East Asian Arch Psychiatry 2013;23:139-43
ORIGINAL ARTICLE
陈发展、项玉涛、陆峥、王刚、胡晨、AM Kilbourne、GS Ungvari、方贻儒、司天梅、杨海晨、黎以菁、 胡建、陈致宇、黄颐、孙静、王小平、李惠春、张晋碚、张向阳、赵凤琴
Dr Fa-Zhan Chen, MD, Department of Psychiatry, Tongji Hospital, Tongji University School of Medicine, Shanghai, China.
Dr Yu-Tao Xiang, MD, PhD, Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong SAR, China; Mood Disorders Center, Beijing Anding Hospital, Capital Medical University, Beijing, China.
Dr Zheng Lu, MD, Department of Psychiatry, Tongji Hospital, Tongji University School of Medicine, Shanghai, China.
Dr Gang Wang, PhD, MD, Mood Disorders Center, Beijing Anding Hospital, Capital Medical University, Beijing, China.
Dr Chen Hu, MD, Mood Disorders Center, Beijing Anding Hospital, Capital Medical University, Beijing, China.
Dr Amy M. Kilbourne, PhD, Department of Psychiatry, University of Michigan Medical School; Veterans Administration Center for Clinical Management Research, Ann Arbor, Michigan, United States.
Dr Gabor S. Ungvari, MD, PhD, The University of Notre Dame Australia / Marian Centre, Perth, Australia.
Dr Yi-Ru Fang, MD, Division of Mood Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China. Dr Tian-Mei Si, MD, PhD, Peking University Institute of Mental Health, Beijing, China.
Dr Hai-Chen Yang, MD, PhD, Division of Mood Disorders, Shenzhen Mental Health Center, Shenzhen, China.
Dr Kelly Yee-Ching Lai, MD, Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong SAR, China.
Dr Jian Hu, MD, The First Affiliated Hospital of Harbin Medical University, Harbin, China.
Dr Zhi-Yu Chen, MD, The Seventh People’s Hospital of Hangzhou, Hangzhou, China.
Dr Yi Huang, MD, West China Hospital, Sichuan University, Chengdu, China. Dr Jing Sun, MD, Affiliated Nanjing Brain Hospital, Nanjing Medical University, Nanjing, China.
Dr Xiao-Ping Wang, MD, Mental Health Institute, The Second Xiangya Hospital, Central South University, Changsha, China.
Dr Hui-Chun Li, MD, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China.
Dr Jin-Bei Zhang, MD, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, China.
Dr Xiang-Yang Zhang, MD, PhD, Menninger Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, Texas, United States.
Dr Helen Fung-Kum Chiu, MD, Department of Psychiatry, The Chinese University of Hong Kong, Hong Kong SAR, China.
Addresses for correspondence:
Dr Yu-Tao Xiang, Department of Psychiatry, The Chinese University of Hong Kong, G/F, Multicentre, Tai Po Hospital, Tai Po, New Territories, Hong Kong SAR, China.
Tel: (852) 2607 6031; Fax: (852) 2647 5321; Email: xyutly@gmail.com
Dr Zheng Lu, Department of Psychiatry, Tongji Hospital, Tongji University School of Medicine, Shanghai 200065, China.
Tel: (86) 18017311151; Email: luzheng@tongji.edu.cn
Submitted: 7 May 2013; Accepted: 24 June 2013
Abstract
Objectives: Bipolar disorder is often misdiagnosed as major depressive disorder. Such misdiagnosis partly depends on the type of treatment setting. This study compared general hospital psychiatric units with psychiatric hospitals in China with respect to basic demographic and clinical characteristics of patients with unrecognised bipolar disorder who are treated for major depressive disorder.
Methods: Patients treated for major depressive disorder were consecutively examined in 13 health centres (6 general hospital psychiatric units and 7 psychiatric hospitals) in China. Their socio-demographic and clinical features were recorded using a standardised protocol and data collection procedure. The DSM-IV diagnoses were established using the Mini-International Neuropsychiatric Interview.
