Hong Kong J Psychiatry 2008;18:115-21
ORIGINAL ARTICLE
首發思覺失調患者的幻聽經驗以及應對策略:與壓力應對的關係
Ms Suzanne HW So, MA, MSc, MSSc, Department of Psychology, Institute of Psychiatry, King’s College London, United Kingdom.
CW Wong, PsychD, Clinical Psychology Department, Kwai Chung Hospital, Hong Kong, China.
Address for correspondence: Ms Suzanne HW So, Department of Psychology, PO Box 78, Addiction Sciences Building, 4 Windsor Walk, London SE5 8AF, United Kingdom.
Tel: (44-207) 8485728; Fax: (44-207) 8480860; E-mail: suzanne.so@iop.kcl.ac.uk
Submitted: 9 April 2008; Accepted: 20 May 2008
Abstract
Objective: To investigate subjective experiences and coping with drug-resistant auditory hallucinations in patients with first-episode psychosis, and to compare coping with auditory hallucinations as opposed to general stress.
Participants and Methods: Twenty two patients with first-episode psychosis participated in this study. Characteristics of their voices, beliefs about the voices, coping strategies used for such voices and for general stress were measured, using a semi-structured interview and questionnaires.
Results: Despite active antipsychotic medications, patients on average reported 3 persistent auditory hallucinations. Most found the voices unpleasant and personally relevant, and spontaneously coped with them with modest levels of subjective efficacy. The most frequently adopted strategies were not the most effective ones. Patients reported a broad repertoire of coping for general stress, which included both emotion-focused and problem-focused strategies. People who actively coped with voices also used more coping strategies in reaction to general stress.
Conclusion: Patients with early psychosis commonly interacted with the persistent psychotic symptoms in individually different ways. The way patients coped with residual voices was related to the characteristics of the voices, their symptomatology, as well as general stress coping. Implications for research methodology and psychological interventions were discussed.
Key words: Adaptation, psychological; Auditory perception; Hallucinations; Psychotic disorders; Schizophrenia
摘要
目的:探視首發恩覺失調患者對耐藥性幻聽的主觀經驗和應對,並比較應對幻聽和應對般壓力的策略。
參與者與方法:22位首發思覺失調患者參加了研究。研究應用問卷調查和半結構式面談,量度他們所聽到的聲音特點、他們對這些聲音的看法、應對這些聲音以及般壓力的策略。
結果:儘管施用抗思覺失調藥物積極進行治療,但病人報告持續幻聽的平均值仍然高達3 。大部分患者覺得這些聲音難聽且和個人相關,一聽到就即時處理這些聲音,但主觀上的效力有限。他們最常探用的策略並非是最有效的。患者應對一般壓力的方法非常多,既有情緒為重點的,也有以問題為焦點的,積極處理幻聽聲音的病者在面對般壓力時也會應用更多應對策略。
結論:恩覺失謂的患者通常以自己的方法處理持續的思覺失調症狀。患者應對餘育的方式與聲音的特性、症狀學,以及調適一般壓力的芳法有關。此外,本文亦討論此項研究對研究芳法和心理學介入治療的敢示。
關鍵詞:心理適應、聽覺感知、幻覺、精神異常、精神分裂症
Introduction
Auditory hallucination (AH) is a defining symptom of psychotic disorder. According to Sartorius et al,1 more than 70% of individuals with schizophrenia experienced AH every month. Despite adequate levels of medication being prescribed, voices persist in 25 to 50% of patients.2 Over 75% of persons hearing voices reported being ‘highly distressed’ by the hallucinatory experience.3 Therefore, non-medical intervention for persistent hallucinations is important in the management of the psychotic illness.
