Hong Kong J Psychiatry 2008;18:131-5
ORIGINAL ARTICLE
Dr R Chandrasekaran, MD, Department of Medicine, Asian Institute of Medicine, Science and Technology 08100, Kedah Darul Aman, Malaysia.
Dr J Gnanaselane, MA, MSW, Department of Psychiatry, Jipmer, Pondicherry 605006, India.
Address for correspondence: Dr R Chandrasekaran, School of Medicine, Asian Institute of Medicine, Science and Technology, Jalan Bedong, Semeling, 08100 Kedah Darul Aman, Malaysia.
Tel: 0060164138739; Fax: 006044298083; E-mail: drrch54@gmail.com
Submitted: 2 May 2008; Accepted: 14 July 2008
Abstract
Objective: Little is known about the risk factors that differentiate individuals who make subsequent suicide attempts after surviving their first attempt. This study investigated the predictors of repeat suicidal attempts in first-ever attempters.
Participants and Methods: Face-to-face interviews were conducted with 348 subjects who were hospitalised following their first-ever suicide attempt. Information on socio-demographic, clinical, and psychosocial variables related to the suicide attempt was collected. In 293 patients, a follow-up interview was completed at the end of 2 years. Factors associated with repeat suicidal attempts were evaluated. Results: The repetition rate at the end of 2 years was 23%. Repeat suicide attempters showed higher levels of baseline depression, hopelessness, and suicidal intent. They also had elevated stress scores during the 12 months prior to the attempt and poorer adaptive functioning. The presence of major depression and social maladaptation had a significant predictive value for repeat attempts in first-ever attempters. Conclusions: Treatment of depression in first-ever attempters should be optimised to minimise the risk of future attempts.
Key words: Depressive disorder; Recurrence; Risk factors; Suicide, attempted; Follow-up studies
摘要
目的:對於能分辨出自殺未遂者再嘗試自殺的危險因素所知甚少。本研究探討自殺未遂者反復自殺的預測因子。
參與者與方法:與348位首次自殺未遂而入院的病人進行面試,收集與他們自殺有關的資料,如社會人口學、臨床、心理社會變項。兩年後,成功與293位病人再進行隨訪面試,研究出他們反復自殺的預測因子。
結果:病人兩年後反復自殺率為23%。反復自殺者在最初抑鬱、絕望、自殺意圖方面的程度相對高。病人在嘗試自殺的12個月前的壓力分數上升,適應能力亦較差。嚴重抑鬱和社會不良適應均為自殺未遂者反復自殺的顯著預測因子
結論:應盡量為首次自殺未遂者治療抑鬱,以減低病人反復自殺的危險。
關鍵詞:抑鬱、反復、危險因素、企圖自殺、隨訪研究
Introduction
Suicide attempts may become a recurrent pattern of behaviour. Patients who repeat attempts experience a heavy burden of distress, continue to put themselves at risk, and may eventually kill themselves. About 20 to 40% of the suicide attempters repeat suicidal attempts; most of them within the first 3 years.1-4 Follow-up evaluation extending back 10 years also supports this finding.5 Factors relating to repeat suicidal attempts have been extensively studied. Young age has been implicated, whereas the converse is true for ‘successful’ suicide.3 Unemployment in association with personality disorders was reportedly a risk factor for repeat attempts.6 Those who engaged in repeat suicidal behaviour are more likely to be suffering from mental disorders including schizophrenia,7 dysthymia,8 substance use,9 and personality disorders.10 Other risk factors include: prior attempt, a family history of suicide,7 being divorced or separated,11 and having a history of psychiatric treatment,6,8,9 interpersonal conflicts,12 and poor social networking.4 To overcome possible correlation among the various risk factors, logistic regression models have been applied.13 In the majority of these studies, the sample comprised a mix of first attempters and repeaters. Recent studies showed that multiple attempters are likely to have more depressive symptoms, greater suicidal risk, and experience more stress than one-time attempters.14 There is inadequate information about risk factors that differentiate individuals who make subsequent suicidal attempts after surviving their first attempt from those who do not. The present investigation was a 2- year follow-up evaluation using face-to-face interviews with survivors following their first-ever suicide attempt, with a view to identifying the predictors of repeat attempts.