Results: Of the 1487 patients included in the study, 309 (20.8%) were diagnosed with bipolar disorder. There was no significant difference between general hospital psychiatric units and psychiatric hospitals in the ratio of all types of unrecognised bipolar disorders (χ2 = 0.008, degrees of freedom = 1, p = 0.9) and bipolar II disorders (χ2 = 3.1, degrees of freedom = 1, p = 0.08). The proportions of unrecognised bipolar I disorders (χ2 = 4.1, degrees of freedom = 1, p = 0.04) differed significantly between the 2 types of study site. Multivariate analyses showed that patients with bipolar I disorders with more seasonal depressive episodes were more likely to receive treatment in general hospital psychiatric units (odds ratio = 3.3, 95% confidence interval = 1.1-9.8).
Conclusion: Patients with bipolar I disorders receiving treatment in general hospital psychiatric units had different clinical characteristics compared to their counterparts treated in psychiatric hospitals in China.
Key words: Bipolar disorder; China; Mental health services
摘要
目的:双相情感障碍往往被误诊为重度抑鬱症。这样的误诊在一定程度上取决於治疗环境。本研究旨在比较中国各地的综合医院精神科部门与精神病院其重度抑鬱症患者的未被识别双相情感障碍的人口统计学和临床特徵。
方法:纳入中国13间卫生服务中心(包括6间综合医院精神科部门和7间精神病院)的重度抑鬱症患者,并采用标準化协议和数据收集程序记录其社会人口统计学和临床特徵。使用简明国际神经精神访谈作DSM-IV诊断。
结果:共1487名重度抑鬱症患者被纳入研究,当中309名(20.8%)被诊断双相情感障碍。两类研究点於各种未被识别双相情感障碍的比例(χ2 = 0.008,df = 1,p = 0.9)和双相情感障碍II型(χ2 = 3.1,df = 1,p = 0.08)均无显著差异,但未被识别双相情感障碍I型方面(χ2 = 4.1, df = 1,p = 0.04)则有明显差异。多变量分析显示,季节性抑鬱病发次数较多的双相情感障碍I型患者较大机会於综合医院精神科部门接受治疗(比值比 = 3.3,95%置信区间 = 1.1-9.8)。
结论:於综合医院精神科部门接受治疗的双相情感障碍I型患者,其临床特徵跟在精神病院的相对群组有所不同。
关键词:双相情感障碍、中国、精神健康服务
Introduction
In clinical practice, depressive episodes in bipolar disorders (BD) are typically more frequent and last longer than manic or hypomanic episodes.1 Therefore, patients with BD are more likely to be misdiagnosed and treated for a major depressive disorder (MDD).2 Different types of psychiatric services attract different clients,3 and BD patients treated in different settings have different demographic and clinical features.4-8 To date, no study has explored the characteristics of unrecognised BD patients between different mental health care settings anywhere in the world, including China.
Psychiatric hospitals (PHs) and general hospital psychiatric units (GHPUs) are the 2 major types of mental health services available in China. Psychiatric hospitals, usually located in suburban areas, provide both inpatient and outpatient services for patients with severe psychiatric symptoms, particularly for those with violent behaviours, refractory symptoms, and high risk of suicide. Relative to GHPUs, PHs usually provide more intensive services, such as medication and electroconvulsive therapy, and a considerable proportion of inpatients in PHs are admitted suddenly. In contrast, GHPUs are usually located in cities and provide more accessible outpatient services for patients with no aggressive symptoms and less risk of suicide. Some large GHPUs also provide less intensive inpatient services. As GHPUs are established in general hospitals, patients with somatic symptoms and major medical conditions can be easily referred to medical departments. We hypothesised that the type of treatment setting could predict different socio-demographic and clinical characteristics of unrecognised BD among patients treated for MDD. Understanding these characteristics of unrecognised BD patients could facilitate their early identification and improve clinical outcomes.
To improve the early recognition of BD in China, the Chinese Society of Psychiatry initiated the Diagnostic Assessment Service for People with bipolar disorders (DASP). Understanding how recognition and management of BD might differ by facility type can inform the tailored interventions that are most appropriate for different types of treatment setting. This study, which is a secondary analysis of the data from the DASP project,9 compared PHs and GHPUs in China with respect to socio-demographic and clinical features of BD patients misdiagnosed with MDD.