Previous studies have shown that 72 to 100% of psychotic patients spontaneously attempted to cope with their AHs (see review by Garcelán and Rodríguez4); mean numbers for their coping strategies ranged from 2.2 to 18.3.5 Using multidimensional scaling techniques, Carter et al6 drew clusters of coping strategies based on frequency of use and efficacy. They reported that the most commonly used strategies include yelling / talking back to the voices, listening to songs / music / radio, talking to someone, and going to sleep. Other commonly employed behavioural strategies included: watching television, going for walks, and participating in sport.4
Inconsistency in the number of coping strategies and their frequency of use is related to the great variety of ways such information is obtained and categorised. It has been shown that participants are more ready to claim a coping strategy when prompted by a list than when asked an open question.7,8 Therefore, using both open questions and a prompt list might elicit more comprehensive information about natural coping.
The most effective coping methods also vary between studies.5 For example, some suggested that humming is a highly efficacious way of coping,6,9 while others argued that direct confrontation, including humming, increases anxiety and the frequency of the voices.7 The latter contend that strategies based on acceptance of the voices and on passive coping (such as ignoring the voices) lead to a reduction in anxiety and better coping.7,10-12
While many studies have shown that effectiveness improves if participants use several strategies at the same time,6,10-11,13 others have argued the converse.14,15 Contradictory findings may be related to different ways of measuring effectiveness. For example, Carter et al6 equated effectiveness with eliminating the voices, whereas Farhall and Gehrke7 considered effectiveness as a multidimensional construct, including a degree of control, anxiety levels, and overall coping effectiveness. As the perceived (or actual) effectiveness of different strategies may differ widely across individuals,16 it is useful to assess effectiveness of coping with voices from the patient’s point of view.
It has been shown that the coping strategies most frequently used are not the most effective; the most effective ones are used only by quite a small proportion of patients.6 The way that patients cope with hallucinations is related to a number of factors. For example, Chadwick and Birchwood17 and Sayer et al18 reported that patients are more likely to engage the voices if they believe that the voices are benevolent, and resist them if they consider them malevolent. With regard to symptomatology, it has been found that positive psychotic symptoms are associated with the use of emotion-oriented coping strategies (strategies targeting the emotions associated with the stressor), whereas negative psychotic symptoms have an inverse relationship with the total number of coping strategies and problem-oriented coping strategies (strategies aiming at problem-solving).19
While many studies investigate the ways psychotic patients cope with psychotic symptoms, less is known about how they cope with the range of stressors encountered in their everyday life. It has been shown that persons with schizophrenia are ineffective and avoid problem-solving.20,21 Macdonald et al22 found that people with early psychosis, who have greater feelings of self-efficacy and perceived social support as well as flexible use of problem-focused coping strategies, appear more likely to cope with day-to- day stressors.
The above studies seem to suggest that psychotic patients often do not cope effectively with AH and general stressors. However, the majority of these studies involved only adult patients with a longer history of schizophrenia. Besides, none compared the coping with hallucinations and general stressors. It is, therefore, not known whether the strategies for coping with AH reflect a general coping style of the patients, or that there is something special about the hallucinatory experiences that lead to a symptom-specific style of coping.
The current study aimed to explore the patterns of coping among patients with first-episode psychosis employed in the face of persistent AHs as well as for general day-to-day stressors. In particular, it looked for answers to the following questions:
- What are the characteristics of patients experiencing persistent AHs?
- What strategies do patients employ to cope with persistent AHs and are they considered effective?
- Are the coping strategies for hallucinations related to various characteristics of the voices and the patient’s belief about the voices?
- Is the style of coping with hallucinations consistent with that used to cope with general stressors?
Methods
Sample
Participants were outpatients with first-episode psychosis, who experienced persistent AHs and were under psychiatric treatment at the Early Assessment Service for Young People with Psychosis (EASY23). This is an early intervention service for younger individuals with first-episode psychosis. Approximately 700 new cases with psychotic disorders received treatment at the EASY Service every year.
Patients were recruited to the study if they were assessed as experiencing persistent AHs by their treating psychiatrists. All participants gave written informed consent to join the study. Patients were not invited to participate if their primary diagnosis was a substance use disorder, mood disorder, or organic mental disorder. Within the 1-year sampling period, 24 patients with first-episode psychosis were invited to participate in this study, 2 of whom reported an absence of AHs by the time of assessment. Hence, 22 patients were included in the final analysis. This sample was representative of the clinical population within the EASY Service.
