Hong Kong J Psychiatry 2008;18:158-65
ORIGINAL ARTICLE
吉隆坡醫院的病人自殘行為與月經週期之關係
Dr Omar Ainsah, MD, MMed Psych, PhD, Discipline of Psychiatry, Universiti Teknologi MARA, Malaysia.
Dr B Norharlina, MD, MMed Psych, Department of Psychiatry, Hospital Kuala Lumpur, Malaysia.
Dr CB Osman, MD, MMed Psych, Discipline of Psychiatry, Universiti Teknologi MARA, Malaysia.
Address for correspondence: Dr CB Osman, Discipline of Psychiatry, Universiti Teknologi MARA, Malaysia.
Tel: (603) 5544 2000; Fax: (603) 9173 74841; E-mail: ocbaaaah@yahoo.com.my
Submitted: 23 December 2007; Accepted: 3 May 2008
Abstract
Objective: To examine the relationship between the menstrual cycle and deliberate self-harm.
Participants and Methods: This was a case-control study on consecutive eligible female patients (n = 86) admitted to Hospital Kuala Lumpur following an episode of deliberate self-harm (defined by Hawton, 1999) and controls admitted for acute minor medical problems during the period March to June 2005. The Mini-International Neuropsychiatric Interview and Suicide Intent Scale were administered to diagnose psychiatric disorders and to assess suicidal intensity.
Results: Patients with deliberate self-harm were associated with the age-group of 18 to 29 years (84%), being single (61%), and employed (78%). They were also significantly associated with being of Malay origin (p < 0.05), having a lower education level (p < 0.05), lacking a confiding relationship (p < 0.05), and having a depressive disorder (p < 0.05). The commonest method was self-poisoning (91%). More than half of the patients had medium suicidal intent. Deliberate self-harm was significantly associated with the follicular phase of the menstrual cycle (p < 0.05), later onset of menarche (p < 0.05), and shorter duration of menses (p < 0.05). Diagnoses of depressive disorders were not significantly different according to the phase of the menstrual cycle (p > 0.05).
Conclusion: Menstrual factors may be significantly associated with deliberate self-harm. Further investigations are recommended to explore psychosocial and physiological factors associated with deliberate self-harm in young women.
Key words: Menstrual cycle; Mental disorders; Premenstrual syndrome; Suicide, attempted
摘要
目的:探討月經週期與病人自殘行為的關係。
參與者與方法:此病例對照研究包括於2005年3月至6月入住吉隆坡醫院的病人,其中有自殘行為(根據1999年Hawton的定義)的連續86名病人(病例組),以及因急性輕微疾病的病人(對照組)。使用「迷你國際神經精神會談工具」(MINI)及「自殺意圖量表」診斷精神病及病人自殺意欲程度。
結果:有自殘行為的病人與年齡介乎18至29歲(84%)、單身(61%)、和在職(78%)有關。此外,亦與以下因素有顯著關係:馬來人(p < 0.05)、低教育水平(p < 0.05)、沒有摯友(p < 0.05)、患有抑鬱(p < 0.05)。最普遍的自殘行為方法為服毒(91%)。超過一半的病人有中度自殺傾向。自殘行為與以下月經週期因素有顯著關係:濾泡期(p < 0.05)、較遲有第一次月經來潮(p < 0.05)、較短的月經天數(p < 0.05)。抑鬱症與月經週期無顯著關係(p > 0.05)。
結論:月經週期可能與自殘行為有顯著關係。建議進一步研究年輕女性的自殘行為與心理社會及生理因素的關係。
關鍵詞:月經週期、精神病患、經前綜合徵、企圖自殺
Introduction
The relationship between the menstrual cycle and psychiatric morbidity has long been recognised. Psychiatric disturbances, such as premenstrual syndrome, postpartum psychiatric disorders, and depression are known to be related to the menstrual cycle.1 Suicidal behaviour or deliberate self-harm (DSH) may also be influenced by the menstrual cycle, but the results of various studies are inconsistent, contradictory, and controversial. Several authors had specifically hypothesised that low oestrogen levels may contribute to suicide.2,3 While some concluded that there is no relationship between the menstrual cycle and suicidal behaviour,4-6 others believe exactly the opposite.7-9
Morris and Maniam10 did an extensive review of the literature pertaining to suicide and attempted suicide in Malaysia. Most studies were descriptive and based on uncontrolled observations. Important socio-demographic profiles associated with suicidal behaviour included ethnicity,11-15 method of suicide and help-seeking behaviour,14 gender, age, education, and rural-urban differences.16 There have been few controlled studies on suicide or DSH in Malaysia. Peng and Chin17 studied social problems and psychiatric disorders among parasuicide subjects. Maniam15 examined differentiating characteristics among 19 families with a history of suicidal behaviour and 21 control families. Recent studies investigated social support network, coping styles18 and personality factors.19
To our knowledge, there has been no study examining the association between the menstrual cycle and DSH in Malaysia. Therefore the aim of this study was to determine any such association, and any related factors.