Methods
Study Participants and Settings
The DASP project was carried out in 13 major teaching mental health centres (6 GHPUs and 7 PHs) geographically located in the north, south, east, west, and central parts of China, representing a wide range of clinical settings, from 1 September 2010 to 28 February 2011. The study method has been described in detail elsewhere.9 Briefly, inpatients and outpatients aged between 16 and 65 years were enrolled if they had a diagnosis of MDD according to the DSM-IV or ICD-10 criteria based on a review of medical records. The patients were given an explanation about the aims of the study and they or their guardians (for patients < 18 years) provided written informed consent. Exclusion criteria included a history of, or ongoing significant medical or neurological condition(s), depressive disorder secondary to a medical condition, or electroconvulsive therapy administered in the past month. The study protocol was approved by the Clinical Research Ethics Committees of the participating centres.
Instruments and Assessment
Inpatients and outpatients with a diagnosis of MDD receiving treatment in the participating hospitals / units were consecutively referred to the research team at each site for eligibility screening. All patients fulfilling the study criteria were invited to participate in the study. All members of the research team were psychiatrists.
A diagnostic assessment was conducted using the validated Chinese version of the Mini-International Neuropsychiatric Interview (MINI) version 5.0 to establish the DSM-IV diagnoses of MDD and BD-I or BD-II.10,11 Only previously undiagnosed BD patients were included for analysis. After providing informed consent, patients completed the clinical assessment. Additional demographic data were collected from chart reviews. All 13 raters in the study were trained in diagnosing BD using the MINI in 20 MDD patients prior to the study. In this reliability exercise, the raters’ judgements of BD were compared with the best- estimate lifetime diagnoses12; the kappa values were above 0.85 for each rater.
Statistical Analyses
Comparisons of patients’ socio-demographic and clinical characteristics between PHs and GHPUs were performed by independent sample t test and Chi-square test as appropriate. Stepwise multiple logistic regression analyses were used to identify independent demographic and clinical correlates of treatment settings separately for BD-I and BD-II. The variables that were statistically significant in the univariate analysis were entered as independent variables, while seeking treatment in different settings (GHPU vs. PH) was the dependent variable. The significance level was set at 0.05 (2-tailed).
Results
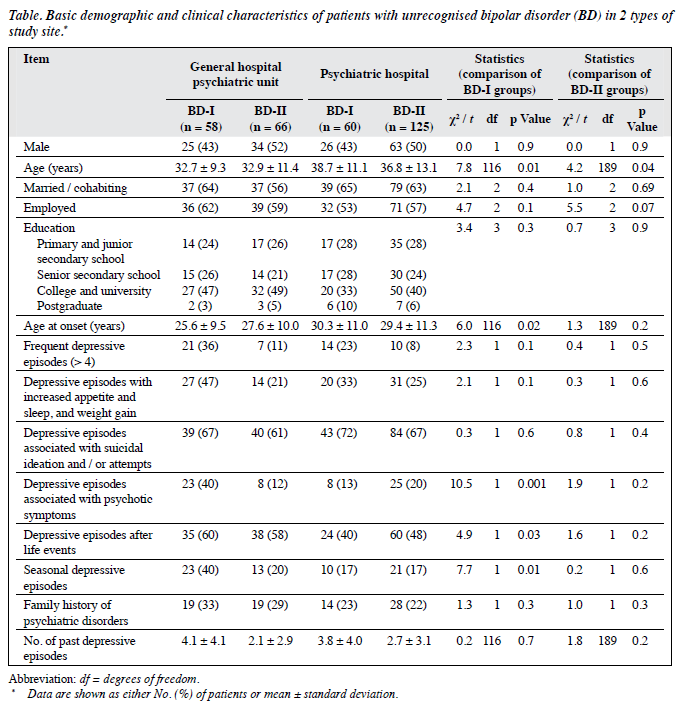
A total of 1757 patients diagnosed with MDD were invited to participate in the study; 270 (15.4%) refused to participate or failed to complete the interview. Among the 1487 patients who participated in the study, 600 were from GHPUs and 887 were from PHs. A total of 309 patients were diagnosed with BD (Table). There were no significant differences between GHPUs and PHs in the ratio of unrecognised BD (all types) [χ2 = 0.008, degrees of freedom (df) = 1, p = 0.9] and BD-II (χ2 = 3.1, df = 1, p = 0.08). The proportions of unrecognised BD-I (χ2 = 4.1, df = 1, p = 0.04) differed significantly between the 2 types of study site.
