Hong Kong J Psychiatry 2008;18:23-7
ORIGINAL ARTICLE
Relationships between Antipsychotic Medication and Anthropometric Measurements in Patients with Schizophrenia Attending a Psychiatric Clinic in Malaysia
透過一間馬來西亞精神科診所的精神分裂症患者,檢視抗精神病療程與人體測量數據的關係
O Ainsah, R Salmi, CB Osman, AS Shamsul
Dr O Ainsah, MD, MMed (Psy), PhD, Department of Psychiatry, Faculty of Medicine, Hospital Universiti Kebangsaan Malaysia, Jalan Tenteram, 5600, Ceras, Kuala Lumpur, Malaysia.
Dr R Salmi, MD, MMed (Psy), Unit of Psychiatry, Universiti of Technology Mara, Shah Alam, Selangor, Malaysia.
Dr CB Osman, MD, MMed (Psy), Department of Psychiatry, Faculty of Medicine, Hospital Universiti Kebangsaan Malaysia, Jalan Tenteram, 5600, Ceras, Kuala Lumpur, Malaysia.
Dr AS Shamsul, MD, McommHealth (Epidemiology and Statistics), Department of Community Health, Faculty of Medicine, Hospital Universiti Kebangsaan Malaysia, Jalan Tenteram, 5600, Ceras, Kuala Lumpur, Malaysia.
Address for correspondence: Dr Omar Ainsah, Department of Psychiatry, Faculty of Medicine, Hospital Universiti Kebangsaan Malaysia, Jalan Tenteram, 5600, Ceras, Kuala Lumpur, Malaysia.
Tel: 03 9170578; Fax: 03 91737841; E-mail: ainsah@mail.hukm.ukm.my
Submitted: 30 July 2007; Accepted: 23 October 2007
Abstract
Objective: To examine the relationship between antipsychotic use and obesity among patients with schizophrenia.
Participants and Methods:This is a cross-sectional study. Patients who fulfilled the Diagnostic and Statistical Manual of Mental Disorders (4th edition) diagnosis of schizophrenia were included in this study. Demographic profiles and antipsychotic-related factors, including types of antipsychotic and concomitant drugs used, and duration of treatment, were obtained. Anthropometric measurements such as body mass index and waist circumference were measured and classified according to the body mass index and waist circumference classification for Asian populations proposed by the World Health Organization.
Results:Sixty three (64.9%) and 34 (35.1%) patients were receiving atypical and conventional antipsychotics respectively. Twenty (20.6%) patients were being prescribed concomitant conventional depot antipsychotics. The prevalence of being overweight or obese (body mass index: > 23.0 kg/m2) was 71.4% (n = 45) for the atypical antipsychotics group and 79.4% (n = 27) for the conventional antipsychotics group. A large waist circumference was associated with treatment with atypical antipsychotics (p < 0.05) and concomitant conventional depot antipsychotics (p < 0.05). The duration of treatment with clozapine correlated inversely with patients' waist circumferences (r = –0.66, p = 0.04), and there was a positive correlation between duration of treatment and waist circumference in patients on olanzapine (r = 0.45, p = 0.03).
Conclusion:Obesity is highly prevalent among patients with schizophrenia. A high waist circumference is related to the types of antipsychotic medications prescribed and concomitant use of conventional depot antipsychotics. These findings suggest schizophrenic patients are at higher risk of developing obesity-related physical illnesses.
