Hong Kong J Psychiatry 2007;17:115-23
ORIGINAL ARTICLE
Dr Kavin KW Chow, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Shatin Hospital, Ma On Shan, New Territories, Hong Kong, China.
Dr FS Ng, MBChB, MRCPsych, FHKCPsych, FHKAM (Psychiatry), Private practice.
Address for correspondence: Dr Kavin KW Chow, Shatin Hospital, 33 A Kung Kok Street, Ma On Shan, New Territories, Hong Kong, China.
Tel: (852) 2636 7748; Fax: (852) 2647 5321;
E-mail: kavinchow@gmail.com
Submitted: 15 August 2007; Accepted: 25 September 2007
Abstract
Objectives: To investigate the prevalence of violence among psychiatric patients in Hong Kong and its associated risk factors.
Participants and Methods: Retrospective case notes analysis of patients admitted to the psychiatric units of the New Territories East Cluster of Hong Kong within the period from 1 January to 31 March 2005. Patients were divided into those with and without violent behaviour. The 2 groups were compared for socio-demographic and psychopathological variables.
Results: Case notes of 515 patients, aged between 18 and 64 years, with diagnosable psychiatric disorders were studied. The prevalence of violent behaviour within 4 weeks of the index admission was 18.6%. Violence was particularly associated with older patients diagnosed with psychotic disorders and having persecutory delusion and agitation.
Conclusions: The prevalence of violent behaviour was comparable to what has been reported in similar studies from western countries. Associated risk factors were identified for which preventive measures should be implemented accordingly.
Key words: Mental disorders; Patient admission; Prevalence; Risk factors; Violence
摘要
目的:研究香港精神病患者的暴力現患率及相關的危險因素。
參與者與方法:回顧分析2005年1 月1 日至3月31 日期間,入往香港新界東醫院聯網精神科病房的紀錄。 病人分成「 暴力行為組」 及「 無暴力行為組」,並比較兩組的社會人口學及精神病理學變項。
結果:分析515位18至64歲病人的精神病患紀錄。首次入院4星期內的暴力現患率達18.6% 。暴力行為與年齡較大及是患有思覺失調, 並有被害妄想症和激越行為有關。
結論:精神病患者暴力的現患率與西方研究結果相似,亦確認了相關的危險因素,以制定預防措施。
關鍵詞:精神病、病人入院、現患率、危撿因素、暴力
Violence in patients with mental disorder has always been an important area of concern. An influential German study published in 1982 concluded that persons with psychiatric disorder were no more likely to be violent than the general population.1 In the last 2 decades however, other studies suggested that there was a moderate and reliable association between mental disorder and violence.2,3 According to the Cambridge Advanced Learner’s Dictionary, violence is defined as “actions or words which are intended to hurt people”. In relation to psychiatric practice, there was no single, universal definition. Swanson et al4 defined violence as “any physical fighting or assaultive actions causing bodily injury to another person, or as any use of a lethal weapon to harm or threaten someone”. Despite the differences between such definitions, their common ingredients include: acts or threats of force, with or without weapons that could lead to injury or damage. The Royal College Research Unit in 1998 defined a violent incident as “a situation where a mental health service user is either actively violent or on the brink of being so”. In the general population, a number of factors were identified as predictors of a propensity to violence.5,6 Further exploration was required to find out whether similar factors contributed to violent behaviour in psychiatric patients. Research strategies for investigating the relationship between mental illness and violent behaviour can be classified into 3 broad categories.
The first approach involved community studies, which examined the presence of mental illness and the level of engagement in violent behaviour. In one of the most important studies of this type,7 data pertaining to 10,059 subjects from the Epidemiological Catchment Area Study in the United States were analysed. Psychiatric assessment of the participants was based on the Diagnostic Interview Schedule (DSM-III) and their levels of violent behaviour were studied. Those reporting violent behaviour within the preceding year tended to be young, male, and of low socio-economic status; more than half of them met DSM- III criteria for one or more psychiatric disorders. The risk of violent behaviour increased with the number of psychiatric diagnoses that the respondents met. In another major community-based study, Link et al8 compared the official and self-reported violence of psychiatric patients with community residents who never received psychiatric treatment. They found that psychiatric patients had higher rates of violence than community residents. Stueve and Link9 found that there was a higher rate of violence among psychiatric patients than the general population. These community studies were subject to sampling bias, because seriously ill as well as seriously violent subjects were excluded.