Methods
This was a prospective observational study. Subjects were patients presenting to the emergency department of the Jawaharlal Institute of Post Graduate Medical Education and Research, a tertiary care hospital in India, during the period January to December 2002. Ours was a public hospital offering both free and paid services to patients depending on their income. The resident doctors of different clinical departments were informed about the scope of the study to ensure prompt referral. Information available in the admission register of the emergency medical services was scrutinised to avoid omission of cases. The study defined suicidal attempt as a condition that received a diagnostic code under “intentional self harm” (x60-x84), Chapter XX in the International Classification of Diseases.15 Individuals younger than 18 years were excluded, as were those who obtained a score of less than 25 on Mini- Mental State Examination.16
Assessment at First Interview
Patients were assessed in their respective wards after the medical condition became stable. The research worker made first contact with the patient in the ward. Each patient was informed about the nature and scope of the investigation, and informed consent was obtained with an option to withdraw from the study at any time. The assessment was completed over 2 sessions; each session took about 30 to 45 minutes. All but 3 patients (interviewed at home) completed the interview in the hospital. A semi-structured schedule was used to collect information on socio-demographic and psychosocial variables and details of the suicidal attempt. In addition, the following rating instruments were used:
- Mini International Neuropsychiatric Interview (MINI) Plus,17 a structured diagnostic interview jointly developed by European and American psychiatrists for the Diagnostic and Statistical Manual of Mental Disorders–IV (DSM-IV) and International Classification of Diseases 10 (ICD-10) categories. It features a number of algorithms to handle hierarchical rule-outs in the event the patient had one disorder at a time;
- ICD-10 International Personality Disorder Examination,18 a self-reported instrument available in a separate module based on ICD-10. It has a screening questionnaire consisting of 59 true / false items. If 3 or 4 items are circled, the patients have failed the screen for that disorder and have to be interviewed subsequently;
- Risk Rescue Rating Scale,19 which is used for assessing the lethality of suicidal attempts. The underlying principle of the scale is the lethality of implementation, defined as the probability of inflicting irreversible damage, and may be expressed as a ratio of factors influencing risk and rescue. The scale has 5 risk factors and 5 rescue factors;
- Suicide Intent Scale,20 which is divided into 3 sections: (i) objective circumstances related to the suicidal attempt, (ii) self report, and (iii) others;
- Hopelessness Scale,21 a self-reporting instrument consisting of 20 statements of thoughts and feelings about the future. Subjects rate each item as true or false;
- Montgomery Asberg Depression Rating Scale,22 which contains 10 items and includes all the most important depressive symptoms;
- Presumptive Stressful Life Events Scale23 that included 51 items in all, which has been constructed specifically for the Indian population. Each event has a presumptive stress score standardised for the Indian population;
- Global Assessment Functioning Scale24 is an Axis V of DSM-IV, which records the clinician’s judgement regarding the highest level of adaptive functioning demonstrated by the patient during the past 1 year;
- Multidimensional Scale of Perceived Social Support,25 which is a 12-item self-rated measure of social support as perceived by the individual.
Translation and back-translation exercises were carried out for the self-rated scales with the aid of bilingual experts. The consultant psychiatrist administered the MINI Plus and International Personality Disorder Examination. One of the authors, a mental health professional, was specially trained to administer the other scales. The inter-rater reliability was determined for observer-rated scales, namely: the Risk Rescue Rating Scale, the Global Assessment Functioning Scale, and the Montgomery Asberg Depression Rating Scale and were found to be 0.69, 0.61, and 0.71, respectively. Formal approval for the study was granted by the Institute’s Research Council and was later cleared by the relevant Ethics Committee.
The Follow-up Interview
At follow-up at the end of 2 years, the investigator conducted a face-to-face interview of the patients in their homes. The research worker dispatched letters to the subjects informing them of the proposed visit, to ensure the availability of the subject and visited their home on the day the interview was scheduled. For subjects missing appointments, the research worker left a postage-paid addressed envelope with a neighbour, to be handed to that patient for a future appointment. The follow-up evaluation was similar to that of the first, and sought specific information on repeated attempts. Thus, the present study used only self-reported information on suicidal attempts that occurred at any point of time between the first and second evaluation.
Results
Of 348 individuals who met the eligibility criteria, the study sample included a total of 341 persons who agreed to participate; 7 were excluded as they refused. This sample amounted to approximately 2.5% of the total number of emergency admissions in that calendar year. There were 153 (45%) men and 188 (55%) women. The mean age of the patients was 26 (standard deviation [SD], 9) years. The mean (SD) ages of the men and women were 27 (18) years and 25 (10) years, respectively. In all, 189 (55%) of the subjects were in the 18-to-24 year age-group, and 206 (60%) reported that they were employed at the time of the attempt. In all, 135 (40%) were unskilled labourers, 184 (54%) were married, 289 (85%) came from rural areas, and 309 (91%) attempted suicide by consuming either insecticide or poisons of vegetable origin. The 2-year follow-up evaluation was completed for 293 patients. Regarding the remaining 48 patients, 8 (3 males and 5 females) had committed suicide, 5 had died of various medical problems, and the rest could not be traced (as they had moved residence).