Key words: Anthropometry; Antipsychotic agents; Obesity; Schizophrenia; Weight gain
摘要
目的:分析精神分裂症患者使用抗精神病藥與肥胖症的關係。
參與者與方法:本橫斷面研究對象為根據<<心理疾病診斷統計手冊(第四版) >>診斷患有精神分裂症的病者;收集人口統計學資料與抗精神病相關的治療因素,包括使用抗精神病藥和伴隨藥物的類型和治療時間,以及有關人體數據,例如體重指數(BMI)和腰圍,並以世界衛生組織對亞裔人口BMI和腰圍的指引作出分類。
結果:63名(64.9% )和34名(35.1 %)患者各自接受非典型和典型的抗精神病藥治療。20名(20.6% )患者獲處方伴隨典型抗精神病藥。接受非典型抗精神病藥的一組,超重或肥胖症的現患率(BMI > 23.0 kg/m2) 為71 .4% (n = 45) ,而接受典型抗精神病藥的一組,現患率則為79.4% (n = 27)。腰圍較大與服用非典型抗精神病藥(p < 0.05) 和伴隨典型常規抗精神病長效注射藥(p < 0. 05) 呈正相關;以氯氮平治療的時間與患者腰圍呈負相關(r=0.006,P =0.004) ,但以奧氮平治療的時間與患者腰圍則呈正相關(r= 0.45, P = 0.03)。
結論:精神分裂症患者容易導致肥胖症。腰圍大與服用抗精神病藥物的類型和伴隨便用典型常規抗精神病長效注射藥有關。研究結果顯示,精神分裂症病人患有與肥胖症相關病症的風險較高。
關鍵詞:人體測量學、精神病藥劑、肥胖症、精神分裂症、重量增加
Introduction
Antipsychotic medications, particularly new generation atypical antipsychotic medications, are reportedly associated with higher risks of developing obesity.1 New generation antipsychotic medications cause weight gain, adversely affecting glucose and lipid metabolism and putting patients at greater risk of developing obesity-related diseases.1,2
It has been reported that weight gain affects compliance and causes relapses.3-5 A review suggests that 40 to 80% of patients taking antipsychotic medications experience weight gain exceeding their ideal body weight by 20% or greater.6 Patients with schizophrenia taking conventional antipsychotics have been found to have more than 3 times as much intra-abdominal fat as controls matched for age, gender, and lifestyle.7 Among conventional antipsychotics, the weight gain associated with chlorpromazine and thioridazine has been well described, whereas the high- potency typical antipsychotic medications, such as haloperidol and fluphenazine, have had fewer weight- inducing effects reported.8,9
This study aimed to examine the relationship between obesity and antipsychotic prescription patterns, including the types of antipsychotics prescribed, concomitant use of depot conventional antipsychotics, antidepressants and the duration of the current antipsychotic treatments being used by patients with schizophrenia.
Methods
Subjects
This study was conducted at the Psychiatric Outpatient Clinic, Hospital Universiti Kebangsaan Malaysia (HUKM). Participants’ diagnoses were reviewed by researchers (postgraduate psychiatric trainees and consultant psychiatrists) using the Structured Clinical Interview for DSM-IV Axis I Disorder.10 Inclusion criteria required that patients were able to give informed consent, were aged between 18 and 60 years, had been on antipsychotics for at least 1 month and had adequate command and understanding of either Malay or English and were literate in one or other language. Patients who were intellectually subnormal or had marked cognitive deficits, dementia, substance dependence, medical conditions such as Cushing’s disease, polycystic ovarian syndrome, hypothyroidism, severe oedema, pregnancy, or were receiving other medication that could contribute significantly to weight change, e.g. steroids, insulin, orlistat, sibutramine, duromine, oestrogen and had a body mass index (BMI) of < 18.5 kg/m2 were excluded.
Those who were able to give consent, fulfilled the study selection criteria, and met the diagnostic criteria for schizophrenia were enrolled in this study. Demographic data and drug factors i.e. types of antipsychotic medication, concomitant depot medication, antidepressants, and duration of current treatment, were obtained using a clinical interview, medical record / case notes and the HUKM E- prescribing system (an electronic system with information on drugs prescription, appointments, and doctors in-charge). Patients’ body weights, heights, and waist circumferences were also measured.
