Hong Kong J Psychiatry 2006;16:14-20
ORIGINAL ARTICLE
RMK Ng, MSL Cheung
Dr Roger MK Ng, MRCPsych (UK), FHKAM (Psychiatry), Department of Psychiatry, Kowloon Hospital, 147A, Argyle Street, Hong Kong, China.
Miss Martina SL Cheung, Clin Psych, Department of Psychiatry, Castle Peak Hospital, Hong Kong, China.
Address for correspondence: Dr Roger MK Ng, Department of Psychiatry, Kowloon Hospital, 147A, Argyle Street, Hong Kong, China.
Tel: (852) 3129 7111; Fax: (852) 2711 4601;
E-mail: ngmk@ha.org.hk
Submitted: 5 April 2006; Accepted: 5 July 2006
Abstract
Objective: To examine the efficacy of social skills training in Hong Kong Chinese patients with schizophrenia.
Patients and Methods: Thirty six hospital inpatients with residual schizophrenia were randomised to receive either social skills training (n = 18) or supportive group discussion (n = 18) for 30 hours in group-format of 2 sessions per week for 8 weeks.
Results: There was no improvement in symptoms or social functioning after completion of either social skills training or supportive group discussion. There was also no difference between the 2 groups in terms of symptoms or social functioning. The relapse rate was similar across the 2 groups.
Conclusion: Social skills training is not an effective psychosocial intervention for patients with chronic schizophrenia in Hong Kong.
Key words: Schizophrenia, Social adjustment, Social behaviour
Introduction
Social skills training (SST) has been used to improve the social skills and social functioning of patients with schizo- phrenia. The literature generally supports that patients with schizophrenia can acquire social skills through SST, includ- ing simple and complex social behaviour.1-4
Despite the apparent evidence for the efficacy of SST for improving social skills in patients with chronic schizophrenia, many unanswered questions remain. Most studies primarily recruited men, because these studies were conducted in veterans hospitals3; the results may not be readily generalisable to women. Furthermore, a meta-analysis showed that effect size was dependent on the type of out- come measure.4 Effect size was substantially smaller when the assessment was conducted outside the treatment setting or differed in form or content from the training exercises. Meta-analyses have also found that inpatients and severely ill patients benefited less from SST.3,4 In a recent meta- analysis with stringent selection criteria of randomised controlled studies, the conclusion was significantly differ- ent from previous reviews; there was no clear evidence for any benefits of SST on global functioning, social functioning, relapse rate, quality of life, or treatment compliance.5 There is a paucity of randomised studies of SST among the Chinese population. At the time of writing, only 3 studies had been performed in a Chinese population (1 in China,6 1 in Hong Kong,7 and 1 in Taiwan8). A recent randomised pilot study found that inpatients with schizophrenia receiving 8 weekly 3-hour sessions of SST had significant improvement in social behaviour as measured by the Social Behaviour Schedule (SBS).9,10 The training had little effect on negative symptoms, which were usually more enduring and resistant to such a brief psychosocial intervention. The therapist time was not controlled and the sample size was small (n = 14). Following the encouraging results of the pilot study, the current study was an attempt to investigate the efficacy of SST with a methodologically rigorous study.
The objectives of this research were to:
- test whether SST is effective in improving the social functioning and social skills of Chinese patients with chronic schizophrenia
- investigate whether SST is more effective than other types of group treatment (i.e., supportive group discussion for the purposes of this study)
- investigate whether the effect of SST, if any, can be maintained
- test whether SST can reduce/avert relapses in comparison with supportive group discussion.
Patients and Methods
Patients
This was a single-centre prospective rater-masked ran- domised controlled trial with a 6-month follow-up period. Eligible patients were randomly allocated to 1 of 2 treat- ments: SST and usual treatment or supportive group discussion and usual treatment. Patients were assessed for social functioning, psychopathology, and relapse before and after the treatment phase (8-week period). Patients were then followed up and assessed through psychiatric interview and examination of case notes 6 months after completion of treatment. It was predicted that the group receiving SST would show better social skills and global functioning after treatment and at 6 months, and a reduced rate of relapse and readmission to hospital.
