Hong Kong J Psychiatry 2007;17:75-80
ORIGINAL ARTICLE
Dr David YK Lau, MRCPsych, FHKCPsych, FHKAM (Psychiatry), St. Paul’s Hospital, 2 Eastern Hospital Road, Causeway Bay, Hong Kong, China.
Dr Alfred HT Pang, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Tai Po Hospital, 9 Chuen On Road, Tai Po, Hong Kong, China.
Address for correspondence: Dr David YK Lau, Suite 1802, 18/F, East Point Centre, 555 Hennessy Road, Causeway Bay, Hong Kong, China.
Tel: (852) 3586 9881; Fax: (852) 3568 9882;
E-mail: drdavidlau@yahoo.com.hk
Submitted: 21 May 2007; Accepted: 4 July 2007
Abstract
Objectives: To examine the appraisal of caregiving experience by relatives of patients suffering from severe mental disorders.
Participants and Methods: Relatives of patients suffering from major psychiatric disorders were assessed with the Chinese version of the Experience of Caregiving Inventory. Clinical correlates of the appraisal of caregiving were evaluated with the Brief Psychiatric Rating Scale, Scale for the Assessment of Negative Symptoms, and the Mastery Scale.
Results: A total of 81 patients and 129 caregivers were recruited. There was a positive correlation between positive and negative appraisals as measured by the Experience of Caregiving Inventory (r = 0.32, p = 0.003). Positive psychotic and depressive symptoms did not show any significant relationship with the Experience of Care giving Inventory scores. A regression analysis of the Experience of Care giving Inventory scores (n = 81) showed that negative appraisal was influenced by the Global Assessment of Functioning 1 year before index admission and the educational levels of the caregivers, while positive appraisal was associated with the employment status of patients and the educational levels of the caregivers.
Conclusions: The caregiving experience is affected by different factors. Interventions for caregivers should focus on the specific needs of the families using a multi-dimensional perspective.
Key words: Caregivers; Family health; Mental disorders; Stress, psychological
摘要
目的:檢視嚴重精神病患者的親屬對照顧患者的經驗評估。
參與者與方法:應用中文版照顧經驗量表(CECI) 對親屬作出評估, 並把評估結果中的臨床相關因素, 結合簡明精神病評定量表(BPRS)、陰性症狀量表(SANS) ,以及駕馭感量表(MS) 來評估。
結果:評佮對象共81 位病人和129位照該者。CECI量度發現正面評估和負面評估之間呈正相關。陽性徵狀和抑鬱症狀與CECI的得分沒有顯著關係。 CECI的回歸分析顯示,負面經驗受功能評定量表(GAF) ,以及照顧者的教育程度所影響,而正面經驗則和患者的就業情況及照顧者的教育程度相關。
結論:照料嚴重精神病毒甚者的經驗受不同因素影響。照顧者應從多角度入手, 把注意力集中在家庭的具體需要上。
關鍵詞:照顧者、家庭健康、精神病患、心理壓力
Introduction
Psychiatric illnesses have a major impact on both patients and their relatives.1,2 Caring for a relative with mental illness significantly affects all aspects of the caregivers’ life.3,4 The consequence of this caregiving role is formally known as the ‘caregiving burden’.
In order to understand its determinants, mediating influences, and effects on clinical outcome, researchers have tried to study the caregiving burden using psychological or social theory.5-9 Baronet10 reviewed 34 previous studies on the determinants of the caregiving burden. Major categories of variables included the socio-demographic data of patients and caregivers, and illness-related factors. Other studies emphasised the relationship between coping strategies and the caregiving burden.6,8,9 Younger caregivers were reported to experience a higher caregiving burden.11 Having a patient of a younger age was associated with a higher negative appraisal.12 Residing with the relative was found to be associated with a high caregiving burden.13-15 People with a lower educational background suffered greater distress,16 while a higher educational level was associated with less subjective burden.16 Positive17-19 or negative symptoms20,21 of psychosis specifically caused a greater caregiving burden but a recent study found that symptomatology does not predict the negative appraisal of burden.11
Coping skills and sense of mastery affect the caregiver’s burden. Coping strategies are the characteristic strategies that an individual uses to handle stress.22 A ‘stress-coping’ model, based on the ‘stress-appraisal-coping’ paradigm of Lazarus and Folkman, was developed.22 Caregivers who practise coping strategies that emphasise problem-focused techniques experience less burden.23-25 Caregivers with a stronger sense of mastery were found to have less subjective burdens or appraisals of caregiving.6,7,26
A study of ethnic Chinese families found that they were more affected by stigma than western families.27 Previous local studies on the caregiver’s burden have demonstrated that families of schizophrenic patients suffer social costs, such as loss of social ties, financial difficulties, and strained family relationships,28 as well as emotional costs such as anger, sadness, and anxiety.29 There have been few quantitative studies evaluating the caregiving burden until Wong30 demonstrated that caregivers with a stronger sense of mastery have better psychological well-being. Illness-related factors, such as diagnosis, symptomatology, functioning of patients, and duration of illness have not been studied in a local Chinese setting. Our study evaluated the determinants of the caregiving experience in relatives of persons with severe mental disorders. Their appraisal of the caregiving experience was examined by analysing the impact of the ‘sense of mastery’ on the experience of caregiving.