Measurements
The BMI and waist circumference (WC) were classified according to the Malaysian Practice Guideline in Management of Obesity (BMI classification for Asian populations proposed by the World Health Organization, 200411—BMI: 18.5-22.9 kg/m2 as normal weight, 23- 27.4 kg/m2 as overweight, > 27.5 kg/m2 as obese; WC: > 90 cm in males as high, > 80 cm in females as high). This classification was adopted because Asian populations are at higher risk of developing health problems at a lower BMI and have a higher body fat percentage than non-Asians.11,12 These BMI classifications are based on measurements proposed by analysing measurements of Asian populations as Asians are at higher risk of developing obesity-related problems.12,13
Informed consent was obtained after the research procedures were fully explained to the subjects. Ethics approval was obtained from the Ethics Committee, HUKM.
Statistical Analysis
Antipsychotic medication prescribing patterns, social demographic profiles, and anthropometric measurements were analysed. The Chi-square test was used to compare the difference between groups of categorical data, while the parametric data were analysed using the t test (for normally distributed data) and Mann Whitney U test (for non-normally distributed data) to calculate the difference between two groups. Analysis of variance test was used to examine the difference among 3 groups of variables with normally distributed continuous data. Pearson correlation and Spearman correlation were used to examine the correlation between two continuous variables which were normally and non-normally distributed. Statistical significance was set at the p value of ≤ 0.05.
Results
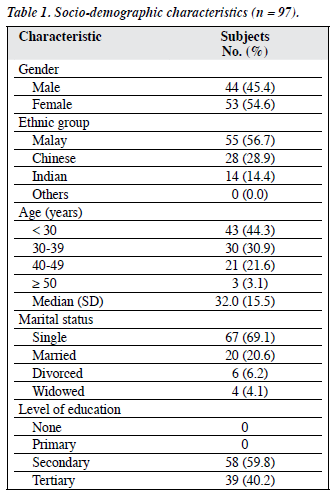
Of 174 potential subjects identified, 97 (73.3%) fulfilled the inclusion criteria and participated in this study. Their socio- demographic data are shown in Table 1.
Antipsychotic Medication Patterns
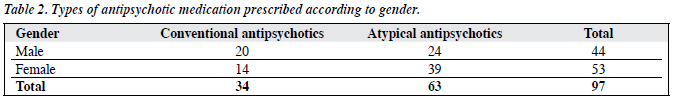
Sixty three (64.9%) patients received atypical antipsychotics and 34 (35.1%) received conventional antipsychotics (Table 2). Twenty (20.6%) patients received concomitant conventional depot antipsychotics while 23 (23.7%) received concomitant antidepressants. None had concomitant mood-stabilising treatments and none received more than 1 antipsychotic medication. Other medications prescribed concomitantly included anti-cholinergics (n = 30, 30.9%), benzodiazepines or zolpidem (n = 21, 21.6%). Twenty four (24.7%) male patients and 39 (40.2%) female patients received atypical antipsychotics, whilst 20 (20.6%) male patients and 14 (14.4%) female patients received conventional antipsychotics (Table 2). There was no significance gender difference (Chi-square = 3.83, p = 0.50) in the types of antipsychotic medications prescribed. The median age for subjects treated with typical antipsychotics (n = 34) was 34.29 (SD, 9.3) years while that for patients treated with atypical antipsychotics (n = 63) was 32.95 (SD, 8.99) years but this difference was not significant (t = 0.69, p = 0.49).
