East Asian Arch Psychiatry 2013;23:78-9
EDITORIAL
One day an old gentleman visited my memory clinic. He was a very old retired university professor. He was intolerably good at playing Paduk. Hardly surprising, he could think a mind-boggling 10 to 15 moves ahead. In recent months, he recognised his razor-sharp mind had started to dull. When he could no longer think more than 10 moves ahead, he was sure something was seriously wrong. He himself arranged to visit my memory clinic. However, a neuropsychological battery of tests including the Mini-Mental State Examination (MMSE) revealed nothing amiss. He was adamant that he needed help even though he successfully sailed through every test designed to diagnose early dementia. However, brain magnetic resonance imaging appeared seriously abnormal. Greatly widened sulci and enlarged ventricles and moderate-to-severe atrophy in the frontal and temporal cortex as well as the hippocampi were evident. The anatomical evidences indicated advanced dementia, with a level of damage that would make most people greatly impaired in every cognitive domain. However, for this retired professor, the only impact was that he could no longer play Paduk to high standards.
There have been reports that the brains of people who appeared mentally intact when alive show extensive evidence of the dementia at autopsy. The classical case is that of Sister Bernadette of the Nun Study.1 This was due to the prevailing belief that Alzheimer’s disease is due to a concentration of plaques inside the brain. However, even the brightest of the nuns, who showed no signs of Alzheimer’s disease at all during their lifetime, showed plenty of plaques and tangles when their brains were examined after death.
According to the cognitive reserve theory, very well educated and active people are more able to fend off the symptoms of dementia and brain damage. People who are better educated and more intelligent, lead more intellectually stimulating lives, and have high-status occupations are somehow protected from the mental decline that comes with age. And not just age, but other insults too, including head injuries, effects of alcohol, stroke, and human immunodeficiency virus, as well as Alzheimer’s and Parkinson’s diseases. Dementia is not a dichotomised condition like appendicitis or pneumonia, but rather a process that evolves over decades and interacts with many other factors. When dementia symptoms first appear, the level of brain pathology in different individuals varies.
No More a Constant Cutoff Score to Diagnose Cognitive Impairment and Dementia
Contrary to our common sense, there exists no clear definition of how to dichotomise the presence or absence of the essential features of dementia. Yet amnesia, agnosia, aphasia, apraxia, and executive dysfunction are 5 abnormalities specifically utilised as diagnostic criteria of dementia in the Diagnostic and Statistical Manual of Mental Disorders and the International Classification of Diseases. In other words, dementia has been diagnosed not by clear definitions but by the arbitrary standard (i.e. a cutoff score of a test).
For example, there have been countless publications related to dementia using the MMSE.2 It is a brief 30-point questionnaire test to screen for cognitive impairment and dementia, to estimate severity, and to follow the course of cognitive changes in an individual over time. Any score of ≥ 25 points (out of 30) indicates normal cognition. Lower scores indicate mild (21-24 points), moderate (10-20 points), or severe (≤ 9 points) cognitive impairment. Numerous foreign language versions of the MMSE have been validated and published locally and internationally. Excellent sensitivity and specificity of each version have been proposed.
However, too many false-positive or false-negative cases appear when applying the MMSE to diagnose dementia or cognitive impairment. A perfect MMSE score of 30 can never rule out dementia. Low to very low scores correlate closely with the presence of dementia, but they even cannot guarantee the presence of dementia or cognitive impairment. This shortcoming is not limited to the MMSE but to any tools or batteries for cognitive assessment tests using cutoff scores to distinguish the abnormal from the normal.
Pitfalls in Widely Used Cognitive Tests
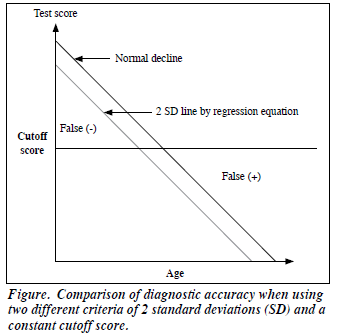
Screening tools or neuropsychological batteries using constant cutoff points inevitably produce false-positive and false-negative cases as soon as a cutoff point is set, so that they cannot properly diagnose or rule out dementia. The older the subject, the more false-positive there may be, and younger persons are prone to false-negatives. Generally speaking, this is because cognition declines with age. In view of educational attainment, there are more false- negative cases in the better educated, while there are more false-positives in illiterate subjects.
