Hong Kong J Psychiatry 2008;18:62-8
Original Article
Symptom Presentation in Patients with Acute Schizophrenia: Comparison in Three Major Malaysian Ethnic Groups
急性精神分裂症患者的臨床徵狀:馬來西亞三個族群的比較
O Ainsah, H Nurulwafa, CB Osman
Dr O Ainsah, MD, MMed (Psy), PhD, Department of Psychiatry, Universiti Kebangsaan Malaysia, Malaysia.
Dr H Nurulwafa, MD, MMed (Psy), Department of Psychiatry, Malacca Hospital, Malaysia.
Dr CB Osman, MD, MMed (Psy), Department of Psychiatry, Universiti Kebangsaan Malaysia, Malaysia.
Tel: 6-03 9170 2590; Fax: 6-03 9173 7841; E-mail: ocbaaaah@yahoo.com.my
Submitted: 14 September 2007; Accepted: 7 December 2007 62 © 2008 Hong Kong College of Psychiatrists
Abstract
Objective: This cross-sectional study was conducted to examine the difference in presenting symptoms among Malay, Chinese, and Indian patients with schizophrenia, who were admitted to the psychiatric wards of Hospital Kuala Lumpur, Malaysia.
Participants and Methods: This study was conducted between 13 March 2004 and 13 June 2004. The Structured Clinical Interview for DSM-ITI-R (SCID) to generate DSM-N diagnoses was used to diagnose schizophrenia, and Positive and Negative Syndrome Scale (PANSS) was used to compare differences in presenting symptoms among the 3 ethnic groups. A total of 97 patients were recruited; 49% were Malay, 28% Chinese, and 24% Indian.
Results: There were no significant differences among the 3 ethnic groups with regard to the demographic factors except the level of education; more Malays had tertiary education than Chinese and Indians (p < 0.04). In this study, the PANSS score on emotional withdrawal was high among Indians (p < 0.03), and on passive I apathetic social withdrawal and stereotyped thinking were low among Malays (p < 0.002 and p < 0.001 respectively). The scores on tension and active social avoidance were also high among Indians as compared to the Malays (p < 0.02 in both). There was a significant reduction of the total PANSS score over 2 weeks, no difference was noted for the mean change of total PANSS score from baseline, i.e. 'on admission' to 'at week 2' among the 3 ethnic groups. A significant difference was observed in the mean PANSS positive scores, whereby reduction of the positive symptoms was greatest in Malays and least in Chinese (p < 0.004).
Conclusion: A sizable proportion of children in this secondary school population potentially suffered from depression. Psychological interventions are needed to ease this burden and ensure their well-being.
Key words: Ethnic groups; Schizophrenia; Signs and symptoms
摘要
目的:本橫斷面研究的對象為入住馬來西亞吉隆坡中央醫院精神病房,分別為馬來藉、華藉,以及印度藉的精神分裂症患者,為找出他們臨床症狀的不同。
參與者與方法: 2004年3月13 日至2004年6月13 日期間,使用DSM-III-R定式臨床會診量表(SCID)組織得出的DSM-IV診斷精神分裂症狀,並使用「陰性和陽性症狀量表」(PANSS) 比較三個族群間臨床症狀的不同。共97位病人參與此研究;其中49%屬馬來藉、28%華藉、24%印度藉。
結果:三個族群中,除教育程度外,其他人口因素無顯著差異; 其中有較多馬來藉病人有大學教育程度(p < 0.04) 。印度藉病人在情感退縮方面PANSS得分較高(p< 0.03) ,而馬來藉病人在被動/冷漠社交退縮方面(p < 0 . 002) 和固執思維(p < 0.001 )方面均較其餘兩個族群低。至於緊張(p < 0. 02) 和主動社交迴避(p < 0.02) 方面,印度藉病人較馬來藉病人的PANSS得分為高。兩週後的PANSS總得分有明顯減少。三個族群中,入院時和兩過後的PANSS平均總得分的差異無顯著性。陽性症狀量表的平均得分有顯著差異,陽性症狀的減少在馬來藉病人中最多,而在華藉病人中最少(p < 0. 004) 。
結論:陽性症狀方面,三組間的差異無顯著性,但部份的陰性症狀,三組間的差異顯著。
關鍵詞:族群、精神分裂症、症狀
Introduction
Malaysia’s population has many ethnic groups, the 3 major ones being Malay (58%), Chinese (24%), and Indian (8%). Before the country became independent in 1957, the Malays largely resided in rural areas, while the Chinese and the majority of the Indians were urban dwellers. There were fairly distinct differences between the group members in terms of economic and social positions achieved. The Chinese have historically played an important role in trade and business. Most are descendents of immigrants from the south coastal provinces of China. The Indian community in Malaysia is the smallest among the 3 main ethnic groups. For statistical purposes, those of Punjabi and Sri-Lankan origin are also included in the ‘Indian’ category. Hindu traditions remain strong in the Indian community of Malaysia.