Methods
Subjects and Setting
All patients admitted to the New Territories East Psychiatric Observation Unit of Tai Po Hospital in Hong Kong between March 2002 and June 2002 were screened (catchment population = 900,000, Census and Statistics Department, 2001). The selection criteria were as follows: (1) diagnosed as having one of the severe mental disorders: schizophrenia, schizotypal and delusional disorder, and severe affective disorder as evaluated by two qualified psychiatrists within 1 week of admission. Patients who were readmitted during the study period had their diagnosis assessed during the first admission only; (2) aged between 15 and 65 years; (3) ethnically Chinese; (4) no psychiatric co-morbidity; (5) ability to comprehend and complete the interview; and (6) ability to give informed consent to participate in the project.
Caregivers were invited by telephone to attend the interviews. The interviews were conducted within 2 weeks of the patients’ admission, by either the author or the clinical psychologist in-charge at the hospital, who was familiar with the instruments, or by 2 trainee clinical psychologists. The author conducted all patient interviews. Both patients and caregivers gave written informed consent before assessment. Approval was obtained from the Medical Ethics Committee of the Tai Po Hospital.
Assessment
Socio-demographic Information of Caregivers and Patients
Caregivers reported socio-demographic information, including age, gender, kinship, marital status, educational level, whether he or she lived with the ill relative, type of housing, area of housing, number of people in the same household, occupation, and family income. Patients’ demographic information included age, gender, marital status, educational level, occupation, and living conditions. The amount of direct contact between the relative and the patient each week was recorded.
Caregivers’ Burden — Experience of Caregiving Inventory
This 66-item self-report questionnaire—Experience of Caregiving Inventory (ECI)—was originally developed for use with caregivers of patients with severe mental illness.7 It measures the caregivers’ appraisal of the caregiving experience in the preceding 4 weeks. It consists of 52 items measuring 8 negative appraisal subscales, and 2 positive appraisal subscales including ‘positive personal experiences’ and ‘good aspects of the relationship’. Items are scored on a 5-point Likert scale from 0 (never) to 4 (always). Overall positive and negative scores are calculated by summation of these subscores. A validation of the Chinese ECI was conducted and it was found to have satisfactory internal consistency (Cronbach α = 0.49-0.85) and the test-retest reliability (intra-correlation coefficient = 0.83-0.97) was good.31
Coping Resources — Mastery Scale
This is a 7-item scale — Mastery Scale (MS) — measuring the degree to which individuals perceive personal mastery over life outcomes.32 A Chinese version has been translated33 and is commonly used. Internal consistency of the scale is satisfactory.34 Subjects rate items on a 4-point Likert scale, ranging from -2 (strongly disagree) to 2 (strongly agree).
Psychiatric Symptomatology
Positive, negative, and depressive symptoms were rated with the Brief Psychiatric Rating Scale,35 the Scale for the Assessment of Negative Symptoms (SANS),36 and the Hamilton Depression Rating Scale 17-item version.37 The Global Assessment of Functioning (GAF)38 at 4 weeks and 1 year before admission was also performed.
Statistical Analysis
Data were analysed with the Statistical Package for the Social Sciences (Windows version 10.0; SPSS Inc, Chicago [IL], US). Predictors of relatives’ negative and positive appraisals were investigated by calculating the univariate regression coefficients for each independent variable. Variables that demonstrated significance levels of p < 0.05 were then entered into a stepwise multiple regression analysis for further investigation.