The second approach was to examine the frequency of mental illness in people who behaved violently. One pre-eminent study examined the psychiatric status of 1,241 men remanded to Brixton Prison in London, England.10 Nine percent of those subsequently convicted of non-fatal violent crimes and 11% convicted of fatal violence were diagnosed as having schizophrenia. Monahan11 using data from a California prison study concluded that the incidence of schizophrenia among prisoners was 6%, which was more than 3 times the estimated rate in the general American population of 1.7%. Teplin12 investigated 728 remanders in the United States that the prevalence of schizophrenia in the jail population was 2.7%, also 3 times higher than that of the general population (0.91%). In Australia, Wallace et al13 found that those with schizophrenia were 4 times more likely to be convicted of interpersonal violence and 10 times more likely to be convicted of homicide than members of the general population. Studies based on offender populations were complicated both by the selection process, and by the high rates of substance abuse and severe personality disorder which tended to obscure mental illness, if it was present.14,15
The third approach was to investigate the level of violent behaviour in mentally ill people.16,17 These studies reported high rates of assaultiveness, particularly among inpatients with schizophrenia. However, Powell et al18 suggested that violent acts committed by patients during their hospitalisation were not solely related to their disturbed state of mind. Provocative environmental factors, including other patients or staff, as well as hospital routines and restrictions, were also conducive to violent reactions. Similarly, Sheridan et al19 also concluded that violence among inpatients was more related to external factors than to their disordered state of mind. In the Northwick Park Study of first-episode schizophrenia,20 19% of the subjects were identified as behaving in a threatening manner 1 month prior to their first admission. Binder and McNeil21 reported an even higher rate of violent behaviour; 26% of those admitted to an acute psychiatric unit had been assaultative in the 6 months prior to their admission. Monahan22 summarised findings from 3 reviews, which reported 11 studies over 15 years. Based on the various study samples reviewed, he inferred that 10 to 40% of the patients committed violent acts against others shortly before they were hospitalised, the median rate being 15%.
The present study aimed at exploring the prevalence of violent behaviour in psychiatric patients before their index admissions to the psychiatric inpatient units. Predictors of violence, such as the socio-demographic and psychopathological variables, were also investigated. The nature of the violent acts and targeted victims were also documented. It was hoped that the present study could reveal the risk factors for such violence in psychiatric patients and that this could indicate important directions for future research.
Methods
Study Design
This was a retrospective case note analysis of psychiatric patients admitted as inpatients to psychiatric units of the New Territories East (NTE) Cluster of Hong Kong, within the period from 1 January to 31 March 2005. At the time of data collection, the NTE Cluster covered a region with a total population of about 1.3 million. Psychiatric patients who were assessed to have high risk of violence were monitored by intensive aftercare services by mental health teams. A priority follow-up (PFU) system was established for these groups of patients in 1982. The PFU system divided patients into the non-PFU, PFU target, and PFU sub-target groups. Patients were classified as belonging to the PFU (target) group if they had a history of violence or were assessed to exhibit future violence. Patients considered to be the most dangerous (by virtue of significant risk for future violence) were classified as being in the PFU sub-target group. Patients assessed to be at low risk of violence were classified as being in the non-PFU group. In addition to the PFU system, the development of community psychiatric nurse (CPN) services in Hong Kong also aimed to provide more intensive psychiatric services for patients with high propensity of violence. In Hong Kong, the Mental Health Ordinance (Chapter 136) also stipulated a so-called ‘conditional discharge’ (CD) status. This means that psychiatric inpatients with a risk of violence could be conditionally discharged back to the community, if they agreed to comply with certain specified conditions. In the present study, data were only collected from case notes.
Patients with age under 18 or above 64 years were excluded. Data relating to the violence, diagnosis, and socio-demographic factors were extracted and recorded.
Case Definition
Every patient admitted to the psychiatric wards had been examined by a qualified psychiatrist and a formal psychiatric diagnosis (according to the International Classification of Diseases–10th revision) was established in the respective multi-disciplinary ward round chaired by a consultant psychiatrist. Patients with diagnosable psychiatric disorders were divided into 2 groups: one ‘with violent behaviour’ and one ‘without violent behaviour’. Violent behaviour was defined as exhibition of either one of the following within 4 weeks prior to the admission: (i) verbal threat towards persons — threatening words that made a person feel afraid of being physically harmed; (ii) physical aggression against a person — fights in which someone was hit, slapped, kicked, grabbed, shoved, bitten, hurt with knife or gun, or had something thrown at them; and (iii) physical aggression against objects — physical acts with an attempt to break or damage an object. Measurement of violence relied on self- reporting, key informants, official records such as police, court or social services department case notes. Having classified the cases into these 2 groups, they were then compared for socio-demographic and psychopathological variables.