Participants were recruited over 6 months from a rehabili- tation ward specialising in rehabilitation of chronic psychi- atric inpatients. Due to the admission policy of the ward, the age range of the patients was 18 to 65 years. Written consent was obtained from all patients.
Inclusion criteria were as follows:
- Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) criteria of schizophrenia, defined by the Structured Clinical Interview for DSM-IV Diagnosis (SCID-Clinical Version)11
- intelligence quotient of 70 or above (verified by the National Adult Reading Test)12
- no organic central nervous system disorder or history of substance misuse in the previous 12 months.
Potentially eligible patients were screened at admission to the rehabilitation ward by an experienced psychiatrist and baseline assessments and demographic data were recorded. Independent concealed randomisation of patients with minimisation was performed using a random number table. Stratification was undertaken with the following variables: male or female, use of typical or atypical antipsychotics (clozapine, risperidone, and olanzapine), and duration of hospital stay (>1 year or <1 year).
Assessment and Reliability
Two ratings of symptoms were used as outcome measures at baseline, 4 and 8 weeks (post-treatment), and 6 months after completion of treatment — the expanded Brief Psychi- atric Rating Scale (BPRS) total and subscale scores13 and the Scale of the Assessment of Negative Symptoms (SANS).14 Good reliability between the blinded psychiatric rater and the psychiatrist was established using videotaped interviews. Pearson's correlation coefficients (PC) for BPRS scores were 0.85-0.89 for psychotic symptoms, 0.66-0.73 for manic symptoms, 0.72-0.83 for depressive symptoms, 0.66-0.87 for other symptoms, and 0.77-0.82 for total scores. For SANS, the PCs were 0.66-0.75 for affective flattening, 0.65-0.69 for alogia, 0.64-0.72 for avolition-apathy, 0.67- 0.73 for anhedonia-asociality, 0.65-0.68 for attention, and 0.66-0.77 for total scores.
Thirty percent of the videotapes of the BPRS and SANS ratings at baseline, post-treatment, and 6 months follow- up were randomly selected for a reliability check by the psychiatrist. The inter-rater reliability between the psychi- atrist and the psychiatric rater was good (PC for BPRS, 0.77-0.89; PC for SANS, 0.69-0.74).
Two measures of general social functioning and 1 behav- ioural measure of social skills were used as primary out- come measures — the SBS10 and Social Functioning Scale (SFS)15 as general social functioning measures, and the Role Play Test (RPT) of the Social Problem Solving and Assessment Battery16 as a behavioural measure. The SFS, SBS and RPT were administered at week 0, week 8, and month 6, as social functioning measures may take time to demonstrate change after intervention.
Both the SBS and SFS were validated in the rehabil- itation ward (SBS has a split-half internal reliability of 0.75 and inter-rater reliability of k = 0.77; SFS has a split- half reliability of 0.78 and test-retest reliability of k = 0.62). Use of the SFS would test whether SST was therapeutically beneficial for broader behavioural domains and functional contexts.4 The SBS covers 21 behaviour areas such as destructive behaviours, personal appearance, and hygiene. Most of the items were rated on a 5-point scale by a rater who interviewed a close informant of the participants. The severe behaviour problem score was derived to indicate the severity of patients' problems. In this study, the inter-rater reliability between the psychiatric rater and the psychiatrist for the severe behaviour problem score was good (k = 0.88); there was also good internal consistency (Cronbach's a = 0.76). For patients in hospital during the trial period, the informant was the key nurse (defined as the care nurse with at least 3 months of close contact). For patients who had been discharged to the community, the informant was either a family member living with the patient or the key hostel staff with contact for at least 3 months. The SFS is an 81-item self-administered questionnaire covering several behaviour areas such as social engagement/withdrawal and pro-social activities.