One study examined symptoms in schizophrenia patients among White and African-Caribbeans living in Britain.1 Factor analysis was applied to symptom data obtained by the Present State Examination from the 2 groups of patients and identified 6 symptoms dimensions: mania, depression, first-rank delusions, other delusions, hallucinations, and a manic / catatonic category.1 There were no differences between White and African-Caribbean patients with schizophrenia in terms of core symptoms of the disorder, but the African-Caribbean patients appeared to present with more symptoms of a mixed affective nature.1
Results of a local study suggested that the symptoms of schizophrenia are influenced by culture.2,3 Phenomenology of hallucinatory experiences among Chinese patients from a predominantly Chinese area of Malaysia (Penang state) was compared with Malay patients from a predominantly Malay area (Kelantan state). Most Malays heard voices that they attributed to God, demons or spirits, while the Chinese attributed them to friends, relatives, or neighbours. However, Chinese brought up in Malay communities had auditory hallucination like their Malay counterparts. Regarding phenomenological differences in delusions between schizophrenia patients of the 2 cultures of Malays, it was found that 70% presented with persecutory delusions, which was the most common type of delusion.4 These findings were consistent with those of others.5-7
Understanding presenting symptoms may help in the diagnosis and treatment of patients with acute schizophrenia.8
Thus, the objective of this study was to examine the presenting symptoms among patients suffering from acute schizophrenia in the 3 ethnic groups. To have comprehensive evaluation of schizophrenic symptomatology, positive and negative symptoms, as well as general psychopathology, were examined.
Methods
This study was conducted in the psychiatric wards of Hospital Kuala Lumpur, which is the only hospital with a gazetted psychiatric unit in Kuala Lumpur that takes care of mental patients in need of inpatient care. The hospital functions as a tertiary hospital and provides mental health services to the population of Klang Valley. This was a cross-sectional study using interviewer-rated questionnaires, carried out on admission and 2 weeks thereafter. The interviews took place at the psychiatric wards of the hospital from 13 March 2004 to 13 June 2004.
Subjects
A consecutive series of schizophrenia patients admitted to the hospital were recruited. To reduce the risk of type 2 errors, the sample size was calculated, using Epi-info
(Version 6) software, where alpha is equivalent to 95%, 1-beta is equivalent to 80%, the expected frequency based on the prevalence study on hallucinations in schizophrenia patients9 was 76%, and the worst acceptable result was 85%. Based on these figures, a necessary sample size of 86 was estimated.
Inclusion criteria included patients with schizophrenia who were aged between 18 and 64 years. They were diagnosed using Structured Clinical Interview for DSM- III-R (SCID)10 for DSM-IV11 diagnoses and must be able to understand Malay or English. The exclusion criteria included patients with diagnosis of mental retardation, organic psychotic conditions or substance abuse, and who were not in the acute phase of schizophrenia.
Assessment
All patients admitted to the psychiatric wards of the hospital were registered. The investigator used a SCID to ascertain the clinical diagnosis of schizophrenia, after having received appropriate training by a senior consultant psychiatrist who was well versed with the diagnostic instruments. Prior to the study, the investigator used the diagnostic instrument on 10% of the subjects, where the section on Psychotic Screening and Mood Syndrome were used. These subjects were then independently re-rated by the supervisor. The kappa (κ) value was 1 indicating good inter-rater agreement. For those who fulfilled the entry criteria for the study, written informed consent was obtained either from the patient or from a guardian.