Results
A total of 81 patients and 129 caregivers were recruited. There was no significant difference in the demographic characteristics of patients who entered the study and patients who did not. The mean age of patients was 35.1 (standard deviation [SD], 11.1; range, 17-62) years and 63% had a diagnosis of schizophrenia, 17% suffered from affective disorder, 5% had schizoaffective disorder, and the remaining 15% had other psychoses. The mean age of the caregivers was 45.3 (SD, 13.5; range, 16-79) years and 64% were female. Most caregivers (44%) were parents, 25% were partners, 17% were siblings. The mean number of years in education of the caregivers was 9.3 (SD, 5.3) years, 44% were educated up to secondary school level, 40% up to primary level or below. The patient’s diagnosis and the duration of illness also showed no significant relationship with the amount of contact time.
Socio-demographic Characteristics and Experience of Caregiving Inventory
There were no gender differences in the caregiving appraisals. Younger caregivers tended to give a more positive appraisal, though this was not statistically significant (r = –0.21, p = 0.06). The caregivers’ length of education significantly correlated with both negative (r = 0.25, p = 0.03) and positive appraisals (r = 0.28, p = 0.01). Caregivers who were employed showed higher positive appraisal (t = –2.39, p = 0.02). There was also a positive correlation between positive and negative appraisals (r = 0.32, p = 0.003) [Table 1].
Psychiatric Symptomatology and Appraisal of Caregiving
Table 2 shows the association between clinical variables and the appraisal of caregiving. The total score of the SANS showed a non-significant trend towards a negative correlation with positive appraisal (r = –0.29, p = 0.07). The negative symptom subscales had a significant negative correlation between ‘avolition-apathy’ and the positive appraisal (r = –0.29, p = 0.01). The GAF score 1 year before the index admission was negatively correlated (r = –0.27, p = 0.01) with the negative appraisal, and also showed a trend towards a positive correlation with the positive appraisal (r = 0.21, p = 0.06). There was no significant correlation between the recent GAF score and the appraisals of caregiving. No significant relationship was found between appraisal and other clinical variables.
The Association between Mastery Scale and Experience of Caregiving Inventory Scores
The mean score on the MS was 4.40. There was a negative correlation between the age of the caregiver and ‘rational problem-solving’ (r = –0.32, p = 0.003) and ‘seeking support and ventilation’ (r = –0.44, p < 0.001). There was no significant relationship between the gender of caregivers and various ways of coping (p > 0.05). There was a significant positive correlation between the years of education of caregivers and ‘rational problem-solving’ (r = 0.48, p < 0.001) and ‘seeking support and ventilation’ (r = 0.46, p < 0.001). Correlation of the MS with ECI scores showed that a better sense of mastery was associated with less negative appraisal in caregivers (r = –0.24, p = 0.03). There was no significant relationship between the MS score and positive appraisal.
Predictors of Appraisal of Caregiving
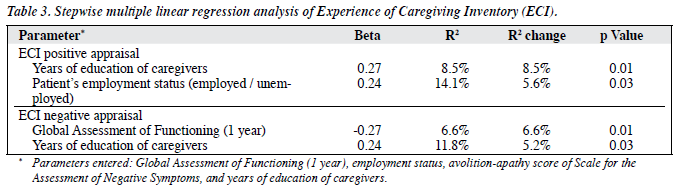
Significant variables, including patients’ employment status, GAF score 1 year before admission, the ‘avolition-apathy’ score in the SANS, and the caregivers’ educational levels, were entered into a regression analysis with positive and negative appraisals as the dependent variables (Table 3). The caregivers’ educational levels accounted for 8.5% of the variance, and the patients’ employment status accounted for 5.6% of the variance in positive appraisal. For negative appraisals, the GAF score at 1 year before admission and caregivers’ years of education together accounted for 11.8% of the variance.