Clinical Correlates of Repeat Suicidal Attempts
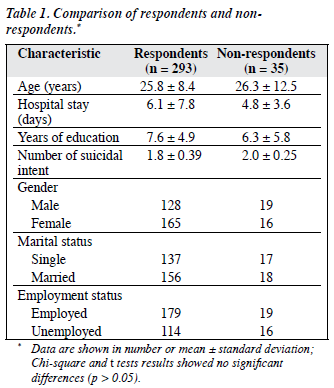
The respondents and non-respondents did not differ significantly in terms of age distribution, gender, and duration of hospital stay, education, employment, and level of suicidal intent at first assessment (Table 1). The repetition rates of suicidal attempts in the first and second years were 14% and 9%, respectively; at the end of 2 years, 23% of the sample had reattempted. No individual had attempted suicide more than once during the observation period. Only 14 subjects received psychiatric treatment for a brief period following the second attempt.
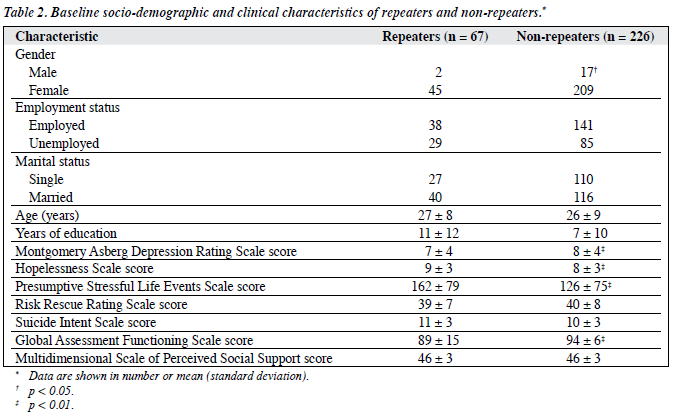
Age, marital status, employment, and educational status did not distinguish the repeaters from non-repeaters (p = not significant). Repeaters reported a history of psychiatric treatment more often than non-repeaters. The mean stress score calculated for the 6 months prior to the attempt was significantly higher in repeaters than in non-repeaters (t = 2.32, p < 0.01). Repeaters were observed to score higher on the hopelessness scale (t = 2.46, p <0.01), and displayed impaired social adaptation. Although suicidal intent following the first attempt was higher among repeaters, the lethality of implementation, as measured by risk rescue scores, did not discriminate repeaters from non-repeaters. The social support received by both groups was not significantly different (Table 2).
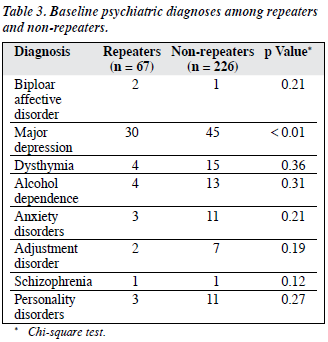
Depression and Repeat Suicidal Attempts
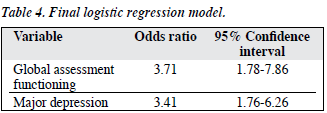
Psychiatric diagnostic categories identified in the sample are shown in Table 3. Major depressive disorder was found to be significantly more common among repeaters. A logistic regression model was developed to assist in predicting a particular outcome. The outcome variable of interest in this study was the presence or absence of a reattempt. Predictor variables that emerged significantly in the bivariate analysis were selected. The explanatory variables included in the model were both categorical and continuous. The forward stepwise option (Wald) was used. Global assessment functioning and a diagnosis of major depression emerged as significant predictors for repeat attempts (Table 4).