Statistical Analysis
The results were analysed using the Statistical Package for the Social Sciences for Windows version 12. For data that were categorical, the Chi-square test was used for comparison, and for continuous variables such as age and length of hospitalisation, independent t tests were used. Differences between continuous variables were also subjected to analyses of variance, with the post- hoc Bonferroni test delineating group differences. For multivariate analyses, the backward stepwise procedure of multiple logistic regression was performed to investigate risk factors associated with violence. Only those variables which yielded p values of less than 0.1 in the univariate analyses were included in the regression. The level of statistical significance was set at 0.05. All tests were 2-sided. Ninety five percent confidence intervals were provided when appropriate. The study was approved by the Joint Clinical Research Ethics Committee of the Chinese University of Hong Kong and NTE Cluster Hospitals.
Results
Demographic Characteristics
Five hundred and sixty eight case notes were reviewed. A majority (93%) were adults, their ages ranged from 18 to 64 years. In all, 28 (5%) patients were (geriatric) older than 64 years and 14 (2%) were adolescents (age < 18 years). The number of cases in these 2 age-groups (adolescent and geriatrics) was small and they have distinct characteristics related to mental illness and violence compared to adult population. Therefore only data from adult patients aged 18 to 64 years were included in the analysis. Among the 526 patients in this group, 11 (2%) had no formal psychiatric diagnosis for the index admission and were also excluded. Thus, only 515 cases were included in the final analysis. The prevalence of patients exhibiting violent behaviour in the 4 weeks prior to the index admission was 19%. Accordingly, the subjects were categorised into 2 groups: ‘with violent behaviour’ and ‘without violent behaviour’. Ninety six subjects were classified as belonging to the violence group and 419 to the non-violent group (Table 1). For the purpose of classifying the types of violence committed by subjects in the former group, the latest recorded violent act within 4 weeks prior to admission was documented.
History of Violence and Psychiatric Illness in the Study Population
Sixty three (12%) of the patients had forensic records and 20 (4%) had a history of criminal violence. Eighty seven (17%) had a history of substance or alcohol abuse. Less than 5% of them had a history of problems related to conduct and behaviour. A few subjects had a history of childhood psychiatric disorder. Sixty seven (13%) had a history of violence towards people, towards objects, and verbal threats, in decreasing order of frequency (Table 2). Only 14 (3%) of them were classified as being under a CD order. One hundred and forty (27%) patients were being followed up by CPNs before their index admission, and 282 (67%) had not received a CD order or been followed up by CPNs. Three hundred and fifty one (68%) subjects had a history of previous psychiatric admissions, whilst 430 (83%) had been followed up by public or private sector psychiatrists, before their index admission (Table 2). Of those receiving psychiatric services and medications, over two-thirds were regular attendees at psychiatric clinics, half of whom reported good compliance with their drug treatment. Psychotic disorders accounted for about 50% of their diagnoses. Others included mood and anxiety disorders (n = 164, 32%), personality disorders (n = 6, 1%), organic brain disorders (n = 8, 2%), substance-related non- psychotic disorders (n = 11, 2%), and mental retardation (n = 13, 3%). Thirty (6%) subjects had an additional co-morbid psychiatric diagnosis. The mean (standard deviation [SD]) duration of psychiatric illness was 9.4 (8.7) years (range, 0.1-37 years).
Index Admission
Over half (n = 301, 58%) of the subjects were admitted via the Accident and Emergency Department, and over 80% were admitted on an informal or voluntary basis (n = 429); 86 (17%) were admitted on a compulsory basis. Among these 515 subjects, the commonest diagnosis was psychotic disorder (n = 306, 59%). Other diagnoses included: mood and anxiety disorders (n = 152, 30%), organic brain disorders (n = 15, 3%), substance-related non-psychotic disorders (n = 21, 4%), personality disorders (n = 6, 1%), and mental retardation (n = 15, 3%). The median duration of hospitalisation was 25 (range, 1-214) days. Regarding the violent acts committed in the 4 weeks prior to admission by the 96 subjects in the violence group, 3 (3%) had taken alcohol and 9 (9%) had a history of substance use before the index incident. Violence was mostly targeted against people (83%); only 13% of the acts were against objects and 4% were verbal threats. Around 80% of the index violent acts occurred in the 2 days before admission. Parents and spouses (41%) were the main targets of violence. Very few violent acts (2%) were against strangers, and most occurred in the patient’s home (68%), followed by hostels (6%), and sheltered workshop (4%). Evidently, motivation for violence was mostly related to arguments (34%) and financial disputes (12%).