Discussion
One interesting finding was the positive correlation between negative and positive appraisals of caregiving, a finding that was reported in a previous study.12 This may be reflective of ‘commitment’ in the process of caregiving.12 Relatives who are more committed to caregiving perceived more difficulties and more rewards than relatives who are more detached. Higher scores of ‘avolition-apathy’ negative symptoms were associated with lower positive appraisals. No significant correlation was found between the appraisals of caregiving and either positive or depressive symptoms. Relatives of unemployed patients had lower positive appraisals, while relatives of patients with poorer social functioning appraised caregiving more negatively. These findings were also consistent with other studies that examined the effect of patients’ employment and social functioning on the caregiving experience.11,39-41
Previous studies have found that older caregivers had a higher burden.42,43 In this study, there was no significant relationship between caregivers’ age and negative appraisal. There was, however, a trend towards less positive appraisal from older relatives. A previous study9 has showed that the adoption of problem-focused strategies was more frequent among young relatives. Caregivers who received higher education showed both higher negative and positive appraisals.15,44 It is possible that subjects who are more educated adopted active problem-focused coping more frequently when they encountered negative appraisal. The mean MS score in this study was higher than the mean score of 2.38 that was found in another local study.30 This suggests a better sense of mastery, and hence greater coping resources, in our caregivers. Relatives with a better sense of mastery appraise caregiving less negatively, a phenomenon demonstrated by other studies.6,7,45
The findings of this study have several implications. Predictors of the appraisals of caregiving suggest specific interventions likely to relieve the distress of caregivers. Our study suggests that interventions or treatments that aim to improve the functioning of the patient might reduce the caregivers’ negative appraisal. Improvement of the patients’ employment status and negative symptoms may enhance caregivers’ positive appraisal and, eventually, decrease psychological distress. Interventions that enhance rational problem-solving coping strategies and mastery may relieve psychological distress and bring about positive changes in distress, burden, and coping.46
References
- Hatfield AB, Lefley HP. Families of the mentally ill: coping and adaptation. New York: Guilford Press; 1987.
- Tessler RC, Killian LM, Gunman GD. Stages in family response to mental illness: an ideal type. Psychosocial Rehabilitation Journal 1987;10:3-16.
- Clausen JA, Yarrow MR. The impact of mental illness on the family. J Soc Issues 1955;11:3-64.
- Grad J, Sainsbury P. The effects that patients have on their families in a community care and a control psychiatric service—a two year follow- up. Br J Psychiatry 1968;114:265-78.
- Maurin JT, Boyd CB. Burden of mental illness on the family: a critical review. Arch Psychiatr Nurs 1990;4:99-107.
- Solomon P, Draine J. Subjective burden among family members of mentally ill adults: relation to stress, coping, and adaptation. Am J Orthopsychiatry 1995;65:419-27.
- Szmukler GI, Burgess P, Herrman H, Benson A, Colusa S, Bloch S. Caring for relatives with serious mental illness: the development of the Experience of Caregiving Inventory. Soc Psychiatry Psychiatr Epidemiol 1996;31:137-48.
- Webb C, Pfeiffer M, Mueser KT, Gladis M, Mensch E, DeGirolamo J, et al. Burden and well-being of caregivers for the severely mentally ill: the role of coping style and social support. Schizophr Res 1998;34:169- 80.
- Magliano L, Fadden G, Economou M, Xavier M, Held T, Guarneri M, et al. Social and clinical factors influencing the choice of coping strategies in relatives of patients with schizophrenia: results of the BIOMED I study. Soc Psychiatry Psychiatr Epidemiol 1998;33:413- 9.
- Baronet AM. Factors associated with caregiving burden in mental illness: a critical review of the research literature. Clin Psychol Rev 1999;19:819-41.
- 1 Horwitz AV, Reinhard SC. Ethnic differences in caregiving duties and burdens among parents and siblings of persons with severe mental illnesses. Journal of Health and Social Behaviour 1995;36:138-50.
- Harvey K, Burns T, Fahy T, Manley C, Tattan T. Relatives of patients with severe psychotic illness: factors that influence appraisal of caregiving and psychological distress. Soc Psychiatry Psychiatr Epidemiol 2001;36:456-61.
- Jones SL, Roth D, Jones PK. Effect of demographic and behavioral variables on burden of caregivers of chronic mentally ill persons. Psychiatr Serv 1995;46:141-5.
- Pickett SA, Greenley JR, Greenberg JS. Off-timedness as a contributor to subjective burdens for parents of offspring with severe mental illness. Fam Relat 1995;44:195-20l.
- Tessler R, Gamache G. Continuity of care, residence, and family burden in Ohio. Milbank Q 1994;72:149-69.
- Noh S, Turner RJ. Living with psychiatric patients: implications for the mental health of family members. Soc Sci Med 1987;25:263-72.
- Wing JK, Monck E, Brown GW, Carstairs GM. Morbidity in the community of schizophrenic patients discharged from London mental hospitals in 1959. Br J Psychiatry 1964;110:10-21.
