Hong Kong J Psychiatry 2004;14(1):2-9
ORIGINAL ARTICLE
Dr SKW Cheng, PhD, MSoSc, BSoSc, AFHKPS, Clinical Psychologist, Kwai Chung Hospital, Hong Kong, China.
Dr BKL Cheung, MBBS, MRCPsych, FHKAM(Psych), Senior Medical Officer, Kwai Chung Hospital, Hong Kong, China.
Address for correspondence: Dr SKW Cheng, Clinical Psychology Service, Kwai Chung Hospital, Hong Kong, China.
E-mail: sammykcheng@cuhk.edu.hk
Submitted: 7 December 2001; Accepted: 7 June 2002
Abstract
Objective: This study aimed to examine the psychometric properties and factor structure of the Chinese versions of 2 rating scales: the revised Subjective Opiate Withdrawal Scale and the Objective Opiate Withdrawal Scale.
Patients and Methods: The study comprised 2 parts. In study 1, fifty one patients with a diag- nosis of opioid dependence (76.6% male, 23.4% female; mean age, 35.60 ± 11.15 years) were assessed with the revised Subjective Opiate Withdrawal Scale and Objective Opiate Withdrawal Scale after admission to Kwai Chung Hospital for detoxification. In study 2, sixteen patients with a diagnosis of opioid dependence (50.0% male, 50.0% female; mean age, 34.40 ± 10.84 years) admitted to Kwai Chung Hospital for detoxification, were recruited. The revised Subjec- tive Opiate Withdrawal Scale and Objective Opiate Withdrawal Scale were administered on days 1, 2, 7, and 14 of a methadone detoxification programme.
Results: The reliabilities of the 2 scales were shown to be satisfactory. Four meaningful factors emerged in the results of factor analyses for the revised Subjective Opiate Withdrawal Scale, whereas a single-factor solution was found to adequately account for the data-set of the Objec- tive Opiate Withdrawal Scale. Consistent with expectations, a steady reduction profile of opiate withdrawal features was present in the measures of the revised Subjective Opiate Withdrawal Scale, whereas the Objective Opiate Withdrawal Scale was less sensitive in measuring the changes.
Conclusion: The revised Subjective Opiate Withdrawal Scale and Objective Opiate Withdrawal Scale were found to have satisfactory psychometric properties and different factor structures. Salient findings and recommendations for future investigation were discussed.
Key words: Factor structure, Opiate dependence, Psychometrics
Introduction
Opiate addiction remains a major problem among users of illicit drugs in Hong Kong. According to the statistics of the Central Registry of Drug Abuse (CRDA) from 1995 to 2000, opiate misuse accounted for approximately 80% of com- mon drug abuses.1 In the latest guide for drug addiction treatment, it is emphasised that effective drug interventions should adopt a biopsychosocial approach to address the com- plex and multiple needs of patients. Detoxification alone is insufficient to achieve long-term abstinence.2 However, the principle of operant theory predicts that the undesirable consequences (the presence of withdrawal symptoms) of discontinuing drug-taking behaviours can serve as a power- ful negative reinforcer to maintain drug use.3,4 Indeed, local substance abusers have reported that the major reason for current drug use (approximately 55%) was to “avoid dis- comfort of its absence”.1 Therefore, pharmacological treat- ment plays a pivotal role in reducing withdrawal symptoms and the associated fear that keep addicted people away from treatment.
In recent decades, new treatment strategies for opiate addiction, such as using opiate receptor antagonists and rapid opiate detoxification under general anaesthesia, have become increasingly common.5-7 Inventing novel pharmacological treatment can minimise withdrawal symptoms and hence facilitate participation in treatment. To document and compare the various treatment approaches for effective detoxification, psychometrically sound measures are necessary.
The Subjective Opiate Withdrawal Scale (SOWS) and Objective Opiate Withdrawal Scale (OOWS) are 2 of the scales developed by Handelsman et al to measure opiate withdrawal signs and symptoms.8 The former assesses 16 covert withdrawal symptoms reported by individuals, whereas the latter examines 13 overt signs checked by observers. Handelsman et al8 showed that these measures had adequate reliability and validity, and Loimer et al9 sub- sequently replicated the satisfactory validity of the scales. However, the latter revealed that the 2 scales did not have a significant correlation.9 A few questions or limitations re- main to be addressed.