Measures
This study adopted a simple cross-sectional design, using the following clinical measures and self-reporting questionnaires.
Semi-structured Interview Schedule
This schedule was designed by the authors to tap into various aspects of AHs, such as duration, volume, emotional relevance, relationship with the voices, as well as coping strategies in response to the voices. Some of the questions required dichotomous responses, while others used a subjective 0-10 scale. Patients were asked whether they had tried to cope with the voices by any means. Following this open question, they were presented with 25 cards detailing different coping strategies6 and asked to select those they had used to cope with the voices. Participants were also asked to prioritise the chosen strategies, according to frequency of use and effectiveness in coping with the voices.
Brief COPE
The Brief COPE24 is a validated short-form of the COPE inventory,25 a widely used measurement of coping in health- related research. The Brief COPE consists of 14 scales of 2 items each. Both cognitive and behavioural strategies of coping are included. At the end of the Brief COPE, participants were asked to indicate the 3 most useful and 3 least useful strategies for coping with day-to-day stress.
Beliefs About Voices Questionnaire – Revised
The Beliefs About Voices Questionnaire – Revised (BAVQ- R)26, developed from the original BAVQ,17 consists of 35 items and measures perceived characteristics of the voices as well as cognitive reactions to them. The 26 items of the BAVQ-R included in this study cover the following scales: malevolence, benevolence, omnipotence, emotional resistance, and emotional engagement. The BAVQ-R scales of behavioural resistance and behavioural engagement were excluded, as behavioural reactions to voices were thoroughly measured in the semi-structured interview.
Positive and Negative Syndrome Scale
The Positive and Negative Syndrome Scale (PANSS)27 has 30 items and consists of the following scales: positive, negative, and general symptomatology. It was rated by the patient’s treating psychiatrist.
Three-subtest Short Form of the Wechsler Adult Intelligence Scale – III
Three-subtest short form of the Wechsler Adult Intelligence Scale – III (WAIS-III)28 is a reduced version from the 4- subtest short form devised by Blyler et al.29 It includes Arithmetic, Digit symbol, and Information subtests and is administered within 15 minutes. Chan et al30 reported that the 3-subtest short form is almost as effective as the 4- subtest short form for estimating the general intelligence of patients with psychotic disorders.
Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS 13.0, SPSS Inc., Chicago [IL], United States). Six of the participants were male. The average age and years of education were 20.6 (standard deviation [SD] = 4.3) and 12.3 (SD = 2.5) years, respectively. About 59% of the participants were students, whereas 32% were unemployed.
Results
Except for 1 participant who was diagnosed to have bipolar affective disorder, all participants were given psychiatric diagnoses of psychosis or schizophrenia spectrum disorders. All participants were on antipsychotic medications. The PANSS score on hallucinatory experience (PANSS P3) ranged from 1 to 6, with a mean of 3.9 (SD = 1.4). Mean scores of PANSS were as follows: positive (13.4; SD = 5.5); negative (10.6; SD = 4.7); and general (22.1; SD = 7.0).
Experience of Auditory Hallucinations
Participants had experienced AHs for an average of 28 (SD = 21) months. The number of active AHs ranged from 1 to 16 (mean = 3; SD = 4). About 27% of the patients reported hearing the voices a few times per hour, 18% reported hourly occurrence of the voices, 41% reported daily occurrence, and 14% reported weekly occurrence. More than 63% of the participants reported that each occurrence of the voices lasted 10 minutes or less, 27% reported the duration to be an hour or less, and 9% reported that they lasted the whole day. There was a trend for a positive correlation between the PANSS P3 score rated by the treating psychiatrists and the frequency of voices reported by the patients (r = 0.43, p = 0.06).