A semi-structured format was used to gather demographic data from patients, their reliable informants, and clinical records. Patients were assessed using the Positive and Negative Syndrome Scale (PANSS)12 within 3 days (72 hours) of admission (on admission), so that all of them were in the acute phase of their illness. Patients were admitted to the ward either as newly diagnosed patients with a first episode or as relapsed cases. Those patients who could not respond to the questions (owing to severe psychotic features, being mute or uncooperative) were retested on 2 separate occasions and were excluded if no information could be obtained after 3 attempts. Subjects were reassessed using PANSS after 2 weeks (at week 2) to examine their post-drug treatment status.
Statistical Analyses
Differences in proportions were tested with the Chi-square test, and analysis of variance (ANOVA) was used to examine for differences among the 3 groups with respect to normally distributed continuous data. Because positive and negative symptoms are probably influenced by several independent variables, we chose to use a multivariate approach in our analysis. The independent variables were demographic measures, such as age, ethnicity, education level, marital status, and employment. Data analysis (descriptive and analytic) was performed using the Statistical Package for Social Studies (SPSS) Windows version 10.0. This research project was approved by the Medical Research and Ethics Committee, Faculty of Medicine, Universiti Kebangsaan Malaysia.
Results
A total of 203 patients with a diagnosis of schizophrenia were admitted and screened during the study period. Ninety seven (48%) were recruited as subjects. Subjects were not included in the study for various reasons — 36 (18%) refused consent, 21 (10%) had problems communicating in English or Malay, 20 (10%) had co-morbid diagnoses (epilepsy, mental retardation, and substance abuse), 12 (6%) were of other ethnic groups, 12 (6%) were discharged before assessment, and 5 (2%) were not in the acute phase of their illness (having been admitted for social reasons). Among the 97 patients who fulfilled the diagnostic criteria of schizophrenia of DSM-IV, 84 (87%) were seen during the second interview (week 2). Of the 13 non-respondents, 5 patients were Malay, 5 were Chinese, and 3 were Indian; 5 were sent to Hospital Bahagia before their week-2 assessment, 8 patients defaulted follow-up after home leave or were discharged. Phone calls to contact these 8 patients were of no avail.
Socio-demographic Characteristics
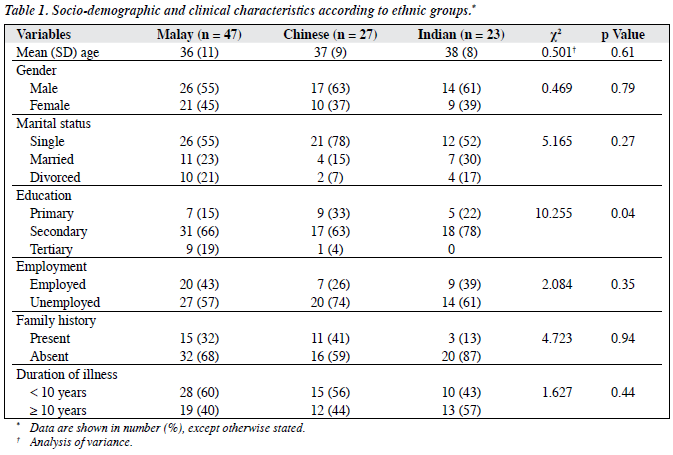
Eight (8%) subjects were admitted for the first time, 22 (23%) had a prior admission. The majority, 67 (69%), had two or more admissions prior to the index admission (Table 1).