Comparison of Violence and Non-violent Groups
Demographic Features
In the violence and non-violent groups, the respective male-to-female ratio was 1.4:1 and 0.73:1, the difference being statistically significant (χ2 test, p = 0.004). However, the mean ± SD age of patients in the respective groups was similar (38 ± 12 years vs. 37 ± 11 years), as was their marital status. The non-violent group had higher levels of education (χ2 test, p = 0.01), and a lower proportion lived in long-stay care homes, halfway houses, or other institutions such as hostels (χ2 test, p = 0.05). There was no statistically significant difference in occupational status between patients in the 2 groups. A greater proportion in the violence than non-violent group lived in hostels (11% vs. 4%, Fisher’s exact test, p = 0.01). There was no difference between groups in terms of parental status in childhood, birth order rank among siblings, numbers of siblings per family, and family history of psychiatric illness (Table 1).
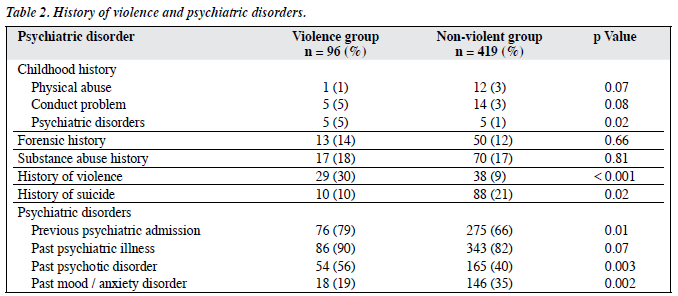
History of Violence and Psychiatric Illness
There was no statistically significant difference between the groups regarding any history of forensic records, substance abuse, childhood physical or other abuse, and childhood conduct problems. However, there was a larger proportion with childhood psychiatric disorders in the violence group (5% vs. 1%; Fisher’s exact test, p = 0.02) [Table 2].
In the violence group, around one-third (n = 29, 30%) had a lifetime history of violence, while in the non- violent group only one-tenth (n = 38, 9%) had such a history (χ2 test, p < 0.001). Respective mean proportions for the number of subjects who had committed violent acts in the past were 0.45 versus 0.11 (Student’s t test, p < 0.001). In the violence group, 21% of the violence was directed at people and 9% against objects. In the non-violent group, 88 (21%) had a history of suicidal attempts, while 10 (10%) had such a history in the violent group (Fisher’s exact test, p = 0.02). More of the latter subjects had a history of previous psychiatric admissions (79% vs. 66%, χ2 test, p = 0.01) and a higher proportion of them had a history of psychotic disorders (56% vs. 40%, χ2 test, p = 0.003).
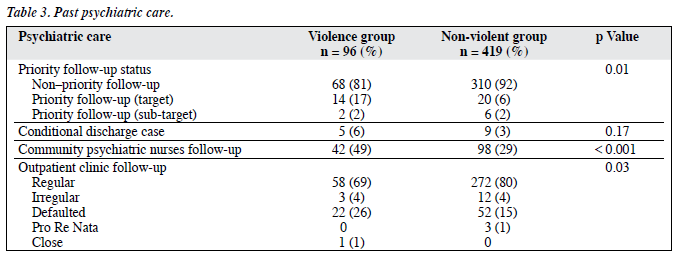
A greater proportion of subjects in the violence group had received antipsychotic treatment (66% vs. 54% [χ2 test, p = 0.03]), including antipsychotic depot injections (38% vs. 17%, χ2 test, p = 0.002). Whereas, a smaller proportion was taking atypical antipsychotic medication (33% vs. 45%), or had received antidepressant drugs (n = 9, 9% vs. n = 107, 26% [χ2 test, p = 0.001]). Drug compliance was better in the non-violent than violence group (n = 174, 42% vs. n = 33, 34% [χ2 test, p = 0.03]), whereas the converse was true for the proportion of defaulters and irregular attendees to the psychiatric outpatient clinic (26% vs. 15%, Fisher’s exact test, p = 0.03). Regarding the priority of their follow-up, a higher percentage in the violence group was assigned to PFU (19% vs. 8%, Fisher’s exact test, p = 0.01) prior to the index admission. Similarly, a higher proportion received CPN services (49% vs. 29%, χ2 test, p < 0.001) prior to the index admission. There was no significant difference between the 2 groups regarding their CD status (Table 3).