For the RPT, patients were asked to listen to 6 scenarios of social interactions from an audiotape (3 were interaction skills with strangers and 3 were self-assertiveness skills). To enhance comprehension and retention of the material, the scenarios were also written on cards for patients to read while listening to the scenarios. There were also 2 trial rehearsal scenarios before the actual test for warm-up and check of comprehension. The patients were required to perform in the particular role as instructed in the audiotape, while the research assistant would play the other role to facilitate the social interaction. All the role-play scenarios were videotaped and rated separately by the blinded raters. The social skills were rated on 3 aspects: content of conversation, paralinguistic behaviour, and effectiveness of the conversation. The 3 aspects were rated according to each patient's verbal and non-verbal behaviours. Inter-rater reli- ability of the RPT between another 2 independent blinded psychiatric raters (different from the rater for BPRS, SANS, SBS) was good (k = 0.89 for scale of content, k = 0.92 for scale of paralinguistic behaviour, and k = 0.85 for scale of effectiveness).
Patients were assessed pretreatment, post-treatment, and 6 months after treatment for relapse and readmission. The hospital charts and case notes of all participants were studied and examined for evidence of relapse by the psychiatrist, using a method devised by Barrowclough et al.17 Relapses were defined as an exacerbation of psychotic symptoms lasting longer than 1 week and leading to a change in patient management, as recorded in the hospital charts. Readmission data were also available in the case notes. This approach was supplemented by interview-based evidence of relapse conducted in the 3 assessment interviews by the psychiatric rater, as recommended by Nuechterlein et al.18 Psychotic relapse was defined as 6 or 7 on the BPRS scales for hallucinations, unusual thought content, or conceptual disorganisation; non-psychotic relapse was defined as 6 or 7 on the scales for bizarre behaviour, self-neglect, hostility, depression, or suicidality.18 These sensitive criteria were chosen because none of the participants had a baseline rat- ing of 6 to 7 in the subscores.
Verbal memory was assessed with the Rey Auditory Verbal Learning Test,19 Chinese version (Neuropsychology Laboratory, Department of Psychology, The University of Hong Kong). Executive functioning was assessed with the Wisconsin Card Sorting Test.20 Early sensory processing was measured by degraded-stimuli Continuous Performance Test.21 These measures were administered once at recruit- ment as neurocognitive measures were found to be a rate- limiting factor for acquisition of skills.22
Subjective satisfaction with the therapists and the treat- ment modality was assessed after 8 weeks with a self-rating scale that covered the following areas: skills of the therapist, usefulness of the topics covered, and format of the treat- ment group. Each area was assessed with a 5-point Likert scale ranging from very satisfied (5) to very unsatisfied (0).
Therapeutic Interventions
The interventions were carried out independently of the raters, who were unaware of the treatment allocation. Rou- tine nursing care and other rehabilitation programmes (self- care training, psycho-education and leisure programmes) were the same for the 2 groups. There is no evidence that the programmes reduce relapse or improve social functioning.23
SST was devised by an experienced clinical psycholo- gist and was based on a widely adopted manual of SST.24 The SST was conducted by 2 experienced nurse therapists, who had conducted more than 10 groups of SST in the previ- ous 4 years. An experienced clinical psychologist supervised the 2 nurse therapists throughout the trial. The delivery was designed to provide 30 to 32 hours of treatment within 8 weeks (2 sessions per week, with each session lasting for 1.5 to 2 hours). SST was conducted according to an infor- mation processing model,25 which included training in re- ceiving skills (to read the situation), processing skills (to think about a response), and sending skills (to act out the response). Behavioural techniques were emphasised, includ- ing instruction, taped modelling, role-play practice, verbal feedback, social reinforcement, coaching, prompting, and homework assignment.