Psychiatric Symptomatology
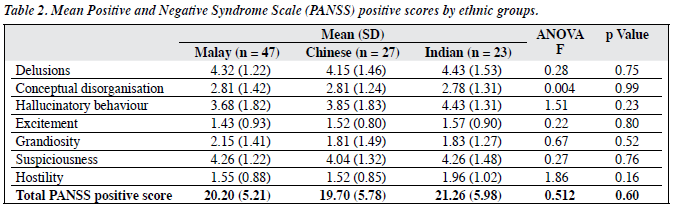
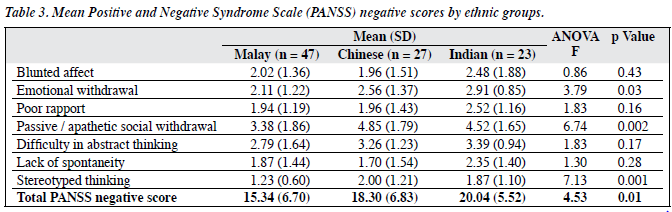
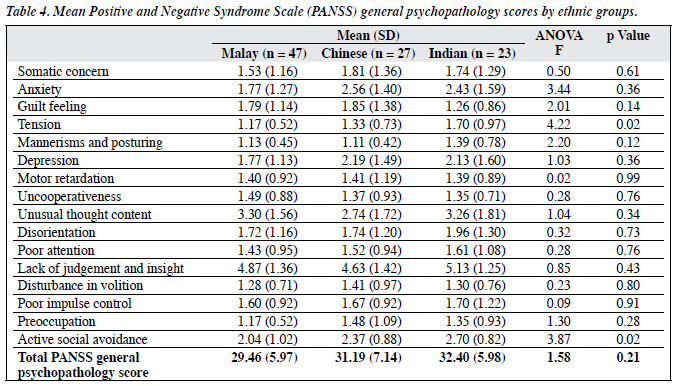
There were no significant differences in the mean PANSS positive scores among different ethnic groups (Table 2). In all ethnic groups, mean scores were higher for delusions, hallucinatory behaviour, and suspiciousness when compared to conceptual disorganisation, excitement, grandiosity, and hostility. There were statistically significant differences in the emotional withdrawal, passive / apathetic social withdrawal, and stereotyped thinking among Malays, Chinese, and Indians (Table 3). Post-hoc multiple comparisons revealed significant difference between Malays and Indians in emotional withdrawal (p = 0.03); significant differences were noted between Malays and Chinese (p = 0.003) and Malays and Indians (p = 0.04) for passive / apathetic social withdrawal. For stereotyped thinking, there was also a significant difference between Malays and Chinese (p = 0.003), and between Malays and Indians (p = 0.02). There were no statistically significant differences in terms of general psychopathology among the different ethnic groups, except for tension (p = 0.02) and active social avoidance (p = 0.02) [Table 4]. Post-hoc comparison revealed that for both symptoms, the significant differences were evident between Malays and Indians (p = 0.01 and p = 0.02 respectively) whereby the Indians scored higher than the Malays. Highest mean scores were noted for lack of judgement and insight across all ethnic groups.
Changes in Psychopathology after Two Weeks
There was a significant reduction of the total PANSS general psychopathology score at week 2 among the 3 ethnic groups, from 29.46 to 15.32, 31.19 to 16.03, and 32.40 to 16.20 respectively in the Malays, Chinese, and Indians; no significant difference was noted. However, there was a significant change in the mean PANSS positive scores from baseline to week 2 among the 3 ethnic groups (p = 0.01). Post-hoc comparison indicated a significant difference between Malays and Chinese (p = 0.004). The reduction of the positive symptoms was greatest in Malays and least in the Chinese.
Multivariate Linear Regression Analysis
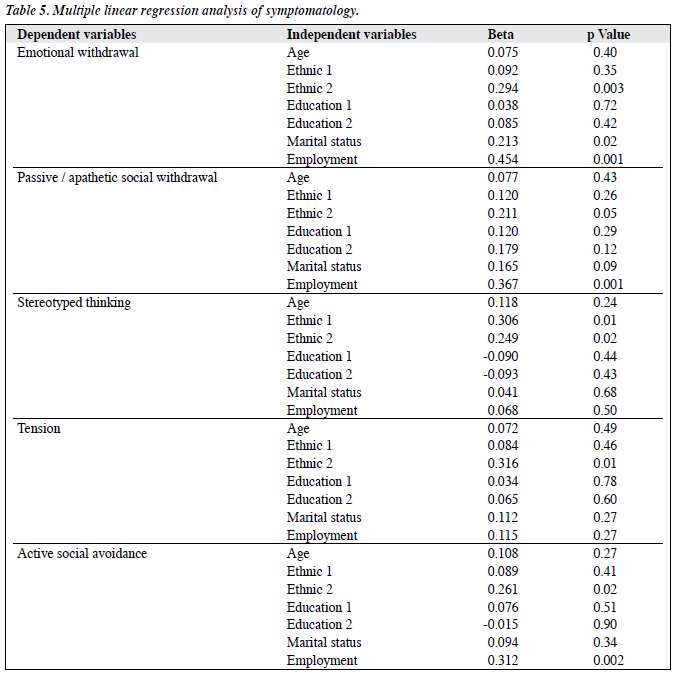
To evaluate any influence of education levels and demographic characteristics on symptom presentation, a multivariate linear regression analysis was carried out (Table 5). Education levels and ethnic factors were grouped into 2 categories, dummy coding was used to create 2 ethnic and 2 education level variables. ‘Ethnic 1’ represented the mean difference between Chinese and Malay and ‘Ethnic 2’ referred to the mean difference between Indian and Malay.