Subjective pleasantness of the voices ranged from 1 to 5 (on a 0-10 scale), with an average of 3.5 (SD = 1.3). Fifteen participants reported more than one co-occurring voice, among whom two-thirds reported conversations between the voices. These participants also reported a longer duration per occurrence than those who reported no conversation between the voices (t = 2.32, p = 0.04). In 36% of the participants, the voices occurred with other (often visual) hallucinations. A majority of the participants (82%) considered the content of the voices personally relevant. About 18% reported that they knew the person who was speaking.
Beliefs about Voices
The means of the major BAVQ-R scales were as follows: malevolence (5.6; SD = 4.7); benevolence (4.8; SD = 4.1); omnipotence (8.3; SD = 3.1); emotional engagement (2.8; SD = 3.5); and emotional resistance (5.4; SD = 2.8). Malevolence was correlated with omnipotence (r = 0.46, p = 0.03), emotional resistance (r = 0.64, p = 0.001), and frequency of AHs (r = –0.51, p = 0.02). Benevolence was correlated with emotional engagement (r = 0.81, p < 0.001) and positivity of content of AHs (r = 0.46, p = 0.04). Omnipotence was correlated with emotional resistance (r = 0.58, p = 0.01) and volume of AHs (r = 0.42, p = 0.05).
Coping Strategies for Auditory Hallucinations
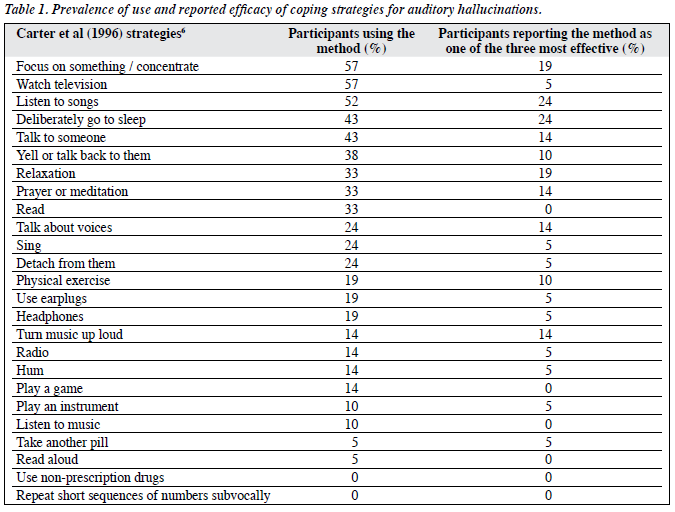
When asked in an open question, 77% of the participants spontaneously endorsed some form of coping strategy when exposed to AHs. On a 0-10 scale, the average level of subjective success in coping was 4.8 (SD = 2.4), ranged from 0 to 9. Being probed with 25 stimulus cards describing commonly used coping strategies, participants identified an average of 6.1 (SD = 2.5; range, 3-11) coping strategies that they had adopted in reaction to the voices. Eight participants named coping strategies other than the 25 on the list (e.g. shopping, using the computer, drawing, eating, crying, biting self, ignoring the voices). Nineteen participants rated at least one of the strategies that they were using as very effective in reducing AHs, whereas 1 reported that none of the adopted strategies were effective. Table 1 shows the popularity of each strategy and its perceived effectiveness.
As shown in Table 1, the proportion of participants trying each specified method ranged from 0 to 57%, and the proportion reporting each method as effective ranged from 0 to 24%. The most popular coping strategies were focus on something / concentrate, watch television, listen to songs, deliberately go to sleep, and talk to someone. Listen to songs and deliberately go to sleep were also rated by most participants as one of the 3 most effective methods. Focus on something / concentrate and relaxation were rated by 19% as effective. On the other hand, while a substantial proportion of participants used television (57%) and talk to someone (43%) for coping, only 5% and 14% respectively found them effective in reducing the voices. More still, 18% of the participants rated television as one of the 3 least effective coping strategies.