Supportive group discussion was used as a comparison intervention to control for non-specific elements of therapist exposure. The intervention was therefore delivered in the same 8-week format (2 sessions per week, with each ses- sion lasting for 1.5 to 2 hours). Discussion topics included practical tips on money management and information on application for social security allowances. Special attention was paid to avoiding discussion on interpersonal skills is- sues and use of behavioural techniques. Supportive group discussion was also supervised by the clinical psychologist and conducted by the 2 nurse therapists. All SST sessions and discussion groups were videotaped. Half of the tapes were randomly selected and viewed by 2 independent raters who were required to classify them as SST or sup- portive group discussion sessions, and to rate the quality of therapy on the Benton and Schroeder criterion list.2
Medication was kept constant during the treatment period, except when patients were diagnosed clinically as having relapsed. Patients were withdrawn from the trial while in relapse and the medication dose was adjusted. Once they had been recruited into the trial, patients who relapsed were considered as treatment failures in the intention-to- treat analysis. At the 6-month follow-up, the medication dose and type were recorded. Adherence in the ward was assessed by daily nurse supervision and compliance in the community was assessed by each patient's verbal report as a dichotomous measure of 'regular' or 'irregular' medi- cation adherence. The verbal report was supplemented by examination of the medical notes or hospital records for non-adherence.
Treatment Exposure and Fidelity of Interventions
The number of sessions was similar in the SST group (16 sessions) and the supportive group discussion (16 sessions). Thirty six patients entered the trial, 18 in each group. The mean number of therapy sessions was similar in the SST group (mean, 13.8 sessions) and supportive discussion group (mean, 15.3 sessions). Three participants allocated to SST and 2 allocated to supportive group discussion dropped out before completion of the trial. For treatment fidelity, agreement between the 2 independent raters was good. Quality of SST was assessed to be good, with a mean of 6.9 for core behavioural techniques specified in the Benton and Schroeder criteria.2 The absence of such techniques was also confirmed in the supportive group discussion (mean, 0.9). Raters correctly classified all the session tapes in terms of the appropriate therapy.
Concealment of Allocation
Randomisation was done by an administrator, independent of both the raters and the therapists. The administrator was only aware of the code number, name, date of birth, and stratification criteria of each patient. Therapists and raters were not permitted to communicate details about the patients. Clinical staff were not aware of the treatment allocation so as to minimise allocation bias for providing a rating for the SBS.10 Data storage and management were kept separate. Patients were also instructed not to divulge details of their treatment to the raters.
Statistical Analysis
All analyses were carried out using the Statistical Package for the Social Sciences (SPSS) software (Version 11; SPSS, Chicago, IL, USA). Analyses of outcome were performed on an intention-to-treat basis. All patients who relapsed and were withdrawn from the trial during the treatment phase were included as treatment failures. All missing data were given mean values of that particular variable at that parti- cular assessment point. Data were first subject to the Kolmogorov-Smirnov test for normality before parametric tests were employed. Baseline differences in symptom scores, social functioning scores, and neurocognitive mea- sures were obtained through the use of analysis of variance. Repeated measures analysis of covariance (ANCOVA), after allowing for relevant baseline scores, time of assessment, patient sex, duration of hospital stay, duration of illness, and verbal intelligence as covariates, was used to detect dif- ferences in the symptom scores, social functioning scores, and relapse data at any time point during the assessment.
Results
Recruitment and Follow-up
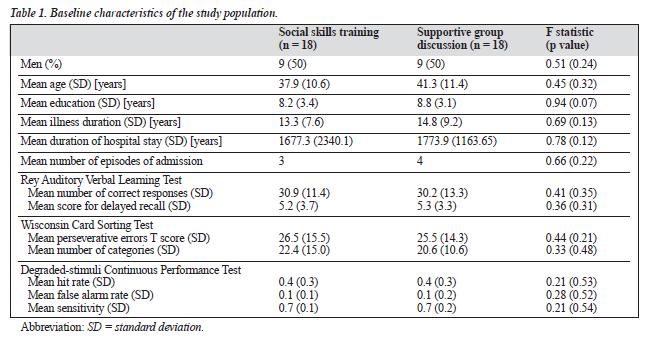
Initial identification and referral to the rehabilitation ward resulted in 64 patients being screened at interview. Of these, 40 patients met the eligibility criteria for study entry and 36 gave written informed consent. The patients were randomised within 3 days of giving consent. There were no significant differences between the consenting and non-consenting adults in age, sex, and duration of hospital stay. Forty percent of patients were detained as certified patients under the Mental Health Ordinance 1997. Baseline characteristics of the 2 treatment groups are given in Table 1. There were no signi- ficant differences in the baseline characteristics measured.