‘Education 1’ represented the mean difference between the secondary and primary education level whereas ‘Education 2’ represented the mean difference between the tertiary and primary education level. Multivariate linear regression analysis was carried out repeatedly for 5 symptom variables for which cross-ethnic differences had been found (emotional withdrawal, passive / apathetic social withdrawal, stereotyped thinking, tension, and active social avoidance). The analysis showed that ethnic group influenced the symptom presentation significantly. However, marital status significantly influenced emotional withdrawal (p < 0.02) and employment influenced emotional withdrawal, passive / apathetic social withdrawal, and active social avoidance (p < 0.001, p < 0.001, and p < 0.002 respectively) [Table 5].
Discussion
The results showed that the scores for delusions, hallucinatory behaviour, and suspiciousness were high, and might have been the reason the patients were admitted. This is consistent with the findings from a local and other studies.9,13 There was no significant difference in the positive symptoms among Malay, Chinese, and Indian. A previous study also found there were no differences in the positive symptoms among Malay and Chinese.13 The positive symptoms, particularly delusions and hallucinations, were assessed based on the severity, but not specifically for the content of delusions or hallucinations.4 The local study undertaken in Penang and Kota Bharu2 found that the content of hallucinations in schizophrenia was influenced by the culture of the patients. The authors reported that Kota Bharu Malay patients had more hallucinations associated with religious content and experienced more visual hallucinations than Penang Chinese and Kota Bharu Chinese. The other study4 also noted that persecutory delusions were the most common, and that grandiose delusions were less common among the Kelantan Chinese. Kelantan Malay patients were deluded about having power and wealth, while the Penang Malay and Chinese patients had grandiose delusions regarding high social status.4
Although there was no difference in the mean PANSS positive score among the 3 ethnic groups, there were differences in negative symptoms among them. There were statistically significant differences in the emotional withdrawal, passive / apathetic social withdrawal, and stereotyped thinking among the Malays, Chinese, and Indians. Indians scored higher compared to the Malays in emotional withdrawal, whilst the Malays scored lower for passive / apathetic social withdrawal and stereotyped thinking compared to the Chinese and Indians.
Tension and active social withdrawal scores were also noted to be significantly higher in Indians compared to other ethnic groups. This could be because Indians could be considered as Caucasians, whilst the Chinese and Malays are considered as Mongoloid.14,15 These differences in psychopathology may reflect differences in both cultural and constitutional predispositions.
Of particular interest was on ‘lack of judgement and insight’. These patients experienced impaired awareness or understanding of their own psychiatric condition and life situation, as evidenced by failure to recognise past or present psychiatric illness or symptoms, denial of the need for psychiatric hospitalisation or treatment, and decisions characterised by poor anticipation of consequences and unrealistic short-term and long-term planning. From these results, lack of judgement and insight scored highest among all subjects. As pointed out by Johnson and Orrell,6 patients may disagree with doctors’ views that they are ill. This may be because of the illness itself, but also because they hold views about the nature of mental illness that differ from medical views.16 Likewise, mental illness may have particularly unpleasant connotations within their cultures, and denial may be a way of coping with the stigma.17-19
Multivariate linear regression analysis revealed that ethnicity influenced the symptom presentations. The results also showed marital status influenced the emotional withdrawal, while the employment significantly influenced the emotional withdrawal, passive / apathetic social withdrawal, and active social avoidance. There are several important limitations to this study that should be considered when interpreting the results. The sample size was rather small, especially for comparison of 3 ethnic groups. The limited sample size was due to the short duration of the study, as well as the strict inclusion and exclusion criteria. The study was carried out only on hospitalised inpatients, which might introduce a bias towards the more severe end of the illness spectrum. The study was carried out in Hospital Kuala Lumpur, which is a tertiary centre, and so findings may not be applicable to the general population. The subjects were only seen on admission and in the second week. In future, it might be helpful to conduct a prospective longitudinal study, where the post-treatment status is assessed over longer periods of time, as this would enable examination of associations between symptomatology and the outcomes.