Firstly, because the SOWS and OOWS were built on previous empirical work (the Addiction Research Center Inventory10 and Himmelsbach Scale11), their conceptuali- sation of opiate withdrawal symptoms might be different from the current concept. In fact, when compared with the Diagnostic and Statistical Manual of Mental Disorders (DSM IV)12 and the International Classification of Mental and Behavioural Disorders (ICD-10),13 5 subjective opiate withdrawal symptoms are not listed in the scales. Thus, there is a need to re-examine the psychometric properties of the scales (particularly the SOWS) if these items are included.
Secondly, what are the factor structures of the scales? Handelsman et al argued that SOWS and OOWS could measure and reflect symptoms of various domains includ- ing motor, autonomic, gastrointestinal, musculoskeletal, and psychiatric.8 However, there was no empirical investigation on the factor structures of the scales in previous studies.8,9 The findings in another similar scale (the Opiate Withdrawal Scale) showed that the single-factor solution model explained the data in a sample comprising 82 opiate addicts.14,15 Empirical examinations of the factor structure may shed light on the future understanding of specific mechanisms or changes of withdrawal symptoms in the process of detoxification. For instance, if both autonomic and psychi- atric factors are indeed present, would one sustain longer than the other during the detoxification process, or would they respond differently to different types of drugs or treat- ment modalities (such as pharmacological versus psycho- logical therapies)? These interesting questions may invite future research to evaluate different treatment programmes for detoxification and motivation enhancement.
Thirdly, could the Chinese versions of the revised SOWS and OOWS yield acceptable reliability and validity? So far, there is no validated Chinese opiate withdrawal scale avail- able in the literature. Although SOWS and OOWS are noted to be clinically applicable in different samples in the West, empirical evaluation is required for local patients.
In sum, the purpose of the present project was to exam- ine the psychometric properties and factor structures of the Chinese versions of the revised SOWS and OOWS in Hong Kong Chinese opiate addicts.
Patients and Methods
Instruments
The following instruments were used in the analysis.
The Chinese version of the revised SOWS is a 21-item scale in which respondents have to give each item a rating from 0 to 4 (0 = not at all, 1 = a little, 2 = moderately, 3 = quite a bit, 4 = extremely), indicating the severity of the symp- toms at the time of the test. The original SOWS consisted of 16 perceived symptoms. However, in the revised version, 5 more symptoms were added based on the description of the DSM IV and ICD-10 for opiate withdrawal symptoms. The new symptoms included are ‘dysphoria’,‘insomnia’, ‘craving for an opioid drug’, ‘diarrhoea’, and ‘racing heart’. Scores of the revised SOWS range from 0 to 84.
The Chinese version of the OOWS is a 13-item scale in which observers check for the presence or absence of with- drawal signs. Scores for the OOWS could fall into a range from 0 to 13.
To ensure the meanings of the items being correctly translated, the backward translation method was adopted. A clinical psychology trainee and the first author performed the initial and backward translation, respectively. They also subsequently checked the items’ meaning before adminis- tering the scale to patients.
Study 1
Fifty one Chinese patients, 40 men and 11 women, with a DSM-IV diagnosis of opioid dependence participated in the study. Potential participants were admitted to Kwai Chung Hospital for opiate detoxification. The inclusion criteria for the participants were as follows:
- conforming to the DSM-IV diagnostic criteria for opiate dependency
- deprivation of methadone or heroin for 12 to 18 hours
- Chinese ethnicity
- definitive intention to stop drug use.
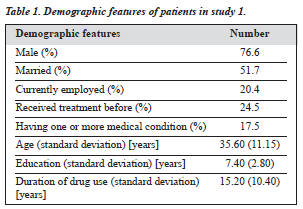
As the purpose of the study was to evaluate the initial opiate withdrawal patterns, the participants completed the scales during the first day of hospital admission. The demo- graphic data of this group are presented in Table 1.
