 44-6.
- Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 1998;12:426- 45.
- Mueser KT, Tarrier N. Handbook of social functioning in schizophrenia. Boston: Allyn & Bacon; 1998.
- Green MF, Olivier B, Crawley JN, Penn DL, Silverstein S. Social cognition in schizophrenia: recommendations from the measurement and treatment research to improve cognition in schizophrenia new approaches conference. Schizophr Bull 2005;31:882-7.
- Greenwood KE, Signmundsson T, Morris RG, Wykes TA. Comparison of profiles of executive impairments in schizophrenia: the relationship with chronicity and symptoms. Schizophr Res 2000;41(special issue):286-7.
- Wykes T, Reeder C. Cognitive remediation therapy: theory and practice. London, England: Brunner Routledge; 2005.
- Reeder C, Newton E, Frangou S, Wykes T. Which executive skills should we target to affect social functioning and symptom change? A study of a cognitive remediation therapy program. Schizophr Bull 2004;30:87-100.
- Wykes T, Reeder C, Corner J, Williams C, Everitt B. The effects of neurocognitive remediation on executive processing in patients with schizophrenia. Schizophr Bull 1999;25:291-307.
- Spaulding WD, Reed D, Sullivan M, Richardson C, Weiler M. Effects of cognitive treatment in psychiatric rehabilitation. Schizophr Bull 1999;25:657-76.
- Penadés R, Boget T, Catalán R, Bernardo M, Gastó C, Salamero M. Cognitive mechanisms, psychosocial functioning, and neurocognitive rehabilitation in schizophrenia. Schizophr Res 2003;63:219-27.