Relationship between Coping Strategies and Characteristics of Voices and Beliefs about Voices
Participants with spontaneous coping with AHs reported higher volumes than those without spontaneous coping (t = 2.32, p = 0.03). The total numbers of strategies adopted to cope with AHs was positively correlated with the PANSS general symptomatology score (r = 0.46, p = 0.04), and negatively correlated with the duration of AHs (r = –0.53, p = 0.02). Subjective success of coping with AHs was negatively correlated with the volume of AHs (r = –0.52, p = 0.03) and clarity of AHs (r = –0.60, p = 0.01), and was less evident among participants reporting co-occurrence of hallucinations in other sensory domains (t = –2.49, p = 0.03). There was no statistically significant relationship between subjective success of coping with AHs and the total number of adopted strategies (p > 0.05), nor was there a correlation between BAVQ-R measures and the number of coping strategies or subjective success (p > 0.05).
Coping with General Stress
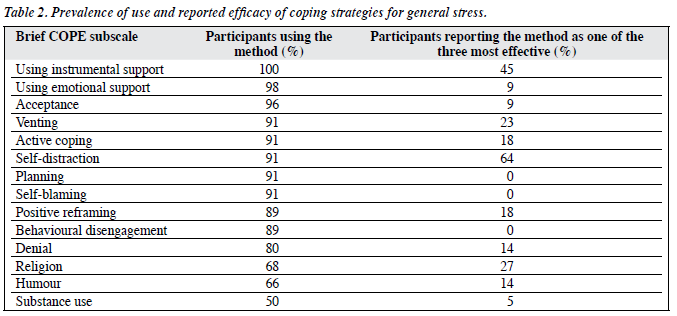
Among the 28 coping strategies in the Brief COPE scale, participants reported an average of 23.8 (SD = 3.2) strategies in reaction to general stress, ranged from 16 to 28. As shown in Table 2, the proportion of participants trying each specified method ranged from 50 to 100%, while the proportion reporting each method as effective ranged from 0 to 64%. The 5 most popular coping strategies entailed: using instrumental support, using emotional support, acceptance, venting, and active coping. The strategies most often rated as effective were self-distraction and using instrumental support. Planning, self-blame, and behavioural disengagement were endorsed by a substantial proportion of the participants, but were rated by none of them as effective methods of coping.
The PANSS positive score was correlated with acceptance (r = 0.54, p = 0.01), substance use (r = –0.56, p = 0.01), and venting (r = –0.44, p = 0.05), whereas the PANSS negative score was correlated with behavioural disengagement (r = –0.47, p = 0.03). Participants with a higher level of education reported more active coping (r = 0.67, p = 0.001), and those with higher IQ estimates reported less venting (r = –0.46, p = 0.03).
Relationship between Coping with Voices and Coping with General Stressors
Participants who coped with AHs spontaneously reported more coping strategies in the face of general stress (t = 2.70, p = 0.01). They also reported more use of the following Brief COPE strategies: active coping (t = 2.83, p = 0.01), using instrumental support (t = 2.61, p = 0.02), and positive reframing (t = 2.90, p = 0.01). On the other hand, they relied less on religion (t = –2.59, p = 0.02) in reaction to stress. There was no significant correlation between the number of coping strategies used for AHs and for general stress (p > 0.05), but the number of strategies adopted to cope with AHs was positively associated with the Brief COPE subscales use of emotional support (r = 0.47, p = 0.03) and humour (r = 0.47, p = 0.03). Subjective success of coping with AHs was negatively correlated with the Brief COPE subscale for acceptance (r = –0.54, p = 0.03).
Discussion
This is the first study, using a semi-structured interview, to look into the subjective experience of persistent AHs in patients with first-episode psychosis, and how these patients cope with this particular drug-resistant symptom. This study also compared how patients coped with AHs in contrast to general stress. Despite active antipsychotic treatment, this group of patients still experienced frequent and unpleasant AHs, the extent of which might not be fully reflected on a clinical rating scale. Characteristics of the hallucinatory experience varied between individuals with psychosis. A majority of patients found that content of the voices had personal meaning.