Results
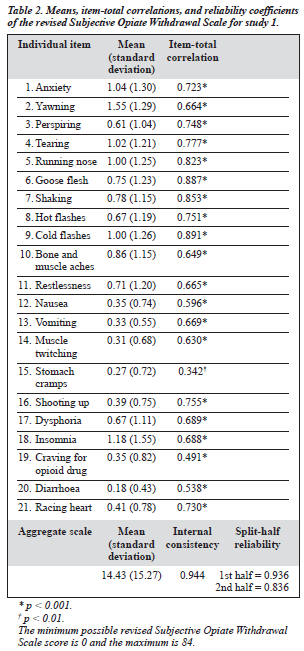
As initial t tests and correlational analyses indicated no sex and age differences in scores of both the revised SOWS and OOWS, all the data were combined in the subsequent statistical analyses. Descriptive data, item-total correlation, and reliability coefficients of the revised SOWS are presented in Table 2. The 3 most distressing symptoms during the initial withdrawal phase in this sample were ‘yawning’, ‘insomnia’, and ‘anxiety’, whereas the relatively less dis- turbing ones included ‘diarrhoea’, ‘stomach cramps’, and ‘muscle twitching’. The item-total correlation coefficients were all significant, ranging from 0.342 to 0.891, with an average of 0.693. Both the coefficients of internal consistency (alpha) and split-half reliability were excellent.
The descriptive data, item-total correlation, and reliabil- ity coefficients of the OOWS are presented in Table 3. The most commonly observed withdrawal signs consisted of ‘hot and cold flashes’, ‘yawning’, and ‘anxiety’, while the infrequently observed ones were ‘piloerection’, ‘tremors’, ‘vomiting’, ‘muscle twitches’, and ‘abdominal cramps’. These objective signs were highly consistent with the subjectively reported symptoms. The item-total correlation coefficients were again all significant, ranging from 0.237 to 0.807, with an average of 0.525. The coefficients of internal consistency (alpha) and split-half reliability were acceptable.
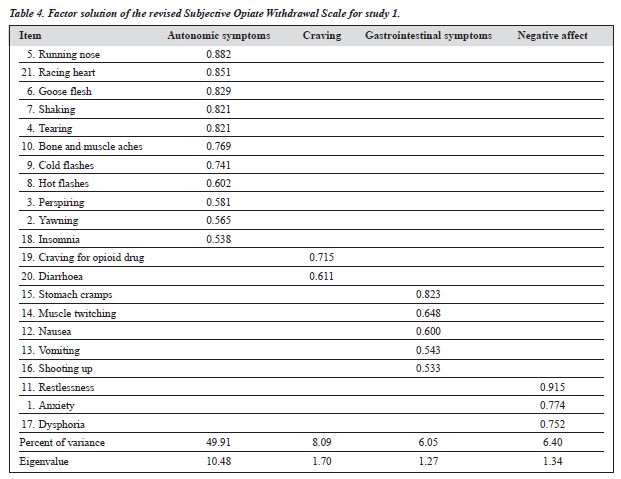
To examine the structural validity of the scales, factor analyses were conducted in the following procedure. Firstly, in the revised SOWS, the principal component method was employed and 5 factors with eigenvalues greater than unity emerged. Secondly, direct oblimin rotation analyses were applied to improve the interpretability of all 5 factor structures. Thirdly, an optimal factor structure was selected and decided by comparing the relative structural stabilities or the size of factor loadings.16 This method is superior to other methods such as the scree test17 where the sample size for factor analyses is small. We used a conservative cut-off, factor loading of 0.53, to eliminate unstable items in each factorial structure.16 The results indicated that the 4-factor solution, in which all the items were retained, appeared to adequately represent the data.
Lastly, following the suggestion of Pedhazur and Schmelkin,18 we examined the 4-factor solution and con- firmed the meaningful interpretation for these factors. The 4 factors, which accounted for 70.45% of the total variance, were named as ‘autonomic symptoms’, ‘craving’, ‘gastro- intestinal symptoms’ and ‘negative affect’. The symptoms were generally consistent with the nominal labels of respec- tive factors. The corresponding items, loadings, eigenvalue, percent of variance, and descriptive data are presented in Table 4.
For the OOWS, factor analyses with the above similar stringent procedure for SOWS were conducted. Four factors initially emerged with eigenvalues greater than one. Results of the structural stability analyses indicated that the single-factor solution had 12 items with factor loadings greater than 0.53, whereas all the other factor so- lutions contained 9 items only. Also, the results of the inter- pretability analyses showed that other factorial structures were relatively less well defined and interpretable. Finally, we decided that the sole-factor solution should be optimal for OOWS. The single factor, which was labelled as ‘perceived symptoms’, accounted for 32.24% of the total variance. The results of the factor loadings are reported in Table 5.
The results indicated that correlation between the revised SOWS and OOWS in our sample was non-significant (0.169, p > 0.05).