The Table shows the socio-demographic and clinical characteristics of previously undiagnosed BD patients. Previously undiagnosed BD-I patients in GHPUs were significantly younger, had earlier onset of disease, more lifetime psychotic symptoms, more depressive episodes following stressful life events, and more seasonal depressive episodes than those in PHs. In contrast, the only significant difference in previously undiagnosed BD-II patients was that those in GHPUs were younger than those in PHs.
Stepwise multivariate logistic regression analysis showed that previously undiagnosed BD-I patients having more seasonal depressive episodes (odds ratio = 3.3, 95% confidence interval = 1.1-9.8) were more likely to receive treatment in GHPUs. Only younger age was significantly associated with treatment setting in the univariate analyses for BD-II patients, so multiple logistic regression analysis was not conducted.
Discussion
The results of this study support the hypothesis that the basic demographic and clinical characteristics of BD patients significantly differ between PHs and GHPUs. Earlier studies explored the characteristics of BD patients treated at entirely different types of health care facility such as primary care versus tertiary PHs,6,8 which makes direct comparison less consequential. Compared with BD-II patients, BD-I patients are usually characterised by more aggressive and violent behaviours, so they are more likely to receive treatment in PHs.
This study found that seasonal depressive episodes can predict BD-I patients receiving treatment in GHPUs. Seasonality may result in more distress and impairment than chronically low mood and may have an independent effect on cardiovascular health.13 Greater seasonality in MDD may independently reflect increased severity and health service utilisation.14 Therefore, it was assumed that depressed patients with more frequent seasonal episodes repeatedly visited their general practitioners which, in turn, may have increased their chances of using mental health services in general hospitals. In addition, the dual vulnerability hypothesis15 suggests that vulnerability to seasonal variation in mood symptoms may be distinct from vulnerability to MDD; seasonal variation of mood symptoms might represent a unique dimension of psychopathology. This study suggests that seasonality is an important factor in unrecognised BD contributing to the choice of treatment setting.
The mechanism underlying the relationship between patients’ characteristics and the type of mental health service is still unclear. Earlier models on the use of health services may help explain these findings. Penchansky and Thomas16 described the 5 ‘A’s of access of affordability, acceptability, accommodation, accessibility, and availability to illustrate the overall dimensions between patients and providers. Accessibility and availability are especially relevant in maintaining longitudinal treatment retention of patients with severe mental illnesses.17 Pescosolido and Boyer18 also developed a network-episode model in which 4 components work interactively to influence the decision to use or continue using mental health services: (1) patients’ socio- demographic variables and personal health background and organisational constraints to accessing care, such as finance; (2) social support system that consists of the social network structure, content, and function; (3) illness career comprising factors such as sick role, recovery, compliance, and spacing of consultations; and (4) a treatment system that encompasses structure, content, and functions of the treatment network.
In China, there are far fewer PHs than GHPUs, although PHs remain the mainstay of the mental health services.19 In this study, earlier onset, more psychotic symptoms, more depressive episodes following life events, and more seasonal depressive episodes in BD-I patients rendered the clinical condition more complex. Given the above models, it was assumed that accessibility and availability of institutions were mainly responsible for the fact that patients with more severe and complex clinical conditions received treatment in GHPUs. A patient’s socio-demographic background is also an important factor influencing the decision to choose the type of mental health service according to the network-episode model.18 However, the impact of age cannot be explained because of the design of this study.
One of the strengths of this study is its large nationwide representative sample. The limitations include (1) a small proportion of patients refused to participate in the study, which might bias the findings; (2) the cross- sectional design which did not reflect the dynamic processes of the clinical phenomena of BD; (3) some important contributors to misdiagnosis such as the clinical experience of the treating psychiatrists, course of illness, and number of hospitalisations, compulsory admissions, and manic episodes were not measured; and (4) only BD-I or -II could be diagnosed using the MINI.