Beliefs about voices were related to certain of their physical characteristics, namely frequency, duration, and volume. Although the mean scores for benevolence and malevolence were higher in this study than in previous studies,17,18 the relationships between benevolence and (emotional) engagement and between malevolence and (emotional) resistance were the same as previously reported.17,18 There was no direct relationship between beliefs about voices as measured by the BAVQ-R and the use and efficacy of coping strategies. It is not clear to what extent such lack of relationship was accounted for by the small sample size.
When asked openly, 77% of the participants spontaneously endorsed some form of coping with AHs, but they all reported having used at least 1 coping strategy when prompted with stimulus cards. This indicates the importance of using multiple methods of measurement when enquiring about coping.7,8 An average of 6 coping strategies were identified, and the choices were highly diverse. This is in keeping with previous findings in patients with non–first-episode psychosis.5 Consistent with Boschi et al’s findings,14 patients with more severe symptomatology tended to endorse a greater number of coping strategies, suggesting that employment of more strategies is a response to symptoms.
Although most patients identified at least 1 effective strategy, they generally considered their coping with AHs only moderately successful, which is consistent with previous findings.14,15 Also, patients with a longer history of AHs had fewer coping strategies but not higher success rates at coping, which is consistent with Carter et al’s6 suggestion that individuals with AHs did not learn from their attempts at coping. However, the present finding is contradictory to previous studies, whereby effectiveness improves with the use of more coping strategies.10-11,13
In this study, the most frequently used strategies for coping with AHs were also reported by patients with non– first-episode psychosis described by Farhall et al.5 Two of the most frequently used strategies were rated as effective by the highest proportion of participants, but one of the most frequently used strategies was only found to be effective by a small minority. This finding offers partial support for Carter et al’s6 argument that the most frequently reported strategies are not those reported as successful.
Current results do not support Boschi et al’s14 findings that the most frequently endorsed strategies are cognitive in nature, while the most helpful are behavioural. In fact, a behavioural strategy (e.g. listening to songs) can be cognitive in function (e.g. trying to be positive or shifting attention), so it may not be meaningful to differentiate coping strategies by such dichotomous taxonomy.4
In reaction to general stress, each listed strategy was adopted by at least half of the participants, suggesting a wide coping repertoire in this group of patients. The frequency and perceived effectiveness of stress coping strategies was higher than that for AH coping strategies. Such a difference in response could not be due to methodology, as coping with both AHs and stress was enquired into using a prompt list. Rather, it is possible that patients generally find it easier to cope with general stress than with AHs, although this speculation warrants empirical testing.
The most frequently used stress coping strategies were also commonly endorsed by patients with early psychosis in an earlier study.22 Contrary to studies on patients with a longer history of schizophrenia,31 patients in the current study used both emotion-focused and problem-focused coping, suggesting a higher level of functioning and success at coping.32-34 However, patients with more severe negative symptoms were related to less use of problem- focused coping, which was also consistent with previous studies.32-34 Also, the fact that patients with more positive symptoms were more ready to use acceptance is consistent with McGorry’s35 suggestion that the trauma associated with psychosis may result in people believing that most situations exceed their coping skills.
Patients who spontaneously coped with AHs also adopted more coping strategies and used more positive coping in reaction to general stress. Patients who were less ready to accept the reality as it was also reported a higher level of success in coping with AHs. It is likely that individuals who cope more actively with day-to-day stress were also active copers in face of AHs, in which case AH was only another form of general stressor. As discussed earlier, coping with AHs was also related to the characteristics of the voices as well as the severity of symptomatology. Future research with a larger sample might delineate the relative importance of these factors in predicting coping with AHs.
Results from the present study imply that psycho- logical interventions for drug-resistant AHs should have a dual focus: symptom coping and general stress management. Nevertheless, among the various forms of psychological interventions for psychosis currently available,36 only Tarrier et al’s37 broader cognitive behavioural therapy for psychosis package combined symptom coping with problem-solving and relapse prevention. It was also the only intervention that reported specific results for hallucinations.38 To what extent these were attributable to the coping enhancement component as opposed to the problem-solving or relapse- prevention components is a question for future research.