After 6 months, 35 patients were interviewed; of these 17 had received SST and 18 had received supportive dis- cussion. One participant receiving SST was lost to follow- up. Participant hospital data were available for assessment of duration of hospital stay for 35 patients and case notes were available for assessment for 35.
Social and Symptom Status
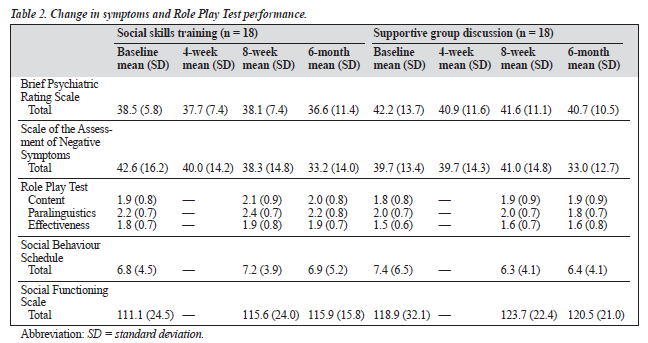
The SFS, BPRS, and SANS data were normally distributed. For the RPT and SBS, the data were normalised after loga- rithmic transformation. The data for the baseline, post- treatment, and 6-month follow-up assessments are presented in Table 2. Comparisons were made between the 2 treat- ment groups of scores for the RPT total, SFS total, SBS total, subscales and total of the BPRS, and the subscales and total of SANS, by means of repeated measures ANCOVA with relevant baseline score, sex, duration of hospital stay, duration of illness, and verbal intelligence as covariates (p > 0.05). Receipt of treatment did not improve outcomes as measured by RPT, SFS, SBS, BPRS, or SANS (p > 0.05). There were no significant differences between SST and supportive group discussion for social or symptom outcomes (p > 0.05).
Hospital Discharge, Relapse, and Readmission
Data were available for 35 patients for hospital admissions and for relapse. The rate of discharge at the 6-month follow- up was 5 of 17 patients for the SST group (29.4%) and 8 of 18 patients (44.4%) for the supportive discussion group. No patients were discharged between the pretreatment and post-treatment time points. The rates of readmission at 6 months were 1 of 5 patients (20%) for the SST group and 1 of 8 patients (12.5%) for the supportive discussion group. The rates of psychotic relapse were 4 of 5 patients for the SST group and 2 of 2 patients in the supportive dis- cussion group. There were no significant differences between the 2 groups in time to subsequent relapse, total duration of hospital stay due to relapse, or time spent in each relapse. However, there was a trend towards significance for more psychotic relapses for patients in the SST group at the post-treatment assessments (SST, 2/17 patients; supportive discussion group, 0/18 patients; p = 0.07). There were no non-psychotic relapses during the treatment phase or during the 6-month follow-up period.
Medication
Data for medication dose were available for 36 patients at baseline and the post-treatment time points. The mean value of daily antipsychotic dose (in chlorpromazine equivalents) at baseline was as follows: SST, 531.7 mg (standard deviation [SD], 362.1 mg); supportive discussion, 516.7 mg (SD, 204.2 mg). The mean value of daily benzhexol dose at baseline was as follows: SST, 2.00 mg (SD, 4.7 mg); sup- portive discussion, 1.56 mg (SD, 2.2 mg). There were no significant differences in benzhexol dose and antipsychotic dose between the SST and supportive discussion groups (p = 0.43). Nine patients in the SST group and 9 in the support- ive discussion group received atypical antipsychotics, as type of medication was one of the factors of stratification. The medication dose was adjusted for 2 patients in the SST group at the 8-week assessment, otherwise the medication for both groups remained the same.