Methods
This was a case-control study examining the association between patients with DSH and menstrual cycle among consecutive patients admitted for DSH and referred to psychiatric clinic of Hospital Kuala Lumpur (HKL) during a 4-month period (1 March 2005 to 30 June 2005).
Sampling Method and Data Collection
In Malaysia, all suicidal attempts are known to the police. All DSH patients seen in the Casualty Department are treated as police cases and admitted regardless of the severity of the attempt.20 After admission, they are referred to the Psychiatric Department of the respective hospital.
Subjects
The cases consisted of female DSH patients consecutively admitted to the HKL, and were identified from a daily check of the admission register of the relevant admitting wards. Referrals to the Psychiatry Clinic were also checked on a daily basis to confirm the recognition of DSH. Individuals who met the inclusion criteria were interviewed before discharge. The controls recruited in this study were female patients between the ages of 18 and 45 years admitted to the HKL following an acute illness. The admission registers of the relevant wards were scrutinised for the controls; most being admitted for acute fevers (uncomplicated dengue, pharyngitis, gastritis, acute gastroenteritis, and urinary infections).
Criteria for inclusion were: being female, aged 18 to 45 years, and admission to HKL during the study period. In addition, all the patients had to be medically fit to be interviewed, give informed consent, and experiencing regular menstrual periods. Patients were excluded if they had attained menopause, were in receipt of hormone replacement therapy, had self harmed accidentally, or had psychotic symptoms. The cases had to be admitted for DSH and referred to the Psychiatric Department. The sample size was calculated by using Epi-Info Version 3.2, 2004 software; 86 cases and 85 controls (n = 171) were recruited.
Definitions
Deliberate self-harm was defined as a non-fatal act in which an individual deliberately caused self-injury or knowingly ingested a substance in excess of any prescribed or generally recognised therapeutic dose or took a substance never intended for human consumption.21
Regular menstruation was defined as menstrual cycles lasting 28 (standard deviation [SD], 6) days in the last index cycles.22 In accordance with the literature, the menstrual cycle was subdivided into the follicular phase (days 1 - 11), mid-cyclic phase (days 12 - 16), and luteal phase (days 17 - 28±3). The follicular phase can be further divided into menstrual follicular phase (days 1 - 7) and non-menstrual follicular phase (days 8 - 11).23
A confiding relationship was defined as having someone whom one could trust and disclose one’s problem.
Assessment
Mini-International Neuropsychiatric Interview
The Mini-International Neuropsychiatric Interview (MINI) was designed as a brief structured interview for the major Axis I psychiatric disorders in the Diagnostic and Statistical Manual of Mental Disorders (4th ed) [DSM-IV] and International Classification of Diseases (10th revision).24 Validation and reliability studies have been performed to compare the MINI to the Structured Clinical Interview for DSM-IV Axis I Disorders for the DSM-III-R. The MINI had acceptably high validation and reliability scores and could be administered in a shorter period of time.