Discussion
This study differs from most others in that the patients did not have any history of prior suicidal attempt, thereby producing a homogenous sample of first-ever suicide attempters. The design of the study was prospective, and involved a large sample size. Potential risk factors were examined both at the initial and follow-up evaluation. Of 341 patients who were initially interviewed, 293 underwent follow-up interviews. However, the study suffers from several limitations. Being a hospital-based study, the results could not be generalised to the whole community. Adolescents were excluded. The majority of patients were from rural areas. The pattern of suicidal attempts may have differed from that in urban settings. Although the subjects were asked to recall the period when the repeat act occurred, there was no certainty about the accuracy of retrospective recollection. With further extension of the follow-up period, it is probable that more single attempters would have made subsequent attempts. The long-term physical effect of pesticides on individuals who survived the attempt could have affected their mental health adversely, which was an aspect that was not evaluated during the follow-up.
At the end of 2 years, 23% of the sample had reattempted. As the focus of the study was on survivors, the subjects who successfully committed suicide at their first attempt were obviously omitted from the analysis. Two studies26,27 have recorded the prevalence of repetition in first-ever attempters, and reported that 8 to 10% of patients repeated the act during the first 12 months of follow-up. Several socio-demographic variables such as age, education, employment status, marital status, living arrangements, urban-rural dichotomy, and socio-economic class were not associated with the repeat attempts. Similarly a family history of suicide and attempted suicide, lethality of implementation, duration of hospital stay, and perceived social support failed to differentiate repeaters from non-repeaters. Our study confirmed the trend reported by others, wherein among repeaters women significantly outnumbered men.2
Past psychiatric treatment and repeat suicidal behaviour show a significant association; though the subjects who reported having sought psychiatric treatment in the past were few, the association was highly significant. Other studies have also reported this finding.6,15 Thus, a history of psychiatric treatment can be considered evidence for mental morbidity, and such individuals are probably at a higher risk for repeat suicidal behaviour. Mood disorders occupy a prominent place in suicide attempters, among which depressive episodes are frequently diagnosed.3 In other studies, there is also an over-representation of alcohol abuse.2,28 A lifetime history of schizophrenia and major depression are also strong predictors for repeat attempts.13 In our study, major depressive episode emerged as a significant clinical condition in repeaters. Levels of depression and hopelessness were also significantly higher in repeaters than in non-repeaters.4,29 Depression and hopelessness can influence each other and together act as mediators between various clinical conditions and suicidal behaviour.29 The role of personality disorders in repeat suicidal attempts have been examined.30,31 In this investigation, the prevalence of personality disorders among the repeaters was low. Some personality traits, such as impulsivity, has been associated with suicidal attempts.32 In future studies of similar scope, it is therefore worth investigating the role of personality traits like impulsivity.
An inverse relationship between the severity of suicidal intent and repeat attempts has been documented in a few investigations.28,33 Our study showed that repeaters had higher intent scores than non-repeaters. High intent is known to correlate with the presence of mental morbidity.34,35 If the mental disorder is not adequately managed, the individual will be at a higher risk of future attempts. Mean stress scores calculated for the 6 months prior to the attempt were also elevated in repeaters. An obvious drawback in the interpretation of this finding is that the summated scores do not capture the impact of individual life events for any individual.
Social maladaptation was one of the risk factors for reattempts. Tejedor et al36 concluded that psychiatric treatment and psychosocial assistance for optimising the patient’s integration into his / her own environment may significantly reduce suicidal risk. In our study, social adaptation was more impaired in repeaters at the index evaluation. The regression model identified 2 variables as significant predictors of repeat attempts, namely presence of major depression and impaired social adaptation. Thus, the factors that play a role in a para-suicidal event may be different from those that have a predictive value for future suicidal behaviour.13 In another comparable study,27 a lifetime history of sexual abuse (both sexes), alcohol abuse, and self-reported psychiatric problems as the main concern (females only), were found to have significant predictive value. Although many independent variables were associated with repeat attempts when examined under bivariate analysis, only 2 emerged from the final logistic regression model. Proper management of co-existing mental disorder and adequate provision of psychosocial assistance during periods of crisis are likely to minimise the risk of future attempts in susceptible individuals.
Acknowledgement
This study is a major research project funded by the University Grants Commission, New Delhi, India.
References
- Rygnestad T. A prospective 5-year follow-up study of self-poisoned patients. Acta Psychiatr Scand 1988;77:328-31.
- Brauns ML, Berzewski H. Follow-up study of patients with attempted suicide. Int J Soc Psychiatry 1988;34:285-91.
- Johnsson Fridell E, Ojehagen A, Träskman-Bendz L. A 5-year follow- up study of suicide attempts. Acta Psychiatr Scand 1996;93:151-7.