Index Admission
The violence group subjects had a longer mean (± SD) duration of hospitalisation (58.9 ± 53.4 days vs. 34.4 ± 36.1 days, t test, p < 0.001), and a greater proportion was admitted via the Accident and Emergency Department (68% vs. 56%, χ2 test, p = 0.05). In all, 48% of the latter subjects were admitted compulsorily, while around 91% of the non- violent subjects were admitted on an informal / voluntary basis (χ2 test, p < 0.001). During the index admission, more than two-thirds (77%) of the subjects in the violence group were diagnosed to have psychotic disorders, compared to 55% in the non-violent group (χ2 test, p < 0.001). Moreover, a greater proportion of the former had mental retardation (8% vs. 2%, χ2 test, p = 0.002).
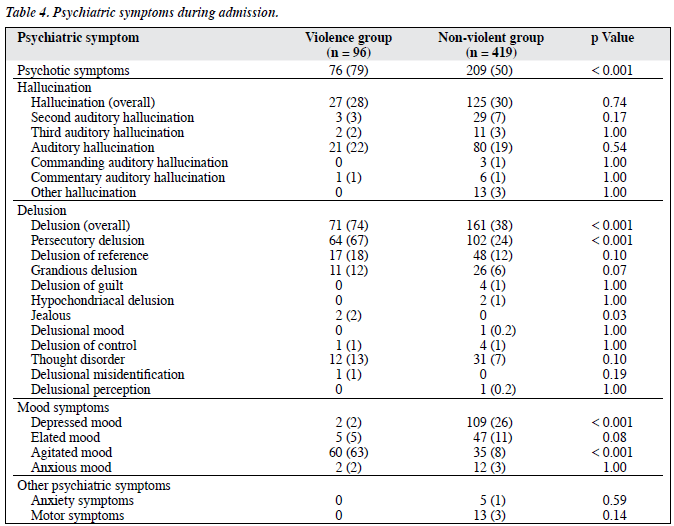
Subjects in the violence group more frequently presented psychotic symptoms, including: delusions and hallucinations (79% vs. 50%, χ2 test, p < 0.001), delusions (74% vs. 38%, χ2 test, p < 0.001), and agitation (63% vs. 8%, χ2 test, p < 0.001), but less frequently had depressed mood (2% vs. 26%, Fisher’s exact test, p < 0.001). Subjects in the violence group more frequently reported delusions of persecution, jealousy, and agitation (Table 4). There was no statistically significant difference between the groups in terms of anxiety and motor symptoms.
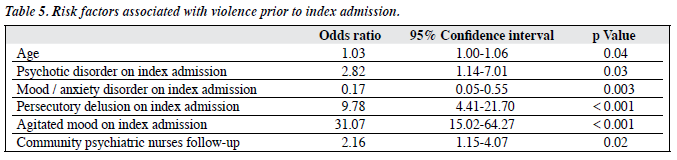
Risk Factors for Violence
Using multivariate analyses, associated risk factors for violence were identified. These were: older age (odds ratio [OR] = 1.03, 95% confidence interval [CI] = 1.00- 1.06, p = 0.04), and being under the care of CPN services (OR = 2.16, 95% CI = 1.15-4.07, p = 0.02). Specific clinical variables included: diagnosis of a psychotic disorder (OR = 2.82, 95% CI = 1.14-7.01, p = 0.03), having persecutory delusions (OR = 9.78, 95% CI = 4.41-21.70, p < 0.001) and agitation (OR = 31.07, 95% CI = 15.02-64.27, p < 0.001) were also risk factors for violence. On the other hand, patients having mood and anxiety disorders appeared less liable to exhibit violence (OR = 0.17, 95% CI = 0.05-0.55, p = 0.003) [Table 5].
Discussion
The prevalence of violent behaviour among psychiatric patients in this study was 18.6% which was comparable to figures in western countries,20,23 though the rate of violence among male than female patients was higher.24,25 In Hong Kong, different gender socialisation processes may foster such disparity. A sociologist studying spousal homicide among all races in Canada suggested that women were socialised to be gentle, tender, less aggressive, and competitive than men.26 In addition, violence committed by men was more likely to result in serious injury — requiring treatment by physicians, and perhaps more likely to be arrested after committing a violent act than women.27 Violence committed by women occurred disproportionately against family members and occurred mostly at home. This may explain why violent acts committed by women often appear to be fewer, clinicians may therefore tend to underestimate the problem. History of emotional and physical abuse has been associated with criminal violent behaviour.28,29 The risk of violence in adulthood was also reported to be higher in patients with a history of childhood conduct disorder,30 but this was not confirmed in this study. In traditional Chinese culture, many prefer not to report this issue to the medical profession.