Study 2
Sixteen Chinese patients with DSM-IV diagnoses of opioid dependence admitted to Kwai Chung Hospital for detoxification treatment were recruited into the study. Their mean age was 34.40 (standard deviation [SD], 10.84); there were 8 men and 8 women. Approximately 37.5% of the patients were working, 43.8% unemployed, 12.5% receiving public assistance, and 6.3% were missing these data. Their average duration of opiate use was 15.31 years (SD, 8.86).
Detoxification Procedure
In the opioid detoxification programme, methadone was used to reduce withdrawal symptoms and achieve abstinence. To measure the withdrawal symptoms in a standardised schedule, the revised SOWS and OOWS were administered at 4 specified time points in a 14-day period. Since some patients entering the programme had already been replac- ing methadone for opiates, the amount of methadone consumption for detoxification at the first day of the methadone programme differed between the participants. Regardless of the amount of methadone consumption on the day of admission, methadone 20 mg was recorded as the detoxification baseline or day 1 (time 1) — the third day was recorded as day 3 (time 2), the seventh day as day 7 (time 3), the fourteenth day as day 14 (time 4). From days 1 to 7, daily methadone consumption was gradually reduced from 20 mg to 0 mg, and remained at 0 mg in the following week before discharge.
When patients were completing the revised SOWS, a research assistant clarified any questions. The observers were 2 registered psychiatric nurses familiar with opiate with- drawal symptoms. To minimise the observers’ bias in checking OOWS, observers would receive standardised instructions for rating before the observation.
As initial t tests indicated no sex differences in the scores of both the revised SOWS and OOWS, data for men and women were combined in all subsequent statistical analyses. The purpose of the study was to examine the predictive validity* of the scales by comparing their respective scores measured over different points of time. Given the nature of gradual diminishing properties of withdrawal signs and symptoms shown in previous similar programmes, it was predicted that the scores of the revised SOWS and OOWS would be gradually decreasing in the initial stage.15 Due to the absence of methadone for patients from days 8 to 14, withdrawal symptoms were predicted to be stabilised and still present at the last 2 ratings.
Results
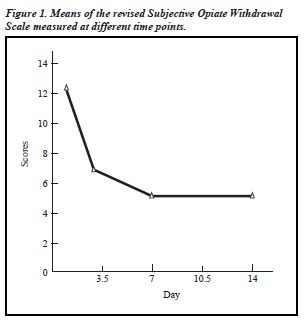
Figures 1 and 2 present the means of the 2 rating scales across different time points. The findings could be summarised as follows. Firstly, the revised SOWS had an anticipated trend of decline in scores from day 1 to day 14, whereas the OOWS had only an initial decline of scores from day 1 and remained relatively stable afterwards. Secondly, consistent with expectations, some residual symp- toms were present in both scales at the last rating. Thirdly, as expected for both the revised SOWS and OOWS, scores at day 7 and day 14 remained constant. Table 6 presents the paired t test values of the 2 scales at different times. There were significant differences between the day 1 revised SOWS scores and those at days 7 and 14, whereas there was no statistically significant change among the paired comparisons for the OOWS.
To evaluate specific changes in scores detected over time, paired t tests among factors of revised SOWS were subsequently performed. A trend of non-significant reduction was revealed between day 1 autonomic symptom scores with those at days 3, 7, and 14 (p < 0.09). The scores for gas- trointestinal symptoms at day 1 were also slightly lower than those for day 7 (p < 0.08).
Discussion
This study aimed to investigate the psychometric properties and factor structures of the revised SOWS and OOWS among local Chinese opiate addicts. A major caveat needs to be addressed here before interpreting the results. It may be argued that some important reliability indices such as the inter-rater and test-retest indices were not included and therefore the reliability of the scales should be challenged. However, the satisfactory reliabilities of the revised SOWS constant scores measured across times, whereas sensitive opiate withdrawal scales denote a changing pattern of symp- toms found at different times. An obtained coefficient of test-retest reliability is therefore confounded by the nature of changing of withdrawal symptoms.