Antipsychotic Medication and Anthropometric Measurements
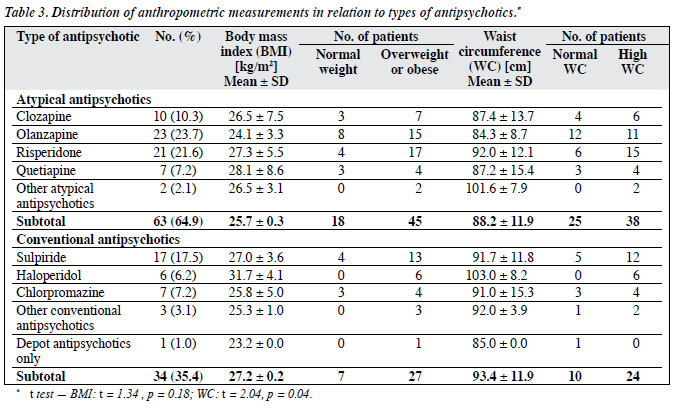
Of the 63 patients taking atypical antipsychotic medication, 45 (71.4%) were either overweight or obese, and 38 (60.3%) had high WC. Similar results were found in those receiving conventional antipsychotics; 27 (79.4%) respondents were either overweight or obese, and 24 (70.6%) had high WC. The mean BMI for patients taking atypical and conventional antipsychotics were 25.7 (SD, 0.3) kg/m2 and 27.2 (SD, 0.2) kg/m2 respectively, however the difference was not significant (t = 1.34, p = 0.18). The mean WC for patients taking atypical and conventional antipsychotic medication were 88.2 (SD, 11.9) cm and 93.4 (SD, 11.9) cm respectively. There was a significant difference between these two means (t = 2.04, p = 0.04) [Table 3]. Twenty three (23.7%) respondents were receiving concomitant antidepressants. There was no significant difference between the WC and BMI of those receiving concomitant antidepressants and those not receiving concomitant antidepressants (WC: χ2 = 0.00, p = 0.97, BMI: χ2 = 1.31, p = 0.25).
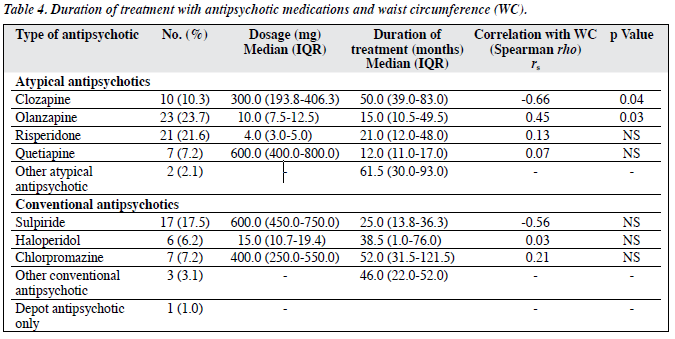
Post-hoc analysis of the duration of use of each type of antipsychotic and its correlation with WC showed that the WC of patients receiving olanzapine (n = 23, rs = 0.45, p = 0.03) was positively related to the duration of use, while the duration of use of clozapine (n = 10, rs = –0.66, p = 0.04) was inversely related to WC (Table 4). There were 20 (20.6%) patients being treated with combinations of depot antipsychotics. Seventeen (85%) had high WC. There was a significant difference between the WC of those being treated with a combination of depot antipsychotics and those not receiving this treatment (χ2 = 4.86, p = 0.03) but this effect was not dose-related. The dosage of depot flupenthixol decanoate prescribed did not correlate with BMI (p = 0.48, rs= 0.18) and WC (p = 0.51, rs = 0.17). Only two respondents received depot fluphenazine decanoate.
Discussion
Obesity is highly prevalent among patients with schizophrenia. This issue needs to be addressed seriously. The different types of antipsychotic medication being prescribed appear to have different effects on WC. Patients treated with atypical antipsychotics, clozapine and olanzapine, had high WC. This may increase their risk of developing obesity and obesity-related physical illnesses.13,14 Different drugs may cause different degrees of weight gain. Atypical antipsychotic medications, such as olanzapine and clozaril, are associated with a high risk of acquiring metabolic syndrome.15 It would be better to avoid drugs which induce marked weight gain unless there is no other choice or to only use them to treat patients with low body weights as this side-effect may be helpful.
Patients being given concomitant depot antipsychotics had significantly higher WC, suggesting that conventional depot antipsychotics are associated with obesity. A survey of 226 patients attending depot neuroleptic clinics found the prevalence of obesity in this group was 4 times higher than
that of the general population.16 The duration of the index drug treatment correlated with WC positively for olanzapine and inversely with clozapine, suggesting that patients being treated with clozapine may gain weight initially but that their weight will be reduced with time. Olanzapine induced weight gain but due to the short duration of olanzapine treatment in the patients in this study, it is difficult to comment on its long-term effects.