The mean value of daily antipsychotic dose (in chlor- promazine equivalents) at 8 weeks was as follows: SST, 550.2 mg (SD, 354.3 mg); supportive discussion, 516.7 mg (SD, 204.2 mg). There were no significant differences be- tween the 2 groups in antipsychotic dose and benzhexol dose. The 2 patients who had relapsed at the 8-week assessment had an adjustment in the dose of conventional anti-psychotics. There was no change in the type of antipsychotics used during the 8-week treatment period.
Data for medication dose were available for 35 patients (97.2%) who completed the 6-month follow-up period. The mean daily medication dose (in chlorpromazine equivalents) was as follows: SST, 560.4 mg (SD, 360.3 mg); supportive discussion, 543.3 mg (SD, 223.6 mg). Generally, medica- tion adherence was good, with 34 of 35 patients reporting regular medication use. This was corroborated by reports of medical adherence and regular appointments in the medical notes. There were no significant differences between the 2 groups for any of the medication measures.
Satisfaction and Acceptability of Treatment
Both treatments were rated as highly satisfactory by the patients. There were no significant differences between the 2 groups in any of the areas covered in the satisfaction survey.
Discussion
The results of this study suggest that SST offers no advan- tages in terms of social functioning, relapse, or readmission compared with supportive group discussion. The results add some support to the conclusions from recent meta-analyses that SST has no benefit for inpatients with severe chronic schizophrenia4,5 and the recent 2003 National Institute for Clinical Excellence (NICE) guidelines, which suggest a lack of evidence of SST for patients with psychosis.26 There are some important differences between this study and other previous studies in Chinese and Western societies.
One important variable that might explain the lack of skill acquisition and generalisation may be related to the severity of the illness and the prominence of negative symp- toms in this study. Xu et al6 and Tsang and Pearson7 re- cruited outpatients and Chien et al8 recruited inpatients with comparatively less severe negative symptoms than the pa- tients in this study. This is the only local study that also provides data on neurocognitive functioning. These patients had a low vigilance level and low executive functioning, which might explain the lack of benefit of SST.22 Patients with schizophrenia with deficit syndrome were not res- ponsive to intensive SST, probably due to poorer cognitive functioning and a greater degree of neuroanatomical and neurobiological impairment.27
Another salient difference between this study and other studies demonstrating a treatment effect of SST is the in- tensity and duration of the treatment. Bustillo et al28 reviewed 18 studies and found that SST improved social adjustment in only 2 studies, both of which involved intensive training for a long duration (90 minutes twice weekly for 6 months, then weekly for 1.5 years in Marder et al's study29; 3 hours daily, 4 times a week for 6 months in Liberman et al's study30). In their summary of psychosocial intervention for schizophrenia supported by empirical evidence, Mueser and McGurk mentioned that SST takes several months to have an effect.31 Similarly, Bellack concluded that "several re- cent reviews of empirical supported treatments rated social skills training as no more than promising¼it may be neces- sary to employ longer-term treatments that extend into the community and that are integrated with an array of inter- vention strategies."32 This study only lasted for 8 weeks (90 minutes twice weekly for 8 weeks only), supporting Bellack's contention that SST of limited duration and in- tensity is not effective for improving social skills in patients with schizophrenia.32 This study might stimulate more in- depth research into the routine hospital practice of conduct- ing SST of short duration and low intensity for inpatients with schizophrenia.
Contrary to the study hypothesis, there is no difference between the effects of SST and supportive group discussion in social outcome. Direct comparison with other published Chinese studies is difficult, as populations and therapeutic aims differ. Xu et al6 and Tsang and Pearson7 investigated the efficacy of specific life skills training in outpatients with schizophrenia (work-related social skills; medication management). Such highly focused modular training was reported to have a better chance of skill generalisation in outpatients.4,23 This inpatient study focused on traditional social skills that emphasised conversational and assertiveness skills in daily events, which more closely resembled the Taiwanese inpatient study.8 However, Chien et al's study was not a controlled trial and only used subjective measures of social competence.8 Furthermore, this study was the first Chinese study of SST in inpatients with schizophrenia that controlled for important confounding variables such as baseline psychopathology, neurocognitive functions, and medication effects.