A major limitation of the present study was the small sample size, which might have limited the generalisability of our findings. Due to the more common use of atypical antipsychotics in patients with first-episode psychosis, recruiting patients with persistent AHs was slower and more difficult than in other studies with chronic patients. The small sample size did not permit stratified analysis that may allude to possible factors associated with different domains of coping. Besides, efficacy of coping with AHs was only rated for strategies adopted by the participants. Therefore, there were no data on how often they applied each strategy and how effective they felt each one was. Direct comparison between coping for hallucinations and stress coping was also limited by the use of different tools for coping measurement. Therefore, this study can be regarded as exploratory in this new area of coping with early psychosis and invites further research using comparable coping measures, a control group, and a larger sample size.
Patients with psychotic disorders are not passive victims of the disease. Instead, they are involved in a personal relationship with their psychotic symptoms and interact with them in individually different ways. In reaction to unpleasant hallucinations, patients spontaneously adopt a number of strategies to cope, reaching a modest level of subjective success. This study shows that the more frequently used strategies may not be the most effective, but patients with first-episode psychosis cope better than chronic patients. Coping with drug-resistant AHs is related to symptomatology, perceived characteristics of the voices, as well as general coping styles. Their clinical implications and future research directions have been discussed.
Declaration
This project was not funded by any external sources and did not involve any conflicts of interest.
References
- Sartorius N, Jablensky A, Korten A, Ernberg G, Anker M, Cooper JE, et al. Early manifestations and first-contact incidence of schizophrenia in different cultures. A preliminary report on the initial evaluation phase of the WHO Collaborative Study on determinants of outcome of severe mental disorders. Psychol Med 1986;16:909-28.
- Pantelis C, Barnes TR. Drug strategies and treatment-resistant schizophrenia. Aust N Z J Psychiatry 1996;30:20-37.
- Birchwood M, Meaden A, Trower P, Gilbert P, Plaistow J. The power and omnipotence of voices: subordination and entrapment by voices and significant others. Psychol Med 2000;30:337-44.
- Garcelán SP, Rodríguez AG. Coping strategies in psychotics: conceptualization and research results. Psychology in Spain 2002;6:26- 40.
- Farhall J, Greenwood KM, Jackson HJ. Coping with hallucinated voices in schizophrenia: a review of self-initiated strategies and therapeutic interventions. Clin Psychol Rev 2007;27:476-93.
- Carter DM, Mackinnon A, Copolov DL. Patients’ strategies for coping with auditory hallucinations. J Nerv Ment Dis 1996;184:159-64.
- Farhall J, Gehrke MJ. Coping with hallucinations: exploring stress and coping framework. Br J Clin Psychol 1997;36:259-61.
- Farhall J, Voudouris NJ. Persisting auditory hallucinations: prospects for non-medication interventions in a hospital population. Behav Change 1996;13:112-23.
- Green MF, Kinsbourne M. Auditory hallucinations in schizophrenia: does humming help? Biol Psychiatry 1989;25:633-5.
- Nayani TH, David AS. The auditory hallucination: a phenomenological survey. Psychol Med 1996;26:177-89.
- Romme MA, Escher AD. Hearing voices. Schizophr Bull 1989;15:209-16.
- Romme MA, Honig A, Noorthoorn EO, Escher AD. Coping with hearing voices: an emancipatory approach. Br J Psychiatry 1992;161:99-103.
- Tarrier N. An investigation of residual psychotic symptoms in discharged schizophrenic patients. Br J Clin Psychol 1987;26:141-3.
- Boschi S, Adams RE, Bromet EJ, Lavelle JE, Everett E, Galambos N. Coping with psychotic symptoms in the early phases of schizophrenia. Am J Orthopsychiatry 2000;70:242-52.
- Falloon IR, Talbot RE. Persistent auditory hallucinations: coping mechanisms and implications for management. Psychol Med 1981;11:329-39.