In conclusion, this study provided preliminary comparative findings about presenting symptoms among Malay, Chinese, and Indian patients with acute schizophrenia in Kuala Lumpur. Differences in some dimensions of negative symptoms may provide useful insights for planning of rehabilitation with special needs for different ethnic groups.
Acknowledgements
The authors thank the director of Hospital Kuala Lumpur, staff of the Department of Psychiatry and participants in the study.
References
- Hutchinson G, Takei N, Sham P, Harvey I, Murray RM. Factor analysis of symptoms in schizophrenia: differences between White and Caribbean patients in Camberwell. Psychol Med 1999;29:607-12.
- Azhar MZ, Varma SL, Hakim HR. Phenomenological differences of hallucinations between schizophrenic patients in Penang & Kelantan. Med J Malaysia 1993;48:146-52.
- Azhar MZ. Mental illness and Malay culture: a study of Kelantan Malays. In: Haque A, editor. Mental health in Malaysia: issues and concerns. Kuala Lumpur: University of Malaya Press; 2001.
- Azhar MZ, Varma SL, Hakim HR. Phenomenological differences of delusions between schizophrenic patients of two cultures of Malaysia. Singapore Med J 1995;36:273-5.
- Burchard EG, Ziv E, Coyle N, Gomez SL, Tang H, Karter AJ, et al. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med 2003;348:1170-5.
- Johnson S, Orrell M. Insight, psychosis and ethnicity: a case-note study. Psychol Med 1996;26:1081-4.
- Liddle PF, Ngan ET, Duffield G, Kho K, Warren AJ. Signs and Symptoms of Psychotic Illness (SSPI): a rating scale. Br J Psychiatry 2002;180:45-50.
- Lefley HP. Culture and chronic mental illness. Hosp Community Psychiatry 1990;41:277-86.
- Small IF, Small JG, Andersen JM. Clinical characteristics of hallucinations of schizophrenia. Dis Nerv Syst 1966;27:349-53.
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry 1992;49;624-9.
- 1 Diagnostic and statistical manual of mental disorder. DSM IV. Washington DC: American Psychiatric Association; 2000.
- Kay SR, Opler LA, Lindemayer JP. The Positive and Negative Syndromes Scale (PANSS): rationale and standardisation. Br J Psychiatry Suppl 1989;7:S59-67.
- Norhayati N. Symptomatology of neuroleptic free schizophrenic patients admitted to Hospital Kuala Lumpur [thesis]. Malaysia: Universiti Kebangsaan Malaysia; 2000.
- Tan ES. Prospects of psychiatric research in a multiracial developing community: West Malaysia. Lebra WP, editor. Transcultural research in mental health: volume II of Mental Health Research in Asia and the Pacific. Honolulu: The University Press of Hawaii; 1972.
- Nida EE. Customs and cultures. New York: Harper; 1954.
- Tseng WS. Clinician’s guide to cultural psychiatry. San Diego, CA: Academic Press; 2003.
- Singh SP. Ethnicity in psychiatric epidemiology: need for precision. Br J Psychiatry 1997;171:305-8.
- Perales A. Studies on schizophrenic symptomatology in Peru. Maj M, Sartorius N, editors. Schizophrenia. 2nd ed. WPA Series Evidence and Experience in Psychiatry; 2002.
- Sankar P, Cho MK. Genetics. Toward a new vocabulary of human genetic variation. Science 2002;298:1337-8.