- Kerkhof A, Arensman E, Bille-Brahe U, et al. Repetition of attempted suicide results from the WHO-EU Multi-Centre study on Para suicide: Repetition-Prediction Part. Proceedings of the 7th European Symposium on Suicide and Suicidal Behaviour; 1998 Sep 9-12; Gent, Belgium; 1998.
- Hall DJ, O Brien F, Stark C, Pelosi A, Smith H. Thirteen-year follow-up of deliberate self-harm, using linked data. Br J Psychiatry 1998;172:239-42.
- Dirks BL. Repetition of parasuicide—ICD-10 personality disorders and adversity. Acta Psychiatr Scand 1998;98:208-13.
- van Aalst JA, Shotts SD, Vitsky JL, Bass SM, Miller RS, Meador KG, et al. Long-term follow-up of unsuccessful violent suicide attempts: risk factors for subsequent attempts. J Trauma 1992;33:457-64.
- Ojehagen A, Danielsson M, Träskman-Bendz L. Deliberate self- poisoning: treatment follow-up of repeaters and nonrepeaters. Acta Psychiatr Scand 1992;85:370-5.
- Morgan HG, Barton J, Pottle S, Pocock H, Burns-Cox CJ. Deliberate self- harm: a follow-up study of 279 patients. Br J Psychiatry 1976;128:361-8.
- Buglass D, Horton J. The repetition of parasuicide: a comparison of three cohorts. Br J Psychiatry 1974;125:168-74.
- Krietman N, Casey P. Repetition of parasuicide: an epidemiological and clinical study. Br J Psychiatry 1988;153:792-800. Erratum in: Br J Psychiatry 1998;154:733.
- Diekstra RF. Suicide and the attempted suicide: an international perspective. Acta Psychiatr Scand Suppl 1989;354:1-24.
- Colman I, Newman SC, Schopflocher D, Bland RC, Dyck RJ. A multivariate study of predictors of repeat parasuicide. Acta Psychiatr Scand 2004;109:306-12.
- Michaelis BH, Goldberg JF, Singer TM, Garno JL, Ernst CL, Davis JP. Characteristics of first suicide attempts in single versus multiple suicide attempters with bipolar disorder. Compr Psychiatry 2003;44:15-20.
- The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
- Folstein MF, Flostein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59(Suppl 20):S22-33.
- Loranger AW, Janca A, Sartorius N. Assessment and diagnosis of personality disorders. The ICD-10 International Personality Disorder Examination. New York: Cambridge University Press; 1977.
- Weisman AD, Worden JW. Risk-rescue rating in suicide assessment. Arch Gen Psychiatry 1972;26:553-60.
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale of Suicide Ideation. J Consult Clin Psychol 1979;47:343-52.
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol 1974;42:861-5.
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979;134:382-9.
- Singh G, Kaur D, Kaur H. Handbook for presumptive stressful life event scale. Agra, India: National Psychological Corporation; 1983.
- Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; 1994.
- Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess 1990;55:610-7.
- Wilkinson G, Smeeton N. The repetition of parasuicide in Edinburgh 1980-1981. Soc Psychiatry 1987;22:14-9.
- Hjelmeland H. Repetition of parasuicide: a predictive study. Suicide Life Threat Behav 1996;26:395-404.
- Hirschfeld RM, Davidson L. Risk factors for suicide. Review of Psychiatry 1988;7:307-33.
- Hawton K, Fagg J, Platt S, Hawkins M. Factors associated with suicide after parasuicide in young people. BMJ 1993;306:1641-4.
- Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. Discriminating borderline personality disorder from other Axis II disorders. Am J Psychiatry 1990:147;161-7.
- Garvey MJ, Spoden F. Suicide attempts in antisocial personality disorder. Compr Psychiatry 1980;21:146-9,
- Simon OR, Swann AC, Powell KE, Potter LB, Kresnow MJ, O’Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav 2001;32(1 Suppl):S49-59.
- Cullberg J, Wasserman D, Stefansson CG. Who commits suicide after a suicide attempt? Acta Psychiatr Scand 1988;77:598-603.
- Pierce DW. Suicidal intent in self-injury. Br J Psychiatry 1977;130:377-85.
- Kumar CT, Mohan R, Ranjith G, Chandrasekaran R. Characteristics of high intent suicide attempters admitted to a general hospital. J Affect Disord 2006;91:77-81.
- Tejedor MC, Díaz A, Castillón JJ, Pericay JM. Attempted suicide: repetition and survival—findings of a follow-up study. Acta Psychiatr Scand 1999;100:205-11.