In this study, BMI and WC were classified according to Malaysian Practice Guideline in Management of Obesity (BMI classification for Asian populations proposed by the World Health Organization, 2004).11 This classification is adopted as Asian populations are at higher risk of developing health problems at lower BMI and have higher body fat percentage than non-Asians.17,18 This classification is very helpful clinically for detecting obesity at an early stage, enabling maximisation of health outcomes for schizophrenic patients.
Obesity is highly prevalent among patients with schizophrenia, increasing their risk of developing obesity- related physical illnesses. As different antipsychotic medications may affect body weight differently, the choice of antipsychotics should be tailored according to the needs of individual patients. Baseline and regular monitoring of body weight, BMI, WC, and metabolic measures, i.e. fasting blood sugar, lipid profile, should be considered routine investigations especially among patients being treated with atypical drugs like olanzapine and clozapine. Psycho-education, emphasising a healthy lifestyle including an exercise programme, should be given to every patient. Weight reduction programmes should be included as part of the treatment for schizophrenic patients with obesity. A case-controlled prospective study over a longer period of treatment would be helpful for examining the impact of antipsychotic treatments on patients’ anthropometric measurements and for controlling other variables.
References
- American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, and North American Association for the Study of Obesity; 2004.
- Mackin P, Watkinson HM, Young AH. Prevalence of obesity, glucose homeostasis disorders and metabolic syndrome in psychiatric patients taking typical or atypical antipsychotic drugs: a cross-sectional study. Diabetologia 2005;48:215-21.
- Berken GH, Weinstein DO, Stern WC. Weight gain. A side-effect of tricyclic antidepressants. J Affect Disord 1984;7:133-8.
- Bernstein JG. Induction of obesity by psychotropic drugs. Ann NY Acad Sci 1987;499:203-15.
- Weiden PJ, Mackell JA, McDonnel DD. Obesity as a risk factor for antipsychotic noncompliance. Schizophr Res 2004;66:51-7.
- Green AI, Patel JK, Goisman RM, Allison DB, Blackburn G. Weight gain from novel antipsychotic drugs: need for action. Gen Hosp Psychiatry 2000;22:224-35.
- Thakore JH. Metabolic syndrome and schizophrenia. Br J Psychiatry 2005;186:455-6.
- Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999;156:1686-96.
- Vanina Y, Podolskaya A, Sedky K, Shahab H, Siddiqui A, Munshi F, et al. Body weight changes associated with psychopharmacology. Psychiatr Serv 2002;53:842-7.
- Diagnostic and statistical manual of mental disorder; DSM IV. Washington DC: American Psychiatric Association; 2000.
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-63.
- Weisell RC. Body mass index as indicator of obesity. Asia Pac J Clin Nutr 2002;11(Suppl 8):S681-4.
- Kissebah AH, Krakower GR. Regional adiposity and morbidity. Physiol Rev 1994;74:761-811.
- Hans TS, van Leer EM, Seidell JC, Lean ME. Waist circumference action levels in the identification of cardiovascular risk factors: prevalence study in a random sample. BMJ 1995;311:1401-5.
- Lindenmayer JP, Czobor P, Volavka J, Citrome L, Sheitman B, McEvoy JP, et al. Changes in glucose and cholesterol levels in patients with schizophrenia treated with typical or atypical antipsychotics. Am J Psychiatry 2003;160:290-6.
- Silverstone T, Smith G, Goodall E. Prevalence of obesity in patients receiving depot antipsychotics. Br J Psychiatry 1988;153:214-7.
- Deurenberg-Yap M, Schmidt G, van Staveren WA, Deurenberg P. The paradox of low body mass index and high body fat percent among Chinese, Malays and Indians in Singapore. Int J Obes Relat Metab Disord 2000;24:1011-7.
- He M, Tan KC, Li ET, Kung AW. Body fat determination by dual energy X-ray absorptiometry and its relation to body mass index and waist circumference in Hong Kong Chinese. Int J Obes Relat Metab Disord 2001;25:748-52.