Several reviews have shown that patients have improved social skills, especially in role-play situations, after SST.2,3,33 For studies with positive effect on behavioural tests, the content and form of the behavioural tests resembled SST.4 How- ever, there is uncertainty about real improvement in social skills when evaluated with role-plays of novel situations. The failure of skills generalisation to the community setting is documented in several reviews and meta-analyses.5,33,34 In the current study, SST had no effect on role-play tests. This might be explained by the lack of generalisation of SST to other role-play situations. Furthermore, when those patients discharged to the community after 6 months were examined for behavioural outcome, there was no improvement. This might highlight the importance of teaching community survival skills in the community, where practice and reinforcement are readily available.35
Contrary to the study hypothesis, there was no reduc- tion in relapse rates for patients who received SST; in fact there was a trend towards significance that patients receiv- ing SST were more likely to experience a relapse. This in- crease could not be explained by medication adherence as both groups had similar adherence rates. The lack of ben- efit on the relapse and readmission rates was consistent with previous reviews and meta-analyses.5,34 Whether the risk of relapse for these patients increased with intensive SST war- rants further investigation. However, the concept of cogni- tive stress triggering relapse in highly vulnerable psychotic patients is not new.36 Excessive environmental stress, such as that experienced by the demands of learning SST, could accumulate and overcome the ability to cope, leading to the recurrence of psychotic symptoms.
The major limitation of this study was that it had a small sample size. A priori power calculation was not performed, so the conclusion regarding the lack of efficacy of SST can best be viewed as tentative. The relatively short follow-up is another limitation. Furthermore, the measure of medica- tion adherence was based on patients' verbal reports and scrutiny of medical notes. Use of a dimensional measure rather than a dichotomous one and pill count might increase the sensitivity of detecting medication non-adherence.
Acknowledgements
The authors would like to thank Miss ML Lee and Mr HW Leung as the nurse therapists who conducted the trial. They would also like to express sincere thanks to Dr SP Leung, Consultant Psychiatrist, Castle Peak Hospital, for support- ing the trial.
References
- Bellack AS, Mueser KT. Psychosocial treatment for schizophrenia. Schizophr Bull. 1993;19:317-36.
- Benton MK, Schroeder HE. Social skill training with schizophrenics: a meta-analytic evaluation. J Consult Clin Psychol. 1990;58:741-47.
- Corrigan PW. Social skills training in adult psychiatric populations: A meta-analysis. J Behav Ther Exper Psychiatry. 1990;22:203-10.
- Dilk MN, Bond GR. Meta-analytic evaluation of skills training research for individuals with severe mental illness. J Consult Clin Psychol. 1996; 64:1337-46.
- Pilling S, Bebbington P, Kuipers E, et al. Psychological treatments in schizophrenia: II. Meta-analyses of randomized controlled trials of social skills training and cognitive remediation. Psychol Med. 2002; 32:783-91.
- Xu Z, Weng Y, Hou Y. Efficacy and follow-up of research of medica- tion management module training for schizophrenic patients in Beijing. Chin J Psychiatry. 1999;32:96-9.
- Tsang H, Pearson V. A work-related social skills training for people with schizophrenia in Hong Kong. Schizophr Bull. 2001;27:139-48.
- Chien HC, Ku CH, Lu RB, et al. Effects of social skills training on improving social skills of patients with schizophrenia. Arch Psychiatr Nurs. 2003;5:228-36.
- Chan J, Ng R, Ng K, Kan F. A controlled study on the efficacy of social skills training. In: Annual Report: Hospital Pre-discharge Unit. Hong Kong: Castle Peak Hospital; 1996-1997:10-13.
- Wykes T, Sturt E. The measurement of social behaviour in psychiatric patients: an assessment of reliability and validity of the SBS schedule. Br J Psychiatry. 1986;148:1-11.
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical In- terview for DSM-IV. New York: Biometrics Research Department, New York State Psychiatric Institute; 1997.
- Nelson HE. The national adult reading test. Windsor, UK: NFER- NELSON;1982.
- Lukoff D, Liberman RP, Nuechterlein KH. Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophr Bull. 1986;12: 578-602.