Several findings should be highlighted in view of the present findings. Firstly, the factor structure of the revised SOWS indicates the presence of multiple factors of opiate withdrawal symptoms during detoxification. These factors not only reinforce the concept of multiple domains or structural validity of opiate withdrawal features,8 but also generate an insight in the design of future detoxification treatment. For instance, in the study 2 methadone detoxi- fication programme, the factors autonomic symptoms and gastrointestinal symptoms tended to have a quicker reduc- tion in scores.* In contrast, the scores of the factors negative affect and craving are slower to respond to the methadone detoxification. Alternative drug treatment or psychological treatment may be considered useful to alleviate these factors’ scores in the process. Consistent with this assertion, intervent- ions that include contingent reinforcement for opiate-free urines may be effective in reducing opiate drug use among patients during methadone withdrawal treatment.20 One plausible explanation for the mechanism is that an inclusion of the behavioural components such as reinforcers may reduce the negative affect scores or distract the craving effects. Hence, withdrawal symptoms could be much more effectively controlled during the process. Future empirical investigations in this area can illuminate the validity of this assertion.
* Although one might argue against the level of significance being set too lenient (p < 0.1), one should note that the small sample size of study
2 should have compromised the power and simultaneously increased the chance of a type II error. The option for a lenient significance p value is a balance of the trade-off.19
While most of the items in the revised SOWS have been meaningfully categorised under the umbrella of correspond- ing factors, the item diarrhoea appears not to fit well with the factor craving. One explanation may be related to the inadequate relevant items in the pool, a condition that allows less theoretically similar items being grouped together due to statistical rather than conceptual relevance.21 In the present analyses, this factor has been reliably reproduced under dif- ferent factor structures (including the 3-factor, 4-factor, and 5-factor models), and the item ‘craving for an opioid’ con- sistently bears the highest factor loading. This finding indicates that this factor tends to be a robust factor distinct from others. Theoretically speaking, the factor craving may consist of different kinds of craving such as affective, behavioural, cognitive, and sensory cravings.22 We specu- late that craving can be an important factor of withdrawal symptoms and that new items such as affective, behavioural, and cognitive cravings can be added. We suggest that future research can re-examine the factor structure of the revised SOWS if additional items of craving are incorporated.
Interestingly, factor analyses results of the OOWS indicate that the single solution factor model can explain the and OOWS shown by the item-total correlations and a co-efficients argue against this point. Furthermore, test-retest reliability may be a conceptually blurred psychometric in- dicator in the opiate withdrawal measures. This is because good test-retest reliability usually implies the presence of data well. Because the OOWS is checked by observers rather than by the addicted, the findings may merely reflect the observers’ perception of a single factor accounting for the withdrawal symptoms. The results are consistent with the notion that although observation is less intuitive in the data- collecting process, observers may be relatively less sensi- tive to discriminate and identify withdrawal factors than the individuals themselves.9,23,24
Although the results of study 2 generally support the anticipated trend of withdrawal symptoms measured by both scales, the revised SOWS appears to be relatively sensi- tive to such a gradual change.8 In the original work by Handelsman et al,8 their reported scores (on admission, mean, 2.0; SD, 0.4; after methadone, mean, 0.9; SD, 0.2) are highly similar to ours.
Taken together, these findings point to the fact that the OOWS is relatively less sensitive in measuring withdrawal symptoms among patients undergoing methadone detoxification programmes. Such an insensitivity can be explained by a number of previous studies in which objective withdrawal symptoms could only be observed at a very high level of distress.9,23,25 These findings appear valuable to clinicians and future researchers. For instance, in a drug treatment research design where adequate control of withdrawal symptoms is anticipated, researchers may be inclined to choose the SOWS rather than the OOWS to measure the withdrawal symptoms. On the other hand, in a highly distressing withdrawal condition where a subjective rating may be difficult to conduct, the OOWS could be a better option.
The low correlation (0.169, p > 0.05) between the revised SOWS and OOWS in this study lends support to previous findings that the OOWS and SOWS are scales designed to assess different aspects of opiate withdrawal features.23 Therefore, patients undergoing methadone detoxi- fication programmes may not present with severe observ- able withdrawal symptoms easily discerned by others. Consequently, the insensitivity of observing withdrawal symptoms at moderate or low levels of distress explains why the correlations between subjective measures and observed ratings of withdrawal symptoms have been reliably found to be low.9,23,25
In sum, the Chinese versions of the revised SOWS and OOWS enjoy satisfactory psychometric properties. Results of factor analyses show that the revised SOWS is composed of 4 meaningful factors, whereas the OOWS has 1 general opiate withdrawal factor. Findings also indicate that the revised SOWS is relatively more sensitive for measuring the changes of opiate withdrawal symptoms than the OOWS in the present methadone detoxification programme.