A higher percentage of subjects in the violence group were living in hostels, hence having poorer social functioning, community adjustment, and interpersonal relationships. Such characteristics have been suggested as risk factors for violence.31 Restrictions in halfway houses and their crowded living environment easily create conflicts, leading to subsequent violence among patients and staff. Moreover, violent acts were more likely to be reported by hostel staff in order to maintain discipline in these group settings.
Patients with a history of childhood psychiatric disorder, psychiatric admissions, and violence were more fre- quent in the violent group. Similarly, a history of aggression was also reported to increase risk of future violence32 and previous psychiatric admissions usually indicated a more severe mental disorder. We also found that patients in the PFU system and those being monitored by CPN services were more liable to violent behaviours before admission. In a certain sense, this observation was understandable, as patients included in the PFU system were known to be dangerous due to a history of violence. Apparently, the system did pick up high-risk subjects, but might not be effective in decreasing the rate of violence committed by these patients. A study by Walsh et al33 reported similar findings, in that intensive case management did not reduce the prevalence of violence in psychotic patients compared to standard care. After all, the causes of violent behaviour were complicated and close monitoring of only the mental state may not be an adequate solution. Nevertheless, the importance of the PFU system should not be undermined. As its name indicated, in essence the system was to locate these high-risk patients for PFU. In Hong Kong, community psychiatric care was only established in the mid-1990s and till now, psychiatric services were largely hospital-based, especially for patients at risk of violence. Despite the provision of PFU, there were only limited services for the defaulters and for most of the time, action could only be taken if patients posed a risk to themselves or others. This involved admitting patients for treatment under a compulsory order, which was unfortunately, too late in some instances. In this sense, a more comprehensive application of CDs within the PFU system might be preferable, as it could operate in a similar manner to involuntary outpatient commitment, which is a system that prevails in some western countries. By this means it could engage difficult-to-serve public mental health needs of many patients, especially those deemed at risks to becoming violent and dangerous without treatment.
In this study, patients diagnosed with psychotic disorders posed a higher risk of violence, which was consistent with strong evidence from western countries.24,34,35 It has been assumed that somehow, psychosis removed or inhibited an individual’s capacity for self-control and therefore, negated the psycho-dynamic barriers which prevent violence. Our patients on atypical antipsychotic medication appeared less likely to exhibit violent behaviour, treatment with atypical antipsychotics is reported to be particularly helpful in controlling violent impulses in those with psychotic disorders.36 However, the differing treatment patterns could be a consequence of poor drug compliance in patients exhibiting violence, leading to an increased use of depot treatment. An association between persecutory delusions and violent behaviour was also noted, which was consistent with hallucinations and delusions of persecution being subtypes of psychotic symptoms particularly related to violence.37-39 Link and Stueve40 suggested ‘threat control override’ symptoms were more related to violence, as such patients experienced feeling that others were trying to harm them and their minds via external dominating forces. Such fear and anger impaired their internal control and increased arousal levels to a point where their cognitive control was overwhelmed, thus resulting in a violent act. Substance abuse and alcoholism have a well-recognised association with violence and disturbed behaviour in psychiatric patients,41-43 though it was not present in this study for substance misuse. This might be explained by cultural difference in substance and alcohol use; prevalence of substance abuse being lower in Hong Kong (5% in men and 1.8% in women44) than in western countries.
Violence towards people was the commonest type in psychiatric patients; hitting with a fist or objects was the commonest means of doing so. Family members or relatives were the main target, which was also similar to findings in western countries45,46; very few victims (2.1%) were strangers. Thus, public concerns over the danger posed by psychiatric patients might be exaggerated, particularly because they are fuelled by the sensational reporting of unpredictable acts of violence in the media.
The results of the present study provide information on violent behaviour and its predictors in psychiatric patients in Hong Kong, aid in identifying those at high risk and devise ways to manage them, especially in community settings. Patients with certain persecutory delusions and agitation should be properly identified. Cognitive therapy or medication could help to reduce their perceived threats, and consequential violent reactions. Community psychiatric teams should closely monitor patients adhering poorly to treatment. Early intervention might prevent relapse of mental illness and subsequent violent events. More training in anger management, community living, and social skills may reduce conflicts among patients and others. Psycho- educational talks provided to hostel staff on the early warning features of violence could also help to reduce such behaviour in hostels. Psycho-education should also be provided to family members and acquaintances of patients as they have a higher risk of becoming victims of violence. Preventive steps could then be undertaken at an early phase of relapse to minimise the risk of violence.