The interviewer was trained in the use of the MINI by a senior psychiatrist who had experience in using this instrument. The inter-rater reliability for this study was ascertained by randomly interviewing 10% of the cases. Calculation of reliability coefficients for a 2-point category scale revealed that both the senior psychiatrist and the interviewer had a kappa of 1.
Suicide Intent Scale
The Suicide Intent Scale was devised by Pierce in 197725 and relates closely to the original Beck’s Suicide Intent Scale. The former is a semi-structured interview instrument that requires no special training and is easy to administer.
Data Analysis
Data collected were analysed using the Statistical Package for the Social Sciences (Windows version 12.0; SPSS Inc, Chicago [IL], US). The relationships between study parameters were analysed using appropriate statistical tests. Exploratory Data Analysis was used to check for normality. This was to enable detection or identification of problems with the data, data screening and description. Independent sample t tests and Chi-square tests were used to determine significant differences between the cases and controls, with respect to demographic and other variables. The non- parametric Mann Whitney U test was performed on data which were not normally distributed. The 95% confidence interval (CI) was chosen as the level of significance (p = 0.05).
Ethical Considerations
This research project was approved by the Department of Psychiatry Ethical Research Committee of the Universiti Kebangsaan Malaysia, with permission from the head of the Department of Psychiatry and the Director of Hospital Kuala Lumpur. Before each interview, informed consent was obtained from the subject. The purpose of the study was explained, respondents were assured of confidentiality, and the voluntary nature of participation was explained. The data were then keyed into the SPSS computer program without names.
Results
Demographic Factors
A total of 174 patients were referred to the psychiatric departments or admitted to the psychiatric wards of HKL for self-poisoning or self-injurious behaviour during the study period. Of these patients, 32 (18%) were male. Six (3%) patients were older than 45 years and 18 (10%) were younger than 18 years. Five (3%) patients used hormonal contraceptives. Four (2%) patients had irregular menses, and one was pregnant. Two (1%) of the patients were too ill to be interviewed, and 1 did not consent to an interview. Four patients absconded from the medical wards before being interviewed, and 2 others discharged themselves against medical advice. Six (3%) patients took an overdose of painkiller because of severe headache (claiming they had no intent to harm themselves). Five (3%) claimed to have ingested a toxic substance accidentally. Two (1%) of the patients had a history of schizophrenia, and were excluded from the study as they had psychotic symptoms. Thus, from these 174 patients, 88 were excluded for various reasons.
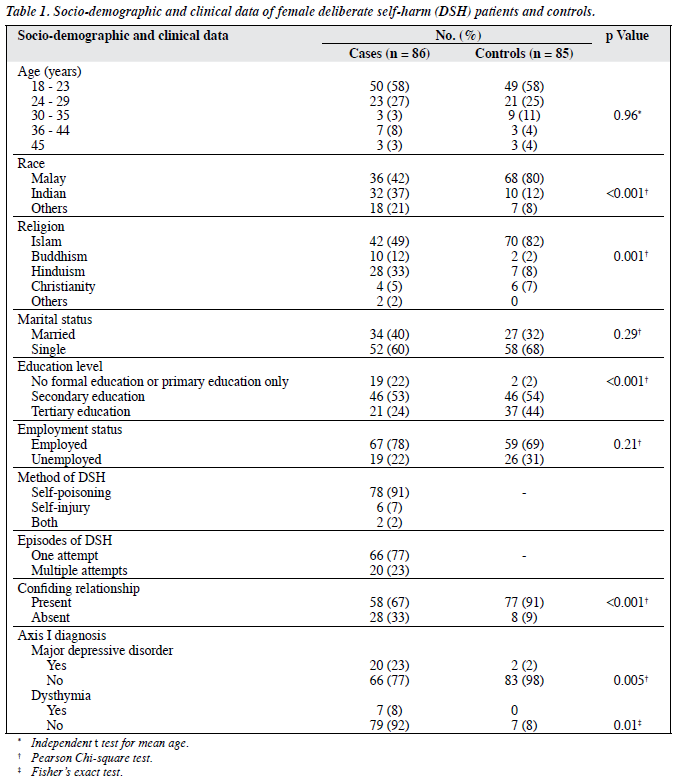
Most of the cases with DSH (58%) and the controls fell into the 18-to-23 years age-group; more than 90% being less than 30 years old. The mean age of the cases and controls were 25 (SD, 7) and 25 (SD, 6) years, respectively. Approximately 85% of the cases and 83% of the controls were in the age-group of 18-to-29 years (Table 1).