Acknowledgements
We would like to thank Ho Kwok Hung, Eunice Lai, Pak Chui Sau, and Francis Tsui for their help with this project. In addition, we are grateful to the valuable comments of 2 anonymous reviewers.
References
- Narcotics Division, Hong Kong Government. Central Registry of Drug Abuse: Drug statistics. 2001. http://www.info.gov.hk/nd/stat/index.htm.
- National Institute on Drug Abuse. Principles of drug addiction treatment: a research-based guide. National Institute on Drug Abuse, National Institutes of Health; 1999. NIH Publication No. 99-4180. http://www.drugabuse.gov/PDF/PODAT/PODAT.pdf
- O’Brien CP, Testa T, O’Brien TJ, Brady JP, Wells B. Conditioned narcotic withdrawal in humans. Science 1977;195:1000-1002.
- Wikler A. Opioid dependence: mechanisms and treatment. New York: Plenum; 1980.
- Brewer C. Ultra-rapid, antagonist-precipitated opiate detoxification under general anesthesia or sedation. Addict Biol 1997;2/3:291-302.
- Hensel M, Kox WJ. Safety, efficacy, and long-term results of a modi- fied version of rapid opiate detoxification under general anaethesia: a prospective study in methadone, heroin, codeine and morphine addicts. Acta Anaesthesiol Scand 2000:44:326-333.
- Stephenson J. Experts debate merits of 1-day opiate detoxification un- der anesthesia. JAMA 1997;277:363-364.
- Handelsman L, Cochrane KL, Aronson MJ, Ness R, Rubinstein KJ, Kanof PD. Two new rating scales for opiate withdrawal. Am J Drug Alcohol Abuse 1987;13:293-308.
- Loimer N, Linzmayer L, Grünberger J. Comparison between observer assessment and self-rating of withdrawal distress during opiate detoxification. Drug Alcohol Depend 1991;28:265-268.
- 10. Haertzen CA. Addiction Research Center Inventory: Development of a general drug estimation scale. J Nerv Ment Dis 1965;141:300-307.
- Himmelsbach CK. The morphine abstinence syndrome, its nature and treatment. Ann Intern Med 1941;15:829-839.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association; 1994.
- 13. World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
- Bradley BP, Gossop M, Philips GT, Legarda JJ. The development of an opiate withdrawal scale (OWS). Br J Addiction 1987;82:1139-1142.
- Gossop M, Griffiths P, Bradley B, Strang J. Opiate withdrawal symp- toms in response to 10-day and 21-day methadone withdrawal programmes. Br J Psychiatry 1989;154:360-363.
- Comrey AL, Lee BH. A first course in factor analysis. 2nd ed. New Jersey: Erlbaum; 1992.
- Cattell RB. The meaning and strategic use of factor analysis. In: Cattell RB, editor. Handbook of multivariate experimental psychology. Chicago: Rand McNally; 1966:174-243.
- Pedhazur EJ, Schmelkin LP. Measurement, design, and analysis: an integrated approach. London: LEA; 1991.
- Stevens J. Applied multivariate statistics for the social sciences. 3rd ed. New Jersey: LEA; 1996.
- 20. Stitzer ML, Bigelow GE, Liebson IA, McCaul ME. Contingency man- agement of supplemental drug use during methadone maintenance treat- ment in behavioral intervention techniques in drug abuse treatment. In: J Grabowski, ML Stitzer, JE Henningfield, editors. NIDA research monograph 46. Washington: NIDA; 1984.
- 21. Tabachnick BG, Fidell LS. Using multivariate statistics. 3rd ed. New York: Harper Collins; 1996.
- Sayette MA, Shiffman S, Tiffancy ST, Niaura RS, Martin CS, Shadel
- WG. The measurement of drug craving. Addiction 2000;95 (Suppl): 189-210.
- Isbell H, Vogel VH. Addiction liability of methadone and its use in the treatment of the morphine abstinent syndrome. Am J Psychiatry 1948; 105:909.
- Turkington D, Drummond DC. How should opiate withdrawal be measured? Drug Alcohol Depend 1989;24:151-153.
- Gossop M, Bradlley B, Strang J, Connell P. The clinical effectiveness of electrostimulation vs oral methadone in managing opiate withdrawal. Br J Psychiatry 1984;144:208.