- Andreasen NC. Modified Scale for the Assessment of Negative Symp- toms (SANS). Iowa City: University of Iowa;1986.
- Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The so- cial functioning scale: the development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853-59.
- Donahoe CP Jr, Driesenga SA. A review of social skills training with chronic mental patients. In: Hersen M, Risler RM, Miller PM, editors. Progress in behaviour modification. Vol 23. Newbury Park: Sage Publications; 1988:131-64.
- Barrowclough C, Tarrier N, Lewis S. Randomised controlled effective- ness trial of needs-based psychosocial intervention service for carers of people with schizophrenia. Br J Psychiatry. 1999;174:505-11.
- Nuechterlein KH, Dawson ME, Gitlin M. Developmental processes in schizophrenic disorders: longitudinal studies of vulnerability and stress. Schizophr Bull. 1992;18:387-425.
- Lezak MD. Neuropsychological assessment. 2nd ed. New York: Oxford University Press;1983.
- Heaton RK. The Wisconsin Card Sorting Test manual. Odessa: Psychological Assessment Resources;1981.
- Nuechterlein KH, Dawson ME, Green MF. Information-processing abnormalities as neuropsychological vulnerability indicators of schizophrenia. Acta Psychiatr Scand. 1994;90(Suppl):71-9.
- Bowen L, Wallace CJ, Glynn SM, Nuechterlein KH, Lutzger JR, Kuehnel TG. Schizophrenic individuals' cognitive functioning and performance in interpersonal interactions and skills training procedures. J Psychiatr Res. 1994;28:289-301.
- Huxley N, Rendall M, Sederer M. Psychosocial treatments in schizophrenia: a review of the past 20 years. J Nerv Ment Dis. 2000; 188:187-201.
- Bellack AS, Mueser KT, Gingerich S, Agresta J. Social skills train- ing for schizophrenia: a step-by-step guide. New York: Guilford Press; 1986.
- Wallace CJ, Nelson CJ, Liberman RP, et al. A review and critique of social skills training with schizophrenic patients. Schizophr Bull. 1980; 6:42-63.
- NICE guidelines: psychological management of schizophrenia. London: Department of Health;2003.
- Kopelowicz A, Corrigan PW, Schade M, Liberman RP. Social skills training. In: Mueser KT, Tarrier N, editors. Handbook of social func- tioning in schizophrenia. Boston: Allyn & Bacon;1998:307-26.
- Bustillo JR, Lauriello J, Horan WP, Keith SJ. The psychosocial treat- ment of schizophrenia: an update. Am J Psychiatry. 2001;158:163-75.
- Marder SR, Wirshing WC, Mintz J, et al. Two-year outcome of social skills training and group psychotherapy for out-patients with schizophrenia. Am J Psychiatry. 1996;153:1585-92.
- Liberman RP, Wallace CJ, Blackwell G, Kopelowicz A, Vaccaro JV, Mintz J. Skills training versus psychosocial occupational therapy for persons with persistent schizophrenia. Am J Psychiatry. 1998;155: 1087-91.
- Mueser KT, McGurk SR. Schizophrenia. Lancet. 2004;363:2063-71.
- Bellack AS. Rehabilitative treatment of schizophrenia. In: Lieberman JA, Murray RM, editors. Comprehensive care of schizophrenia. London: Martin Dunitz; 2001:109-20.
- Penn DL, Mueser KT. Research update on the psychosocial treatment of schizophrenia. Am J Psychiatry. 1996;153:607-17.
- Lawrie SM. Schizophrenia. Clin Evidence. 2000;3:475-85.
- Test MA. Training in community living. In: Liberman RP, editor. Handbook of psychiatric rehabilitation. Boston: Allyn & Bacon; 1992:153-70.
- Lukoff D, Ventura J, Nuechterlein K, Liberman RP. Integrating symp- tom assessment into psychiatric rehabilitation. In: Liberman RP, editor. Hand-book of psychiatric rehabilitation. Boston: Allyn & Bacon;1992.