Race
Among the subjects with DSH, there was a slight preponderance of Malays (42%), followed by the Indians (37%). The Chinese represented a small proportion of the study population (14%). Other races (7%) included one patient from Iban, another from Bajau, 2 were Sikhs, and another 2 were Indonesian. There was a slight preponderance of Malays among subjects with DSH compared to controls with significant difference in the proportions (Pearson Chi- square = 26.205, df = 2, p < 0.05). There was a significant difference among races in terms of DSH. Using the Malay group as a reference, the odds ratio (OR) calculated for Indians was 6, and for all other groups it was 5.
Religion
The majority of subjects with DSH were Muslims (49%), followed closely by Hindus (33%); Buddhists accounted for 12% and Christians 5%.
Marital Status
There was a high proportion of single patients with DSH. Approximately 58% (n = 50) had never been married, 1 (1%) was divorced, and 1 (1%) was widowed. The remaining 40% (n = 34) were married (Pearson Chi-square = 1.13, df = 1, p > 0.05). Chi-square analysis comparing marital status among the DSH patients and controls yielded no significant difference (OR = 1.4; 95% CI, 0.75-2.63; p > 0.05).
Education Level
Half of the cases were educated up to secondary level (53%, n = 46). Approximately 24% (n = 21) had received tertiary education (diploma/degree), 20% (n = 17) had had primary education, and 2% (n = 2) had not had formal schooling. Statistical analysis showed there was a significant difference between cases and controls (p < 0.05); the DSH subjects were more likely to have had lower levels of education than controls. Odds ratio calculated for the no-formal-education versus primary-education groups and the secondary- education with reference to the tertiary-education groups were 16.7 and 1.8, respectively.
Employment
A majority of the cases (78%, n = 67) were employed and 22% (n = 19) were not working. Analysis of employment status between cases and controls showed no significant difference (OR = 1.55; 95% CI, 0.78-3.09; p > 0.05).
Clinical Factors
The commonest method of DSH was an overdose of medication or ingestion of toxic substances such as insecticide, detergent, rat poison, or kerosene (91%, n = 78). Two subjects (2%) committed both self-poisoning and self-injury. Two others (2%) swallowed pieces of glass and slashed their wrist. For most subjects it was their first attempt at DSH (77%, n = 66) while the remaining 23% (n = 20) admitted to at least one previous attempt.
Confiding Relationship
Two-thirds of the DSH subjects (67%, n = 58) had confiding relationship with someone else and 33% (n = 28) had no such relationship, whilst for the controls 91% (n = 77) had confiding relationship and only 9% (n = 8) had no such relationship (Pearson Chi-square = 13.78, df = 1, p < 0.05). The analysis of the association of the presence of confiding relationship and DSH shows a significant difference between the cases and controls (p < 0.05; OR = 4.6; 95% CI, 1.97-10.94). Controls were 4.6 times more likely to have confiding relationship than DSH cases.
Family History of Mental Illness
More than three-quarters of the DSH subjects (90%, n = 77) had no family history of psychiatric illness. One had a family history of mood disorder, 2 of alcohol abuse, 2 of substance abuse, and 4 had a history of other psychiatric illnesses in their families. Other neuropsychiatric disorders included schizophrenia, mental retardation with psychosis (Pearson Chi-square = 2.52, df = 1, p > 0.05). The analysis of the association between family history of psychiatric illness among cases and controls showed no significant difference (OR = 1.73; 95% CI, 0.88-3.42; p > 0.05).