This was a retrospective study, in which only the case notes were reviewed, has obvious limitations. Since the patient was not interviewed during the index admission, psychiatric diagnoses were based mainly on clinical judgement without any type of standardised assessment. Personality traits or other disorders of patients could not be assessed. Therefore the association between personality disorder and violent behaviour could not be correctly ascertained. Besides, the definition of violence was also arbitrary, and its prevalence may have been over- or under-estimated. Certain psychopathology, especially that relating to violent acts, might not be clearly documented. Nowadays however, relevant documentation was based on a multidisciplinary approach and input, which must have minimised the chance of invalid observations and errors. The other main limitation was that certain psychiatric patients might be sentenced to jail after violent acts instead of being admitted to hospital. Thus, the most seriously ill as well as the most seriously violent patients might have been excluded.
In Hong Kong, violence by psychiatric patients has raised many concerns for the public. It is hoped that the results of this study could shed light on the nature of risk factors for violence among psychiatric patients, and that recognition of such factors could provide useful information for future follow-up studies.
Acknowledgements
I would like to use this opportunity to thank Drs S Fong, CM Leung, I Kam, J Tsoh, and Prof GS Ungvari from the Department of Psychiatry, Shatin Hospital, for their comments on the development of protocol and final report.
References
- Hafner H, Boker W. Crimes of violence by mentally abnormal offenders. Cambridge: Cambridge University Press; 1982:5.
- Lindqvist P, Allebeck P. Schizophrenia and crime. A longitudinal follow-up of 644 schizophrenics in Stockholm. Br J Psychiatry 1990;157:345-50.
- Hodgins S. Mental disorder, intellectual deficiency, and crime. Evidence from a birth cohort. Arch Gen Psychiatry 1992;49:476-83.
- Swanson JW, Swartz MS, Essock SM, Osher FC, Wagner HR, Goodman LA, et al. The social-environmental context of violent behaviour in persons treated for severe mental illness. Am J Public Health 2002;92:1523-31.
- Monahan, J. Clinical and actuarial predictions of violence. In: Faigman D, Kaye D, Saks M, Sanders J, editors. Modern scientific evidence: the law and science of expert testimony. St. Paul, MN: West Publishing Company; 1997:315.
- Walsh E, Buchanan A, Fahy H. Violence and schizophrenia: examining the evidence. Br J Psychiatry 2002;180:490-5.
- Swanson JW, Holzer CE 3rd, Ganju VK, Jono RT. Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys. Hosp Community Psychiatry 1990;41:761-
- Erratum in: Hosp Community Psychiatry 1991;42:954-5.
- Link BG, Andrews H, Cullen FT. The violent and illegal behaviour of mental patients reconsidered. Am Sociol Rev 1992;57:275-92.
- Stueve A, Link BG. Gender differences in the relationship between mental illness and violence: evidence from a community-based epidemiological study in Israel. Soc Psychiatry Psychiatr Epidemiol 1998;33 Suppl 1:S61-7.
- Taylor P, Gunn J. Violence and psychosis. I. Risk of violence among psychotic men. Br Med J (Clin Res Ed) 1984;288:1945-9.
- 1 Monahan J. Mental disorder and violence: another look. In: Hodgins A, editor. Mental disorder and crime. California: Sage; 1993:287-302.
- Teplin LA. The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area Program. Am J Public Health 1990;80:663-9.
- Wallace C, Mullen P, Burgess P, Palmer S, Ruschena D, Browne C. Serious criminal offending and mental disorder. Case linkage study. Br J Psychiatry 1998;172:477-84.
- Teplin LA. The criminality of the mentally ill: a dangerous misconception. Am J Psychiatry 1985;142:593-9.
- Hodgins S. Major mental disorder and crime: an overview. Psychology, Crime and Law 1995;2:5-17.
- Karson C, Bigelow LB. Violent behaviour in schizophrenic patients. J Nerv Ment Dis 1987;175:161-4.
- Walker Z, Seifert R. Violent incidents in psychiatric intensive care unit. Br J Psychiatry 1994:164:826-8.
- Powell G, Cann W, Crowe M. What events precede violent incidents in psychiatric hospitals? Br J Psychiatry 1994;165:107-12.
- Sheridan M, Henrion R, Robinson L, Baxter V. Precipitants of violence in a psychiatric inpatient setting. Hosp Community Psychiatry 1990;41:776-80.
- Johnston EC, Crow TJ, Johnson AL, MacMillan JF. The Northwick Park study of first episodes of schizophrenia. I. Presentation of the illness and problems relating to admission. Br J Psychiatry 1986;148:115-20.
- Binder RL, McNeil DE. Effects of diagnosis and context on dangerousness. Am J Psychiatry 1988;145:728-32.