- O’Sullivan K. Dimensions of coping with auditory hallucinations. Journal of Mental Health 1994;3:351-61.
- Chadwick P, Birchwood M. The omnipotence of voices. II. The Beliefs About Voices Questionnaire (BAVQ). Br J Psychiatry 1995;166:773-6.
- Sayer J, Ritter S, Gournay K. Beliefs about voices and their effects on coping strategies. J Adv Nurs 2000:31:1199-205.
- Middelboe T, Mortensen EL. Coping strategies among the long-term mentally ill; categorization and clinical determinants. Acta Psychiatr Scand 1997;96:188-94.
- Corrigan PW, Toomey R. Interpersonal problem solving and information processing in schizophrenia. Schizophr Bull 1995;21:395- 403.
- Penn DL, van der Does AJ, Spaulding WD, Garbin CP, Linszen D, Dingemans P. Information processing and social cognitive problem solving in schizophrenia. Assessment of interrelationships and changes over time. J Nerv Ment Dis 1993;181:13-20.
- Macdonald EM, Pica S, Mcdonald S, Hayes RL, Baglioni AJ Jr. Stress and coping in early psychosis. Role of symptoms, self-efficacy, and social support in coping with stress. Br J Psychiatry Suppl 1998;172:122-7.
- Chen EY. Developing an early intervention service in Hong Kong. In: Ehmann T, MacEwan GW, Honer WG, editors. Best care in early psychosis intervention: global perspectives. London: Taylor & Francis; 2004: 125-30.
- Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med 1997;4:92-100.
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 1989;56:267-83.
- Chadwick P, Lees S, Birchwood M. The revised Beliefs About Voices Questionnaire (BAVQ-R). Br J Psychiatry 2000;177:229-32.
- Kay SR. Positive and negative syndromes in schizophrenia: assessment and research. In: Kay SR, editor. Clinical and experimental psychiatry monograph, No. 5. Philadelphia, PA: Brunner/Mazel; 1991.
- Wechsler D. WAIS-III: Wechsler Adult Intelligence Scale. Administration and scoring manual. 3rd ed. San Antonio: Psychological Corporation/Harcourt Brace; 1997.
- Blyler CR, Gold JM, Iannone VN, Buchanan RW. Short form of the WAIS-III for use with patients with schizophrenia. Schizophr Res 2000;46:209-15.
- Chan EL, Chen EY, Chan RC. Three-subtest short form of the Wechsler Adult Intelligence Scale – III for patients with psychotic disorders: a preliminary report. Hong Kong J Psychiatry 2005;15:39-42.
- van den Bosch RJ, van Asma MJ, Rombouts R, Louwerens JW. Coping style and cognitive dysfunction in schizophrenic patients. Br J Psychiatry Suppl 1992;(18):123-8.
- Cohen CI, Berk LA. Personal coping styles of schizophrenic outpatients. Hosp Community Psychiatry 1985;36:407-10.
- Wiedl KH. Assessment of coping with schizophrenia. Stressors, appraisals, and coping behaviour. Br J Psychiatry Suppl 1992;(18):114- 22.
- Wiedl KH, Schöttner B. Coping with symptoms related to schizophrenia. Schizophr Bull 1991;17:525-38.
- McGorry PD. The concept of recovery and secondary prevention in psychotic disorders. Aust N Z J Psychiatry 1992;26:3-17.
- Wykes T. Psychological treatment for voices in psychosis. Cognit Neuropsychiatry 2004;9:25-41.
- Tarrier N, Haddock G, Barrowclough C. Training and dissemination: research to practice in innovative psychosocial treatments for schizophrenia. In: Wykes T, Tarrier N, Lewis S, editors. Outcome and innovation in psychological treatment of schizophrenia. Chichester: John Wiley & Sons; 1998: 214-36.
- Tarrier N, Kinney C, McCarthy E, Wittkowski A, Yusupoff L, Morris J, et al. Are some types of psychotic symptoms more responsive to cognitive-behaviour therapy? Behavioural and Cognitive Psychotherapy 2001;29:45-55.