Suicide Intent among Cases
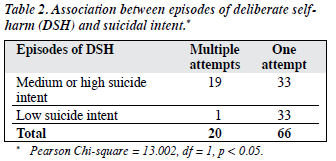
Approximately half of the patients (55%, n = 47) had medium suicide intent scores, while 40% (n = 34) had low scores and 6% (n= 5) had high scores. The analysis of the association between episodes of DSH and suicide intent showed a significant difference (p < 0.05); multiple attempters had higher suicide intent compared to first attempters (Table 2).
Psychiatric Diagnosis
Among DSH subjects, 23% (n = 20) had a diagnosis of major depression, 8% (n = 7) had dysthymia, 4% (n = 3) have panic disorder, 1% (n = 1) had agoraphobia, and 5% (n = 4) had co-morbid diagnoses. One was an alcohol abuser and another a substance abuser (of volatile material). Two had bulimia nervosa and one had a generalised anxiety disorder. Forty eight of the cases and 79 of the controls had no Axis I psychiatric diagnosis. The analysis of an association between major depressive disorder and DSH showed a significant difference between the cases and the controls (Pearson Chi-square = 16.66, df = 1, p < 0.05). The analysis of the association of dysthymia and DSH showed a significant difference between cases and controls (Fisher’s exact test, df = 1, p < 0.05) [Table 1].
Physiological Factors
Menstrual Factors
The mean age of menarche for the cases and controls was 13.3 (SD, 1.4) years and 12.8 (SD, 1.3) years, respectively; the difference being statistically significant (p < 0.05). The mean duration of menses among cases was 5.3 (SD, 1.4) days, while it was 5.8 (SD, 1.5) days among controls; the shorter duration of menses in DSH patients compared to controls was statistically significant (p < 0.05).
The mean duration of the menstrual cycle was 29 (SD, 1) days in cases and 29 (SD, 2) days in controls, there being no statistically significant differences (independent t test, p > 0.05).
Menstrual Cycle Phase among Cases
The numbers of DSH patients presenting during the follicular phase, mid-cyclic phase, and luteal phase were 55% (n = 47), 13% (n = 11), and 33% (n = 28), respectively (Table 3). The frequencies of DSH cases among the 3 phases of the menstrual cycle were significantly different; the 55% ensuing during the follicular phase was significantly greater than the expected value (Chi-square = 8.57, df = 2, p < 0.05). Almost 40% (n = 34) of DSH episodes occurred during the follicular phase, followed by 32% (n = 28) in the luteal phase. When the menstrual phases were divided into 4 phases, there was also a significant difference between the phases; there being 50% more DSH attempts during the follicular phase than expected theoretically (Chi-square = 10.72, df = 3, p < 0.05).
Table 4 is an analysis of clinical factors related to the 2 menstrual phases (follicular and non-follicular) among DSH patients. No clinical data (method and episode of DSH, confiding relationships, suicide intent, family history of psychiatric illness and depressive disorder) relating to DSH subjects attained a statistical significance difference (p > 0.05).
Discussion
In this study, the demographic profile of patients with DSH was comparable to that found in previous local studies12-14; more than two-thirds were aged less than 30 years, more than half were single, and less than 25% had received a tertiary education. There was a preponderance of Malays (almost 42%) and more than two-thirds were employed. Clinical data also mirrored results from previous studies,14,15,17 with respect to the preponderance of self-poisoning (91%), first episode of DSH (77%), and moderate suicidal intent (55%). Approximately 11% had a family history of psychiatric illness, 12% had a family history of suicide or DSH, and one-third had a depressive disorder.