- Monahan J. Mental disorder and violent behaviour. Perceptions and evidence. Am Psychol 1992;47:511-21.
- Rossi AM, Jacobs M, Monteleone M, Olsen R, Surber RW, Winkler EL, et al. Characteristics of psychiatric patients who engage in assaultive behaviour or other fear-inducing behaviours. J Nerv Ment Dis 1986;174:154-60.
- Modestin J, Ammann R. Mental disorders and criminal behavior. Br J Psychiatry 1995;166:667-75.
- Eronen M, Hakola P, Tiihonen J. Mental disorders and homicidal behaviour in Finland. Arch Gen Psychiatry 1996;53:497-501.
- Chimbos, PD. Marital violence: a study of interspouse homicide. In: Ishwaran K, editor. The Canadian family. 2nd ed. Toronto: Holt, Rinehart and Winston; 1976: 580-99.
- Robbins PC, Monahan J, Silver E. Mental disorder, violence, and gender. Law Hum Behav 2003;27:561-71.
- Clare P, Bailey S, Clark A. Relationship between psychotic disorders in adolescence and criminally violent behaviour. A retrospective examination. Br J Psychiatry 2000;177:275-9.
- Klassen D, O’Connor WA. A prospective study of predictors of violence in adult male mental health admissions. Law Human Behav 1988;12:143-58.
- Fulwiler C, Ruthazer R. Premorbid risk factors for violence in adult mental illness. Compr Psychiatry 1999;40:96-100.
- Swanson J, Swartz M, Estroff S, Borum R, Wagner R, Hiday V. Psychiatric impairment, social contact, and violent behavior: evidence from a study of outpatient-committed persons with severe mental disorder. Soc Psychiatry Psychiatr Epidemiol 1998;33(Suppl 1):S8694.
- Cheung P, Schweitzer I. Correlates of aggressive behaviour in schizophrenia: an overview. Aust N Z J Psychiatry 1998;32:400-9.
- Walsh E, Buchanan A, Fahy T. Violence and schizophrenia: examining the evidence. Br J Psychiatry 2002;180:490-5.
- Wessely SC, Castle D, Douglas AJ, Taylor PJ. The criminal careers of incident cases of schizophrenia. Psychol Med 1994;24:483-502.
- Hodgins S, Mednick SA, Brennan, PA, Schulsinger F, Engberg M. Mental disorder and crime. Evidence from a Danish birth cohort. Arch Gen Psychiatry 1996;53:489-96.
- Swanson JW, Swartz MS, Elbogen EB. Effectiveness of atypical antipsychotic medications in reducing violent behavior among persons with schizophrenia in community-based treatment. Schizophr Bull 2004;30:3-20.
- Junginger J. Predicting compliance with command hallucinations. Am J Psychiatry 1990;147:245-7.
- Junginger J. Command hallucinations and the prediction of dangerousness. Psychiatr Serv 1995;46:911-4.
- Taylor PJ, Garety P, Buchanan A, Reed A, Wessely S, Ray K, et al. Delusions and violence. In: Monahan J, Steadman HJ, editors. Violence and mental disorder: developments in risk assessment. Chicago: University of Chicago Press; 1994:161-82.
- Link BG, Stueve A. Evidence bearing on mental illness as a possible cause of violent behaviour. Epidemiologic Rev 1995;17:172-81.
- Mullen PE. A reassessment of the link between mental disorder and violent behaviour, and its implications for clinical practice. Aust N Z J Psychiatry 1997;31:3-11.
- Wessley S. The epidemiology of crime, violence and schizophrenia. Br J Psychiatry 1997;170(Suppl 32):S8-11.
- Scott H, Johnson S, Menezes P, Thornicroft G, Marshall J, Bindman J, et al. Substance misuse and risk of aggression and offending among the severely mentally ill. Br J Psychiatry 1998;172:345-50.
- Lau JT, Kim JH, Tsui HY. Prevalence, health outcomes, and patterns of psychotropic substance use in a Chinese population in Hong Kong: a population-based study. Subst Use Misuse 2005;40:187-209.
- Eronen M, Angermeyer MC, Schulze B. The psychiatric epidemiology of violent behaviour. Soc Psychiatry Psychiatr Epidemiol 1998;33 (Suppl 1):S13-23.
- Estroff SE, Swanson JW, Lachicotte WS, Swartz M, Bolduc M. Risk reconsidered: targets of violence in the social networks of people with serious psychiatric disorders. Soc Psychiatry Psychiatr Epidemiol 1998;33(Suppl 1):S95-101.