- Grad J, Sainsbury P. Mental illness and the family. Lancet 1963;1:544- 7.
- Raj L, Kulhara P, Avasthi A. Social burden of positive and negative schizophrenia. Int J Soc Psychiatry 1991;37:242-50.
- Creer C, Wing JK. Schizophrenia at home. In: Elliot GR, Eisdorfer C, editors. Stress and human health. New York: Springer; 1982.
- Fadden G, Bebbington P, Kuipers L. The burden of care: the impact of functional psychiatric illness on the patient’s family. Br J Psychiatry 1987;150:285-92.
- Lazarus RS, Folkman S. Stress appraisal, and coping. New York: Springer, Berlin Heidelberg; 1984.
- Falloon I, Pederson J, Al-Khayyal M. Enhancement of health-giving family support versus treatment of family pathology. Journal of Family Therapy 1986;8:339-50.
- Birchwood M, Cochrane R. Families coping with schizophrenia: coping styles, their origins and correlates. Psychol Med 1990;20:857-65.
- Bentelspacher C, Chitran S, Rahman M. Coping and adaptation patterns among Chinese, Indian and Malay families caring for a mentally ill relative. Fam Soc 1994;75:287-94.
- Noh S, Avison WR. Spouses of discharged psychiatric patients: Factors associated with their experience of burden. J Marriage Fam 1988;50:377-89.
- Ryder AG, Bean G, Dion KL. Caregiver responses to symptoms of first-onset psychosis: A comparative study of Chinese- and Euro- Canadian families. Transcult Psychiatry 2000;37:255-65.
- Chan KF. The impact of schizophrenia on Hong Kong Chinese families. The Hong Kong Journal of Social Work 1995;29:21-34.
- Pearson V, Ning SP. Family care in schizophrenia: an undervalued resource. In: Chan CL, Rhind N, editors. Social work intervention in health care. Hong Kong: The Hong Kong Scene; 1997.
- Wong DF. Stress factors and mental health of carers with relatives suffering from schizophrenia in Hong Kong: implications for culturally sensitive practices. Br J Soc Work 2000;30:365-82.
- Lau DY, Pang AH. Validation of the Chinese version of Experience of Caregiving Inventory in caregivers of persons suffering from severe mental disorders. Hong Kong J Psychiatry 2007;17:24-31.
- Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav 1978;19:2-21.
- Cheng P, Tang CS. Coping and psychological distress of Chinese parents of children with Down syndrome. Ment Retard 1995;33:10- 20.
- Turner RJ, Noh S. Physical disability and depression: a longitudinal analysis. J Health Soc Behav 1988;29:23-37.
- Lukoff D, Liberman RP, Nuechterlein KH. Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophr Bull 1986;12:578- 602.
- Andreasen N. The Scale for the Assessment of Negative Symptoms (SANS). Iowa: University of Iowa, Department of Psychiatry; 1984.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994.
- Scazufa M, Kuipers E. Stability of expressed emotion in relatives of those with schizophrenia and its relationship with burden of care and perception of patients’ social functioning. Psychol Med 1998;28:453- 61.
- Szmukler GI, Wykes T, Parkman S. Care-giving and the impact on carers of a community mental health service. PRiSM Psychosis Study. Br J Psychiatry 1998;173:399-403.
- Joyce J, Leese M, Szmukler G. The Experience of Caregiving Inventory: further evidence. Soc Psychiatry Psychiatr Epidemiol 2000;35:185-9.
- Horwitz AV, Reinhard SC. Ethnic differences in caregiving duties and burdens among parents and siblings of persons with severe mental illnesses. J Health Soc Behav 1995;36:138-50.
- Stueve A, Vine P, Struening EL. Perceived burden among caregivers of adults with serious mental illness: comparison of black, Hispanic, and white families. Am J Orthopsychiatry 1997;67:199-209.
- Greenberg JS, Kim HW, Greenley JR. Factors associated with subjective burden in siblings of adults with severe mental illness. Am J Orthopsychiatry 1997;67:231-41.
- Noh S, Avison WR. Spouses of discharged psychiatric patients: Factors associated with their experience of burden. J Marriage Fam 1988;50:377-89.
- Falloon IR, Pederson J. Family management in the prevention of morbidity of schizophrenia: the adjustment of the family unit. Br J Psychiatry 1985;147:156-63.