The high rates of psychiatric morbidity associated with DSH in this study are consistent with the suggestion that such patients should be carefully screened for psychiatric symptoms.26 The diagnosis of adjustment disorder was not entertained however, since the MINI did not include this diagnosis. The prevalence of adjustment disorder is nevertheless expected to be fairly high.26,27 There was a high preponderance of DSH attempts during the follicular phase of the menstrual cycle (55%, n= 47), which is also consistent with other studies.2,23,28,29 There was also an association between more previous DSH attempts and medium-to- high suicidal intent. These findings are also consistent with findings from a previous study.23 Hindberg and Naesh30 suggested that plasma serotonin was at its lowest level at the onset of menstruation. It is also known that oestrogen and progesterone levels are lower in the follicular than in other phases of the menstrual cycle. Fourestié et al2 had hypothesised that low oestradiol production contributed to depression and attempted suicide. Low levels of oestrogens are associated with a decrease in brain serotonergic activity, which might well contribute to an increased risk of suicide.2,30
Clinical factors such as methods and episodes of DSH, confiding relationships, family history of psychiatric illness and suicidal intent, however, did not yield any significant association with phases of the menstrual cycle. Also there was no association of depressive disorders and menstrual cycle phases, possibly due to our small sample size. A larger sample was probably needed to assess any association of depressive disorders with the menstrual cycle.
As this was a case-control study, it was also prone to many types of bias and confounding factors. The information on suicidal intent and the last normal menstrual period was obtained retrospectively. Many researchers believe that untrained women may not provide reliable information about their menstrual cycles.31 Ideally, repeated hormonal assessment would have provided a gold standard for establishing the phase of the menstrual cycle. However, due to limited time and financial constraints, this was not undertaken. Our choice of controls was also biased. Ideal controls would have come from the same locality, and same population as the DSH subjects, and from the same socio-economic background. Several confounders were not measured, which included important factors such as life events and premorbid personality of the subjects. Life events are closely correlated with the timing of DSH.17 The assessor was not blinded, which may have led to bias. To overcome this shortcoming, inter-rater reliability was determined and the agreement (kappa value) was good. The other cofounder was that patients with a history of irregular menstrual cycles were excluded. However, those with irregular menstrual cycles were possibly more prone to stress.
There was a significant association between DSH and the age of menarche, the duration of menses, as well as the (follicular) phase of the menstrual cycle, which could all be critical risk factors. A prospective study involving a larger sample size may be able to explore such associations and would be of even greater interest if coupled with biochemical and hormonal investigations to test the hypothetical relationship between menstrual cycle phases and neuro-endocrine function.
In conclusion, based on this preliminary study, there is a need to recognise that information gleaned from the menstrual history may reveal determinants of subsequent psychiatric sequelae. Such a study might help clinicians identify sub-populations of women that should be more closely monitored for the development of psychiatric disturbances, particularly DSH and suicidal behaviour.
Acknowledgements
The authors would like to thank the Director of Hospital Kuala Lumpur, all its doctors and staff as well as the patients who cooperated with the conduct of this study.
References
- Rubinow DR, Schmidt PJ, Roca CA. Estrogen-serotonin interactions: implications for affective regulation. Biol Psychiatry 1998;44:839-50.
- Fourestié V, de Lignières B, Roudot-Thoraval F, Fulli-Lemaire I, Cremniter D, Nahoul K, et al. Suicide attempts in hypo-oestrogenic phases of the menstrual cycle. Lancet 1986;2:1357-60.
- Mann JJ. The neurobiology of suicide. Nat Med 1998;4:25-30.
- Ekeberg O, Jacobsen D, Sorum Y, Aass G. Self-poisoning and the menstrual cycle. Acta Psychiatr Scand 1986;73:239-41.
- Luggin R, Bernsted B, Petersson B, Jacobsen AT. Acute psychiatric admission related to the menstrual cycle. Acta Psychiatr Scand 1984;69:461-5.
- Holding TA, Minkoff K. Parasuicide and the menstrual cycle. J Psychosom Res 1973;17:365-8.