The findings of this study could help mental health professionals to identify unrecognised BD in patients diagnosed with MDD earlier, particularly those with more seasonal depressive episodes receiving treatment in general hospitals.
Acknowledgements and Declaration
This study was funded by the National Key Scientific and Technological Projects for the 11th Five-Year Plan from the Ministry of Science and Technology of the People’s Republic of China (Project Title: “Early Diagnostic Assessment and Standardized Treatment Approach for Depression”; No.: 2007BAI17B05). The authors declared no conflict of interest in this study. This study was launched by the Chinese Society of Psychiatry with support from AstraZeneca China. AstraZeneca China had no role in the study design, or in generating and interpreting the results. The authors are grateful to all the clinicians who helped to organise the study in each study site.
References
- Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry 2003;60:261-9.
- Bowden CL. A different depression: clinical distinctions between bipolar and unipolar depression. J Affect Disord 2005;84:117-25.
- Ettner SL. The setting of psychiatric care for medicare recipients in general hospitals with specialty units. Psychiatr Serv 2001;52:237-9.
- Burns BJ, Ryan Wagner H, Gaynes BN, Wells KB, Schulberg HC. General medical and specialty mental health service use for major depression. Int J Psychiatry Med 2000;30:127-44.
- Katz G, Durst R, Shufman E, Bar-Hamburger R, Grunhaus L. A comparative study of psychiatric inpatients in a general hospital and a psychiatric hospital in Israel: demographics, psychopathological aspects and drug abuse patterns. Isr Med Assoc J 2011;13:329-32.
- Copeland LA, Zeber JE, Valenstein M, Blow FC. Racial disparity in the use of atypical antipsychotic medications among veterans. Am J Psychiatry 2003;160:1817-22.
- Fernández A, Haro JM, Codony M, Vilagut G, Martínez-Alonso M, Autonell J, et al. Treatment adequacy of anxiety and depressive disorders: primary versus specialised care in Spain. J Affect Disord 2006;96:9-20.
- Kilbourne AM, Goodrich D, Miklowitz DJ, Austin K, Post EP, Bauer MS. Characteristics of patients with bipolar disorder managed in VA primary care or specialty mental health care settings. Psychiatr Serv 2010;61:500-7.
- Hu C, Xiang YT, Ungvari GS, Dickerson FB, Kilbourne AM, Si TM, et al. Undiagnosed bipolar disorder in patients treated for major depression in China. J Affect Disord 2012;140:181-6.
- Si TM, Shu L, Dang WM, Se YA, Chen JX, Dong WT, et al. Evaluation of the reliability and validity of Chinese version of the Mini-International Neuropsychiatric Interview in patients with mental disorders. Chin Ment Health J 2009;23:493-503.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22-33.
- Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 1982;39:879-83.
- Bjorvatn B, Sagen IM, Øyane N, Waage S, Fetveit A, Pallesen S, et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res 2007;16:66-76.
- Vigod SN, Levitt AJ. Seasonal severity of depressive symptoms as a predictor of health service use in a community-based sample. J Psychiatr Res 2011;45:612-8.
- Lam RW, Tam EM, Yatham LN, Shiah IS, Zis AP. Seasonal depression: the dual vulnerability hypothesis revisited. J Affect Disord 2001;63:123-32.
- Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care 1981;19:127-40.
- McCarthy JF, Blow FC, Valenstein M, Fischer EP, Owen RR, Barry KL, et al. Veterans Affairs Health System and mental health treatment retention among patients with serious mental illness: evaluating accessibility and availability barriers. Health Serv Res 2007;42:1042-60.
- Pescosolido BA, Boyer CA. How do people come to use mental health services? Current knowledge and changing perspectives. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: social contexts, theories, and systems. Cambridge: Cambridge University Press; 1999: 392-411.
- Liu J, Ma H, He YL, Xie B, Xu YF, Tang HY, et al. Mental health system in China: history, recent service reform and future challenges. World Psychiatry 2011;10:210-6.
Corrigendum
“Differences in Brain Metabolism Associated with Agitation and Depression in Alzheimer’s Disease” (2013;23:86-90). We have been informed by authors of this paper that the Chinese name of the second author should have read “洪嘉蔚”.