Like the retired professor, some individuals cannot be diagnosed as having dementia using current screening tools or batteries of neuropsychological tests. I met a very old woman, aged 85, whose the MMSE score was 10 but she was normal and even wise enough to give sensible advice to the younger generation. She was illiterate and had never left her home village, and never used money to make purchases (something her husband did instead). There was no need to clearly recognise the year, month, day and date for her daily life. There was no need for her to calculate. However, she knew everything intuitively. Therefore, it is essential to eliminate the effects of age and education on test scores when assessing cognition. Constant cutoff scores must not be used any more. There is a better way.
According to medical tradition, dichotomised professional judgement (i.e. presence of a murmur, wheezing) or pathology (e.g. appendicitis) has been a gold standard to clearly distinguish the normal from the abnormal. However, in psychological modelling, the normal and the abnormal exist as a continuum in terms of a normal distribution (i.e. intelligence quotient [IQ]). Assuming a normal distribution, unusual values are those that are more than 2 standard deviations (SD) away from the mean. Then, 95% of values lie within 2 SD of the mean while 5% lie outside this range. For example, in the IQ distribution, the mean is 100 and the SD is 15. Using this notion, mental retardation has been defined when the IQ is ≤ 70 (more than 2 SD below the mean).3 Even this notion has been exploited for the definition of mild cognitive impairment (MCI), a condition referred to when there is an IQ of ≤ 1.5 SD below the mean.4,5
Elimination of Age and Education Effects on the Test Score
In statistics, regression analysis is a technique for estimating the relationships between variables. It includes many techniques for modelling and analysing several variables, when the focus is on the relationship between a dependent variable and one or more independent variables. More specifically, regression analysis helps one understand how the typical value of the dependent variable changes when any one of the independent variables is varied, while the other independent variables are held fixed. Age and education are the independent variables while the test score is the dependent variable. For example, the linear regression equation to eliminate effects of age and education on the test score is as follows:
Test score = a * age + b * duration of education + c * other independent variable + … + a constant
To distinguish the abnormal (i.e. > 2 SD) from the normal, a large-scale community-based epidemiological study should be conducted to establish the norm among the total population by finding the mean and SD resulting from the battery of tests. Thereafter, the abnormal can be defined by an algorithm as follows:
If test score < score at 2 SD, then ‘normal’, or
If test score > score at 2 SD, then ‘abnormal’.
The individual-specific score of 2 SD should be determined by age and education of a testee. Therefore, there is no constant cutoff score but it varies by age and education of the individual. This way using 2 SD instead of a single cutoff score is a better method that can greatly reduce false-positives and false-negatives when screening for cognitive impairment or dementia (Fig). As mentioned earlier, this notion has been already adopted to diagnose mental retardation and MCI.
To adopt the new way of using 2 SD instead of a constant cutoff score, it is recommended to use computer- assisted tests or batteries using the norm of total population. Thus, the computer can calculate the 2 SD point of an individual of certain age and certain number of years of education to define what to call an abnormal score.
There have been neuropsychological battery tests adopted to using 2 SD instead of a single cutoff score to diagnose dementia.6,7 A large-scale nationwide community- based epidemiological study was conducted to establish norms [unpublished data].
Recent advances in information technology can help us to adopt these new methods. The platform to set such a test or battery of tests must be widely popular, and devices like tablet computers and laptops can be useful and convenient in this respect. In the near future, such computer-assisted testing will replace paper and pencil tests to eliminate effects of age and education on the test score, and in so doing greatly increase diagnostic accuracy.
Guk-Hee Suh, MD, PhD (email: suhgh@chol.com)
Department of Psychiatry, Dongtan Sacred Heart Hospital, Hwaseong, Korea
References
- Snowdon D. Aging with grace: what the Nun Study teaches us about leading longer, healthier, and more meaningful lives. Bantam Books; 2001.
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician”. J Psychiatr Res 1975;12:189-98.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington DC: APA; 1994.
- Petersen RC, Smith GE, Waring SC, Ivnik RJ, Kokmen E, Tangelos EG. Aging, memory, and mild cognitive impairment. Int Psychogeriatr 1997;9:65-9.
- Petersen RC, Doody R, Kurz A, Mohs RC, Morris JC, Rabins PV, et al. Current concepts in mild cognitive impairment. Arch Neurol 2001;58:1985-92.
- Suh GH, Lee MH. Cognitive Assessment and Reference Diagnoses System: development of a neuropsychological and clinical examina- tion for clinic and population use. Psychogeriatrics 2003;3:54-62.
- Suh GH. Diagnostic capability of the Cognitive Assessment and Reference Diagnoses System (CARDS). J Korean Geriatr Psychiatry 2002;6:128-35.