- Glass GS, Heninger GR, Lansky M, Talan K. Psychiatric emergency related to the menstrual cycle. Am J Psychiatry 1971;128:705-11.
- Tonks CM, Rack PH, Rose MJ. Attempted suicide and the menstrual cycle. J Psychosom Res 1968;11:319-23.
- Dalton K. Menstruation and acute psychiatric illness. Br Med J 1959;1:148-9.
- Morris P, Maniam T. Ethnicity and suicidal behaviour in Malaysia: a review of the literature. Transcult Psychiatry 2001;38:51-63.
- Haq SM, Buhrich N. Parasuicides and their determinants in a multiracial society. Singapore Med J 1980;21:648-51.
- Orr JW, Pu TN. Parasuicides in Kuala Lumpur. A descriptive study. Singapore Med J 1985;26:161-70.
- Ong S, Yeoh KL. Suicidal behaviour in Kuala Lumpur. In: Kok LP, Tseng W, editors. Suicidal behaviour in the Asia Pacific region. Singapore: Singapore University Press; 1992:144-75.
- Habil MH, Ganesvaran T, Agnes LS. Attempted suicide in Kuala Lumpur. Asia Pac J Public Health 1992-1993;6:5-7.
- Maniam T. Changing patterns of suicides in Cameron Highlands. Malaysian Journal of Psychiatry 1994;2:48-58.
- Simons RC, Sarbadhikary D. Suicide attempters admitted to the University of Malaya Medical Center Psychiatric Unit. Int J Soc Psychiatry 1972;18:97-103.
- Peng R, Chin CN. Social problems and psychiatric disorder in parasuicide: a controlled study. Malaysian Journal of Psychiatry 1997;5:55-62.
- Azhar S. Coping styles and social support networks among patients admitted for deliberate self harm – a case control study [dissertation]. Malaysia: Universiti Kebangsaan Malaysia; 2002.
- Hamidin A. A case control study on personality traits in deliberate self harm [dissertation]. Malaysia: Universiti Kebangsaan Malaysia; 2005.
- Chia PY. Depression and suicide intent in parasuicide patients [dissertation]. Malaysia: Universiti Kebangsaan Malaysia; 1989.
- Hawton K, Harriss L, Hall S, Simkin S, Bale E, Bond A. Deliberate self- harm in Oxford, 1990-2000: a time of change in patient characteristics. Psychol Med 2003;33:987-95.
- Bancroft J. The menstrual cycle and the well being of women. Soc Sci Med 1995;41:785-91.
- Baca-García E, Díaz-Sastre C, de Leon J, Saiz-Ruiz J. The relationship between menstrual cycle phases and suicide attempts. Psychosom Med 2000;62:50-60.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59(Suppl 20):S22-33.
- Pierce DW. The predictive validation of a suicide intent scale: a five year follow-up. Br J Psychiatry 1981;139:391-6.
- Haw C, Hawton K, Houston K, Townsend E. Psychiatric and personality disorders in deliberate self-harm patients. Br J Psychiatry 2001;178:48-54.
- Suominen K, Henriksson M, Suokas J, Isometsä E, Ostamo A, Lönnqvist J. Mental disorders and comorbidity in attempted suicide. Acta Psychiatr Scand 1996;94:234-40.
- Cayköylü A, Capoglu I, Oztürk I. The possible factors affecting suicide attempts in the different phases of the menstrual cycle. Psychiatry Clin Neurosci 2004;58:460-4.
- Gisselmann A, Ait Ameur A, Pinoit JM, François I, Trapet P. Attempted suicide and menstrual cycle. An epidemiologic study [in French]. Ann Med Psychol (Paris) 1996;154:136-9.
- Hindberg I, Naesh O. Serotonin concentrations in plasma and variations during the menstrual cycle. Clin Chem 1992;38:2087-9.
- Shortridge LA. Assessment of menstrual variations in working populations. Reprod Toxicol 1988;2:171-6.